High Resolution Anoscopy Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 1 Table 2 Table 3 Table 4 Colonoscopy-Related Costs
Digestive Health Network, Inc. List of Tables Top 10 Physician Specialties Performing Colonoscopies, Medicare Fee-for- Table 1 Service, 2015 Colonoscopy-related Costs, Medicare Fee-for-Service Beneficiaries who Table 2 Received a Screening or Diagnostic Colonoscopy, 2015 Colonoscopy-related Costs, Medicare Fee-for-Service Beneficiaries who Table 3 Received a Colonoscopy in an Ambulatory Surgical Center (ASC), Hospital Outpatient Department, or Physician Office, 2015 Proportion of Medicare Fee-for-Service Medicare Beneficiaries who Received Table 4 a Colonoscopy and were Treated in the Emergency Department within 7 Days of the procedure, 2015 Digestive Health Network, Inc. Responses to Questions Among Medicare beneficiaries, how many colonoscopies are performed in the US, by type of Q1 physician? Nearly 2 million screening and diagnostic colonoscopies were performed in 2015. Of these, over 78% were performed by a gastroenterologist. Nearly 10% were performed by a general surgeon and about 6% were performed by an internal medicine specialist. These results are shown in Table 1. Q2 What proportion of spending on colonoscopies is accounted for by physician services? In 2015, Medicare expenditures associated with colonoscopies totaled over $1.3 billion. (This excludes anesthesiology, pathology, radiology, and other costs identified in Table 2.) Approximately 31% of this amount, or $416 million was associated with professional fees. Q3 What share of Part B Medicare spending is accounted for by colonoscopies? Medicare Part B expenditures in 2015 totaled over $131 billion (data not shown). Colonoscopy costs accounted for approximately 1.03% of this total. Q4 What are the costs associated with colonoscopies for the different settings of care? Costs associated with colonoscopies in ambulatory surgical centers (ASC), hospital outpatient departments (HOPD), and physician offices are shown in Table 3. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

Combined Endo-Laparoscopic Surgery for Difficult Benign Colorectal Polyps
485 Review Article (Current Strategies in Colon Cancer Management) Combined endo-laparoscopic surgery for difficult benign colorectal polyps Zhong-Hui Liu1, Li Jiang1, Fion Siu-Yin Chan1,2, Michael Ka-Wah Li3, Joe King-Man Fan1,2,3 1Department of Surgery, The University of Hong Kong-Shenzhen Hospital, Shenzhen 518053, China; 2Department of Surgery, The University of Hong Kong, Hong Kong, China; 3Asia-Pacific Endo-Lap Surgery Group (APELS), Hong Kong, China Contributions: (I) Conception and design: JKM Fan, MKW Li; (II) Administrative support: MKW Li; (III) Provision of study materials or patients: FSY Chan; (IV) Collection and assembly of data: ZH Liu, L Jiang; (V) Data analysis and interpretation: ZH Liu; FSY Chan; JKM Fan; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Joe King-Man Fan, MBBS (HK), MS (HKU), FRCSEd, FACS. Department of Surgery, The University of Hong Kong-Shenzhen Hospital, Shenzhen 518053, China. Email: [email protected]. Abstract: Prevention of colorectal cancer (CRC) depends largely on the detection and removal of colorectal polyps. Despite the advances in endoscopic techniques, there are still a subgroup of polyps that cannot be treated purely by endoscopic approach, which comprise of about 10–15% of all the polyps. These so-called “difficult colorectal polyps” are polyps with large size, morphology, at difficult location, scarring or due to recurrence, which have historically been managed by surgical segmental resection. In treating benign difficult colorectal polyps, we have to balance the operative risks and morbidities associated with surgical segmental resection. Therefore, combined endoscopic and laparoscopic surgery (CELS) has been developed to remove this subgroup of difficult benign polyps. -

