Acute Lower Gastrointestinal Bleeding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -

Safety of Heparin Bridging Therapy for Transrectal Ultrasound-Guided Prostate Biopsy in Patients Requiring Temporary Discontinua
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Hamano et al. SpringerPlus (2016) 5:1917 DOI 10.1186/s40064-016-3610-6 RESEARCH Open Access Safety of heparin bridging therapy for transrectal ultrasound‑guided prostate biopsy in patients requiring temporary discontinuation of antithrombotic agents Itsuto Hamano1, Shingo Hatakeyama1* , Tohru Yoneyama2, Yuki Tobisawa1, Osamu Soma1, Teppei Matsumoto1, Hayato Yamamoto1, Atsushi Imai2, Takahiro Yoneyama2, Yasuhiro Hashimoto2, Takuya Koie1 and Chikara Ohyama1,2 Abstract Background: Safety of heparin bridging therapy for transrectal ultrasound-guided prostate (TRUS) biopsy in patients requiring temporary discontinuation of antithrombotic therapy is unknown. This study aimed to assess the relation- ship between heparin bridging therapy and the incidence of complications after TRUS biopsy. Methods: From January 2005 to November 2015, we performed 1307 consecutive TRUS biopsies on 1134 patients in our hospital. The patients were assigned to two groups: those without heparin bridging (the control group) and those with temporary discontinuation of antithrombotic agents with heparin bridging therapy (the bridging group). A 10–12-core TRUS biopsy was performed; the patients were evaluated for bleeding-related complications. Results: Of 1134 patients, 1109 (1281 biopsies) and 25 (26 biopsies) were assigned to the control and bridging group, respectively. Patient background did not significantly differ between the control and bridging groups, except for age, history of diabetes, cardiovascular diseases, and CHADS2 scores. Compared with the control group, the bridg- ing group showed a significantly higher rate of complication for any complication (35 vs. 8.3%, P < 0.001), bleeding- related complications (27 vs. -

Predictive Score for Positive Upper Endoscopies Outcomes in Children with Upper Gastrointestinal Bleeding. Score Prédictif De L
Predictive score for positive upper endoscopies outcomes in children with upper gastrointestinal bleeding. score prédictif de la présence de lésions endoscopiques dans l’hémorragie digestive haute de l’enfant Sonia Mazigh 1, Rania Ben Rabeh 1, Salem Yahiaoui 1, Béchir Zouari 2, Samir Boukthir 1, Azza Sammoud 1 1- Service de médecine C Hôpital d'enfants Béchir Hamza de Tunis- Université de Tunis El Manar, Faculté de Médecine de Tunis 2- Département d'épidémiologie et de médecine préventive - Université Tunis El Manar, Faculté de Médecine de Tunis, résumé summary Prérequis: L'hémorragie digestive haute (HDH) est une urgence Background: Upper gastrointestinal bleeding (UGIB) is a common fréquente en pédiatrie. L'endoscopie digestive haute (EDH) est pediatric emergency. Esophago-gastro-duodenoscopy (EGD) is the l'examen de choix pour identifier l’origine du saignement. first line diagnostic procedure to identify the source of bleeding. Néanmoins l’étiologie demeure inconnue dans 20% des cas. En However etiology of UGIB remains unknown in 20% of cases. outre, l'endoscopie d'urgence n'est pas disponible dans de Furthermore, emergency endoscopy is unavailable in many hospitals nombreux hôpitaux dans notre pays . in our country. Objectifs: Décrire les lésions endoscopiques retrouvées chez Aims: Identify clinical predictors of positive upper endoscopy l'enfant dans l'HDH, identifier les facteurs prédictifs de la présence outcomes and develop a clinical prediction rule from these de ces lésions et élaborer un score clinique à partir de ces parameters. paramètres. Methods: Retrospective study of EGDs performed in children with Méthodes: Etude rétrospective des EDH réalisées chez les enfants first episode of UGIB, in the endoscopic unit of Children's Hospital of présentant un premier épisode d'HDH, à l'unité d'endoscopie Tunis, during a period of six years. -