Lower Gastrointestinal Tract
Lower Gastrointestinal Tract Hemorrhoids—Office Management and Review for Gastroenterologists Mitchel Guttenplan, MD, FACS 1 and Robert A Ganz, MD, FASGE 2 1. Medical Director, CRH Medical Corp; 2. Minnesota Gastroenterology, Chief of Gastroenterology, Abbott-Northwestern Hospital, Associate Professor of Medicine, University of Minnesota Abstract symptomatic hemorrhoids and anal fissures are very common problems. This article provides a review of the anatomy and physiology of the anorectum along with a discussion of the diagnosis and treatment of hemorrhoids and the commonly associated matters of anal sphincter spasm and fissures. The various office treatment modalities for hemorrhoids are discussed, as are the specifics of rubber band ligation (rBL), and a strategy for the office treatment of these problems by the gastroenterologist is given. The crh o’regan system™ is a technology available to the gastroenterologist that provides a safe, effective, and efficient option for the non-surgical treatment of hemorrhoids in the office setting. Keywords hemorrhoids, anal fissure, rubber band ligation, crh o’regan system™ Disclosure: Mitchel guttenplan is Medical Director of crh Medical Products corporation, the manufacturer of the crh o’regan system™. robert A ganz is a consultant to and holds equity in crh Medical Products corporation. Received: 2 november 2011 Accepted: 30 november 2011 Citation: Touchgastroentorology.com ; December, 2011. Correspondence: Mitchel guttenplan, MD, fAcs, 3000 old Alabama rd, suite 119 #183, Alpharetta, gA 30022-8555, us. e: [email protected] Diseases of the anorectum, including hemorrhoids and anal fissures, are experience also makes it clear that hemorrhoid sufferers frequently very common. The care of these entities is typically left to general and have additional anorectal issues that may both confuse the diagnosis colorectal surgeons. -

Hybrid Procedure Offers a Less Invasive Alternative to Colectomy
The better way to get better Hybrid procedure offers a less invasive alternative to colectomy Insufflation gas provides important advantage The colonoscopy-laparoscopy procedure is made possible through the combined skills of the gastroenterologist and laparoscopic surgeon, and the use of CO2 rather than ambient air for insufflation — the introduction of gas into the colon to improve visibility. CO2 is more quickly absorbed by the gastrointestinal tract and results in less bowel distension, giving the laparoscopic surgeon a better field of vision within the abdominal cavity. © Copyright Olympus. Used with permission. “Some patients who would have required a bowel resection can instead benefit from this A new, minimally invasive procedure that is a hybrid of colonoscopy and less invasive procedure. We’re laparoscopy is proving to be a safe and effective alternative to open colectomy using this combined technique (removal of part of the colon) for patients with benign colon polyps that are as a way for patients to avoid colectomy,” explains James not removable endoscopically. Yoo, M.D., a colorectal surgeon Patients who undergo this hybrid procedure experience less pain and often go at UCLA. “This procedure home after only one or two days. Scarring and wound complications are minimal involves tiny incisions for the as the laparoscopic surgeon makes only small, keyhole incisions in the abdomen laparoscopic instruments and patients stay in the hospital only rather than the long incision characteristic of a traditional colectomy. a day or two.” WWW.UCLAHEALTH.ORG 1-800-UCLA-MD1 (1-800-825-2631) Who can benefit from the procedure? Participating When a routine colonoscopy reveals polyps, they are usually removed at the Physicians time of the procedure as a precaution against their progression to cancer. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Is Your Practice Ready for ICD-10?
Practice Management Is Your Practice Ready for ICD-10? Christopher Y Kim, MD, MBA, FASGE Kathleen A Mueller, RN, CPC, CGCS, CCS-P, CMSCS, PCS, CCC November 2013 The current version of diagnosis codes used in the United States since 1979 is formally known as the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Volumes 1 and 2. Volume 3 is also used in Hospitals to record inpatient procedures. The ICD was developed by the World Health Organization (WHO) and is maintained in the US by the National Center for Health and Vital Statistics (NCHS), with the Centers for Disease Prevention and Control (CDC), under the US Department of Health and Human Services (HHS). The Tenth Revision of ICD, also known as ICD-10-CM, will debut on October 1, 2014. Essentially overnight, the new codes will be required on services from that date going forward, and payers will no longer accept ICD-9 codes. Physician offices have just a little under a year to prepare for the transition to the ICD-10-CM diagnosis code sets. For years, HHS has been pushing to adopt the updated ICD-10 code standard that was endorsed by the WHO in 1990, and whose adoption was relatively swift in most of the world with the notable exception of the United States. Reasons given by HHS for adopting ICD-10 include: • ICD-9 is outdated with only a limited ability to accommodate new procedures and diagnoses. • ICD-9 lacks specificity and detail, uses terminology inconsistently, cannot capture new technology and lacks codes for preventive services; other alleged benefits: o ICD-10, with its increased specificity, will accurately label someone with the correct disease, sign/symptoms, or problem, as well as support the level of service provided. -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -
How to Prepare for Your Colonoscopy Using Miralax
PATIENT & CAREGIVER EDUCATION How to Prepare for Your Colonoscopy Using MiraLAX This information will help you prepare for your colonoscopy using polyethylene glycol (MiraLAX®) at Memorial Sloan Kettering (MSK). A colonoscopy is an exam of the entire colon (large intestine). Your doctor will use a flexible tube called a colonoscope to see the inside of your colon on a video monitor. During the procedure, your doctor can remove a small sample of tissue (biopsy) for testing, remove a polyp (growth of tissue), and take photos of the inside of your colon. Follow these instructions carefully. It is very important that your colon is empty for your colonoscopy. If there is stool inside your colon, your doctor may not be able to see polyps or other problems inside your colon and you may have to repeat the procedure. If you have any questions, contact your doctor's office. 1 Week Before Your Procedure Ask about your medications You may need to stop taking or change the dose of some of your medications before your procedure. We have included some common examples below. If you take medication to thin your blood, such as to treat blood clots or to prevent a heart attack or stroke, ask the doctor who prescribes it for you when to stop taking it. Some examples of blood thinners are warfarin (Coumadin®), dalteparin (Fragmin®), heparin, tinzaparin (Innohep®), enoxaparin (Lovenox®), clopidogrel (Plavix®), and cilostazol (Pletal®). There are others, so check with your doctor if you are not sure. If you take insulin or other medications for diabetes, you may need to change the dose. -

Utility of Abdominal Ultrasonography in the Diagnosis and Monitoring of Inflammatory Bowel Disease
1130-0108/2014/106/6/395-408 REVISTA ESPAÑOLA DE ENFERMEDADES DIGESTIVAS REV ESP ENFERM DIG (Madrid COPYRIGHT © 2014 ARÁN EDICIONES, S. L. Vol. 106, N.º 6, pp. 395-408, 2014 REVIEW Utility of abdominal ultrasonography in the diagnosis and monitoring of inflammatory bowel disease Joaquín Poza-Cordón1 and Tomás Ripollés-González2 1Department of Gastroenterology. Hospital Universitario La Paz. Madrid, Spain. 