Lower Gastrointestinal Tract
Lower Gastrointestinal Tract Hemorrhoids—Office Management and Review for Gastroenterologists Mitchel Guttenplan, MD, FACS 1 and Robert A Ganz, MD, FASGE 2 1. Medical Director, CRH Medical Corp; 2. Minnesota Gastroenterology, Chief of Gastroenterology, Abbott-Northwestern Hospital, Associate Professor of Medicine, University of Minnesota Abstract symptomatic hemorrhoids and anal fissures are very common problems. This article provides a review of the anatomy and physiology of the anorectum along with a discussion of the diagnosis and treatment of hemorrhoids and the commonly associated matters of anal sphincter spasm and fissures. The various office treatment modalities for hemorrhoids are discussed, as are the specifics of rubber band ligation (rBL), and a strategy for the office treatment of these problems by the gastroenterologist is given. The crh o’regan system™ is a technology available to the gastroenterologist that provides a safe, effective, and efficient option for the non-surgical treatment of hemorrhoids in the office setting. Keywords hemorrhoids, anal fissure, rubber band ligation, crh o’regan system™ Disclosure: Mitchel guttenplan is Medical Director of crh Medical Products corporation, the manufacturer of the crh o’regan system™. robert A ganz is a consultant to and holds equity in crh Medical Products corporation. Received: 2 november 2011 Accepted: 30 november 2011 Citation: Touchgastroentorology.com ; December, 2011. Correspondence: Mitchel guttenplan, MD, fAcs, 3000 old Alabama rd, suite 119 #183, Alpharetta, gA 30022-8555, us. e: [email protected] Diseases of the anorectum, including hemorrhoids and anal fissures, are experience also makes it clear that hemorrhoid sufferers frequently very common. The care of these entities is typically left to general and have additional anorectal issues that may both confuse the diagnosis colorectal surgeons. -

Colorectal Cancer Health Services Research Study Protocol: the CCR-CARESS Observational Prospective Cohort Project José M
Quintana et al. BMC Cancer (2016) 16:435 DOI 10.1186/s12885-016-2475-y STUDYPROTOCOL Open Access Colorectal cancer health services research study protocol: the CCR-CARESS observational prospective cohort project José M. Quintana1,8* , Nerea Gonzalez1,8, Ane Anton-Ladislao1,8, Maximino Redondo2,8, Marisa Bare3,8, Nerea Fernandez de Larrea4,8, Eduardo Briones5, Antonio Escobar6,8, Cristina Sarasqueta7,8, Susana Garcia-Gutierrez1,8, Urko Aguirre1,8 and for the REDISSEC-CARESS/CCR group Abstract Background: Colorectal cancers are one of the most common forms of malignancy worldwide. But two significant areas of research less studied deserve attention: health services use and development of patient stratification risk tools for these patients. Methods: Design: a prospective multicenter cohort study with a follow up period of up to 5 years after surgical intervention. Participant centers: 22 hospitals representing six autonomous communities of Spain. Participants/Study population: Patients diagnosed with colorectal cancer that have undergone surgical intervention and have consented to participate in the study between June 2010 and December 2012. Variables collected include pre-intervention background, sociodemographic parameters, hospital admission records, biological and clinical parameters, treatment information, and outcomes up to 5 years after surgical intervention. Patients completed the following questionnaires prior to surgery and in the follow up period: EuroQol-5D, EORTC QLQ-C30 (The European Organization for Research and Treatment of Cancer quality of life questionnaire) and QLQ-CR29 (module for colorectal cancer), the Duke Functional Social Support Questionnaire, the Hospital Anxiety and Depression Scale, and the Barthel Index. The main endpoints of the study are mortality, tumor recurrence, major complications, readmissions, and changes in health-related quality of life at 30 days and at 1, 2, 3 and 5 years after surgical intervention. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -
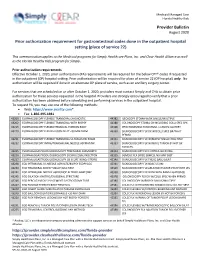
Provider Bulletin Prior Authorization Requirement for Gastrointestinal
Medicaid Managed Care Florida Healthy Kids Provider Bulletin August 2020 Prior authorization requirement for gastrointestinal codes done in the outpatient hospital setting (place of service 22) This communication applies to the Medicaid programs for Simply Healthcare Plans, Inc. and Clear Health Alliance as well as the Florida Healthy Kids program for Simply. Prior authorization requirements Effective October 1, 2020, prior authorization (PA) requirements will be required for the below CPT® codes if requested in the outpatient (OP) hospital setting. Prior authorization will be required for place of service 22 (OP hospital) only. No authorization will be required if done in an alternate OP place of service, such as an ancillary surgery center. For services that are scheduled on or after October 1, 2020, providers must contact Simply and CHA to obtain prior authorization for these services requested in the hospital. Providers are strongly encouraged to verify that a prior authorization has been obtained before scheduling and performing services in the outpatient hospital. To request PA, you may use one of the following methods: Web: https://www.availity.com* Fax: 1-866-495-1981 43200 ESOPHAGOSCOPY FLEXIBLE TRANSORAL DIAGNOSTIC 44382 ILEOSCOPY STOMA W/BX SINGLE/MULTIPLE 43202 ESOPHAGOSCOPY FLEXIBLE TRANSORAL WITH BIOPSY 44388 COLONOSCOPY STOMA DX INCLUDING COLLJ SPEC SPX 43215 ESOPHAGOSCOPY FLEXIBLE REMOVAL FOREIGN BODY 45308 PROCTOSGMDSC RIGID RMVL 1 LESION CAUTERY 43220 ESOPHAGOSCOPY FLEX BALLOON DILAT <30 MM DIAM 45330 SIGMOIDOSCOPY -