2Department of Radiology. Hospital Dr. Peset. Valencia, Spain ABSTRACT lished for examining the gastrointestinal tract, for three main reasons: Better technological development in other Abdominal ultrasonography has been undervalued for years as diagnostic techniques, a rejection by gastroenterologists technique used in examining the gastrointestinal tract. However, in the validity of its results, and the intestinal content it- thanks to the technological advances that have been seen in ultrasonography probes and the use of high frequency equipment, self, which has always been considered a limiting factor we are able to obtain high quality images of the intestinal wall. for exploration. However, in the last 20 years, it has been Moreover, due to the increased sensitivity of the colour Doppler, used with great diagnostic reliability to evaluate inflam- we can detect the parietal vascularization. Finally, in recent years, matory processes of the gastrointestinal tract (1-3) such as intravenous ultrasonography contrast agents have been used that infectious enterocolitis (4,5), diverticulitis (6-8), appendi- allow not only the inflammatory activity to be quantified but also the presence of complications with a diagnostic accuracy similar to citis (9) or ischemic colitis (10). Only in the last decade computed tomography (CT) and full magnetic resonance (full-RM), has it been accepted as a first-line technique in the diagno- without the associated radiation risk and at a lower cost. -
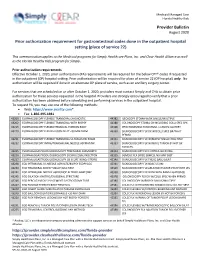
Provider Bulletin Prior Authorization Requirement for Gastrointestinal
Medicaid Managed Care Florida Healthy Kids Provider Bulletin August 2020 Prior authorization requirement for gastrointestinal codes done in the outpatient hospital setting (place of service 22) This communication applies to the Medicaid programs for Simply Healthcare Plans, Inc. and Clear Health Alliance as well as the Florida Healthy Kids program for Simply. Prior authorization requirements Effective October 1, 2020, prior authorization (PA) requirements will be required for the below CPT® codes if requested in the outpatient (OP) hospital setting. Prior authorization will be required for place of service 22 (OP hospital) only. No authorization will be required if done in an alternate OP place of service, such as an ancillary surgery center. For services that are scheduled on or after October 1, 2020, providers must contact Simply and CHA to obtain prior authorization for these services requested in the hospital. Providers are strongly encouraged to verify that a prior authorization has been obtained before scheduling and performing services in the outpatient hospital. To request PA, you may use one of the following methods: Web: https://www.availity.com* Fax: 1-866-495-1981 43200 ESOPHAGOSCOPY FLEXIBLE TRANSORAL DIAGNOSTIC 44382 ILEOSCOPY STOMA W/BX SINGLE/MULTIPLE 43202 ESOPHAGOSCOPY FLEXIBLE TRANSORAL WITH BIOPSY 44388 COLONOSCOPY STOMA DX INCLUDING COLLJ SPEC SPX 43215 ESOPHAGOSCOPY FLEXIBLE REMOVAL FOREIGN BODY 45308 PROCTOSGMDSC RIGID RMVL 1 LESION CAUTERY 43220 ESOPHAGOSCOPY FLEX BALLOON DILAT <30 MM DIAM 45330 SIGMOIDOSCOPY -

APG Regulations
FINAL as of 8/22/08 Pursuant to the authority vested in the Commissioner of Health by Section 2807(2-a) of the Public Health Law, Part 86 of Title 10 of the Official Compilation of Codes, Rules and Regulations of the State of New York, is amended by adding a new Subpart 86-8, to be effective upon filing with the Secretary of State, to read as follows: SUBPART 86-8 OUTPATIENT SERVICES: AMBULATORY PATIENT GROUP (Statutory authority: Public Health Law § 2807(2-a)(e)) Sec. 86-8.1 Scope 86-8.2 Definitions 86-8.3 Record keeping, reports and audits 86-8.4 Capital reimbursement 86-8.5 Administrative rate appeals 86-8.6 Rates for new facilities during the transition period 86-8.7 APGs and relative weights 86-8.8 Base rates 86-8.9 Diagnostic coding and rate computation 86-8.10 Exclusions from payment 86-8.11 System updating 86-8.12 Payments for extended hours of operation § 86-8.1 Scope (a) This Subpart shall govern Medicaid rates of payments for ambulatory care services provided in the following categories of facilities for the following periods: (1) outpatient services provided by general hospitals on and after December 1, 2008; (2) emergency department services provided by general hospitals on and after January 1, 2009; (3) ambulatory surgery services provided by general hospitals on and after December 1, 2008; (4) ambulatory services provided by diagnostic and treatment centers on and after March 1, 2009; and (5) ambulatory surgery services provided by free-standing ambulatory surgery centers on and after March 1, 2009.