APG Regulations
FINAL as of 8/22/08 Pursuant to the authority vested in the Commissioner of Health by Section 2807(2-a) of the Public Health Law, Part 86 of Title 10 of the Official Compilation of Codes, Rules and Regulations of the State of New York, is amended by adding a new Subpart 86-8, to be effective upon filing with the Secretary of State, to read as follows: SUBPART 86-8 OUTPATIENT SERVICES: AMBULATORY PATIENT GROUP (Statutory authority: Public Health Law § 2807(2-a)(e)) Sec. 86-8.1 Scope 86-8.2 Definitions 86-8.3 Record keeping, reports and audits 86-8.4 Capital reimbursement 86-8.5 Administrative rate appeals 86-8.6 Rates for new facilities during the transition period 86-8.7 APGs and relative weights 86-8.8 Base rates 86-8.9 Diagnostic coding and rate computation 86-8.10 Exclusions from payment 86-8.11 System updating 86-8.12 Payments for extended hours of operation § 86-8.1 Scope (a) This Subpart shall govern Medicaid rates of payments for ambulatory care services provided in the following categories of facilities for the following periods: (1) outpatient services provided by general hospitals on and after December 1, 2008; (2) emergency department services provided by general hospitals on and after January 1, 2009; (3) ambulatory surgery services provided by general hospitals on and after December 1, 2008; (4) ambulatory services provided by diagnostic and treatment centers on and after March 1, 2009; and (5) ambulatory surgery services provided by free-standing ambulatory surgery centers on and after March 1, 2009. -
Cals Provider Manual the First 30 Minutes Edition 15 2019
COMPREHENSIVE ADVANCED LIFE SUPPORT CALS PROVIDER MANUAL THE FIRST 30 MINUTES EDITION 15 2019 DIRECTOR: DARRELL CARTER, MD EDUCATION MANAGER: Ann Gihl, RN Comprehensive Advanced Life Support © January 2019 All Rights Reserved www.calsprogram.org NOTE TO USERS The CALS course was developed for rural and other healthcare providers who work in an environment with limited resources, but who are also responsible for the emergency care in their often geographically isolated communities. Based on needs assessment and ongoing provider participant feedback, the CALS course endorses practical evaluation and treatment recommendations that reflect broad consensus and time-tested approaches. The organization of the CALS Provider Manual reflects the CALS Universal Approach. The FIRST THIRTY MINUTES (previously known as Volume 1) of patient care. ACUTE CARE ALGORITHMS/ TREATMENT PLANS/AND ACRONYMS provide critical care tools and are designed for quick access. The STEPS describe a system to diagnose and treat emergent patients. The FOCUSED CLINICAL PATHWAYS provide a brief review of most conditions encountered in the emergency setting. Supplement to the First Thirty Minutes (previously known as Volume 2) is composed of RESUSCITATION PROCEDURES divided into appropriate areas of clinical expertise, which illustrate hands-on techniques. Reference material for the First thirty Minutes (previously known as Volume 3) is composed of DIAGNOSIS, TREATMENT, AND TRANSITION TO DEFINITIVE CARE PORTALS, is also divided into appropriate areas of clinical expertise. In conjunction with the FOCUSED CLINICAL PATHWAYS, these detail further specialized guidelines on many conditions. Recommendations in the CALS course manual are aligned with those from organizations such as the American Heart Association, American College of Surgeons, American Academy of Family Physicians, American College of Emergency Physicians, American Academy of Neurology, American College of Obstetricians and Gynecologists, American Academy of Pediatrics, National Institutes of Health, and Centers for Disease Control. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

The Cutting Edge Fall 2008
DOSNL-FALL08b 11/12/08 9:46 PM Page 1 At the Cutting Edge of Surgical Excellence t is my great pleasure to introduce department has taken a leading role in the Ithe first issue of At the Cutting Edge application to general surgery of robotic — newsletter for the Department of technologies, already widely used in urology Surgery at the University of Illinois at and gynecology. Currently a true revolution Chicago. As the new Head of the is taking place at UIC. Complex procedures Department of Surgery, I am partic- such as hepatectomy, Whipple’s, lung resec- ularly proud to share with you the tion, mediastinal tumor excision, and gastric recent achievements of our surgical staff. The resection are routinely done in a minimally department has some of the most talented invasive fashion thanks to the genius of surgeons in the country, in line with a Professor Giulianotti and the most advanced remarkable tradition of excellence. robotic technology. The opening of the The Department of Surgery at the “Advanced Robotic Training Center” will University of Illinois was brought to the fore- allow Professor Giulianotti and his team to front by Warren H. Cole, who was the contribute to the robotic training of other Department Head between 1936 and 1966. faculties and our surgical residents. An In those years, the Department of Surgery impressive number of surgical leaders from was ranked within the top five in the country. the USA, Europe and Asia are currently com- His successor was Lloyd M. Nyhus, Head of ing to Chicago to learn from the best in the Department of Surgery from 1967 to robotic surgery.