Endoscopy Matrix
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Point of the Needle. Occult Pneumothorax: a Review P Gilligan, D Hegarty, T B Hassan
293 CASE REPORTS Emerg Med J: first published as 10.1136/emj.20.3.296 on 1 May 2003. Downloaded from The point of the needle. Occult pneumothorax: a review P Gilligan, D Hegarty, T B Hassan ............................................................................................................................. Emerg Med J 2003;20:293–296 maximal resonance, which was the left sixth intercostal space The case of a patient with an unusual medical condition in the anterior axillary line. Some 300 ml of air was aspirated and an occult pneumothorax is presented. The evidence from the left hemithorax and the patient clinically improved. for management of occult pneumothorax particularly in The chest radiograph revealed bilateral infiltrates and under- patients with underlying lung disease is reviewed and solu- lying cystic and bullous disease but failed to reveal evidence of tions to the acute clinical problems that may arise are a pneumothorax (fig 1). A chest radiograph performed after suggested. the needle decompression also failed to show a pneumotho- rax. Computed tomography (CT) of the thorax revealed an anterior pneumothorax (fig 2). This was drained under CT guidance by the placement of a chest drain catheter. 27 year old man with histiocytosis X presented to the During the patient’s in hospital stay his chest drain was emergency department with left posterior chest wall removed as his chest radiograph showed no evidence of Apain and marked dyspnoea. The patient previously had residual pneumothorax. The patient became markedly dysp- recurrent pneumothoraces, eight on the right and two on the noeic within 24 hours. Because of the clinical impression of left. He had undergone pleurodesis of the right lung. -
Practice Parameters for the Treatment of Patients with Dominantly Inherited Colorectal Cancer
Practice Parameters For The Treatment Of Patients With Dominantly Inherited Colorectal Cancer Diseases of the Colon & Rectum 2003;46(8):1001-1012 Prepared by: The Standards Task Force The American Society of Colon and Rectal Surgeons James Church, MD; Clifford Simmang, MD; On Behalf of the Collaborative Group of the Americas on Inherited Colorectal Cancer and the Standards Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons is dedicated to assuring high quality patient care by advancing the science, prevention, and management of disorders and diseases of the colon, rectum, and anus. The standards committee is composed of Society members who are chosen because they have demonstrated expertise in the specialty of colon and rectal surgery. This Committee was created in order to lead international efforts in defining quality care for conditions related to the colon, rectum, and anus. This is accompanied by developing Clinical Practice Guidelines based on the best available evidence. These guidelines are inclusive, and not prescriptive. Their purpose is to provide information on which decisions can be made, rather than dictate a specific form of treatment. These guidelines are intended for the use of all practitioners, health care workers, and patients who desire information about the management of the conditions addressed by the topics covered in these guidelines. Practice Parameters for the Treatment of Patients With Dominantly Inherited Colorectal Cancer Inherited colorectal cancer includes two main syndromes in which predisposition to the disease is based on a germline mutation that may be transmitted from parent to child. -

Endoscopy Rotation Coordination and Goals and Objects Department of Surgery Stanford School of Medicine (8/15/17, Jnl)
Endoscopy Rotation Coordination And Goals and Objects Department of Surgery Stanford School of Medicine (8/15/17, jnl) Rotation Director: James Lau, MD ATTENDINGS and CONTACT INFORMATION Cell Phone E-mail Address James Lau, MD (702) 306-8780 [email protected] Homero Rivas, MD MBA (972) 207-2381 [email protected] Dan Azagury, MD (650) 248-3173 [email protected] Shai Friedland, MD [email protected] Andrew Shelton, MD [email protected] Natalie Kirilcuk, MD [email protected] Cindy Kin, MD [email protected] Laren Becker, MD [email protected] Jennifer Pan, MD [email protected] Suzanne Matsui, MD [email protected] Ramsey Cheung, MD [email protected] KEYPOINT The key for this rotation is that you need to show initiative. TEXT Practical Gastrointestinal Endoscopy: The Fundamentals. Sixth Edition. By Peter B. Cotton, Christopher B. Williams, Robert H. Hawes and Brian P. Saunders. You are responsible for the material to enhance your understanding and supplement your past experiences. Lots of pictures and tips and tricks. Quick read. Copy of text available for purchase on Amazon.com or for check out from the Lane Library. Procedure Schedule Monday Tuesday Wednesday Thursday Friday Laren Becker Jennifer Pan Shelton/Kirilcuk/Kin Ramsey Suzanne (VA (VA Colonoscopy 8:00 am Cheung (VA Matsui (VA Livermore) Livermore) (Stanford Endoscopy) Livermore) Livermore) Every other Tuesday Rivas/Lau alternating Upper/Occasional Lower 1 Endoscopy 9a-1p (Stanford Endoscopy) Suzanne Matsui (VA Livermore) The Staff Drs. Becker, Cheung, Pan, and Matsui are gastroenterologists that perform 75% colonoscopies and 25% upper endoscopies at the Livermore location for the Palo Alto VA. -

Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St
Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St. Louis, Missouri LINDA DECKERT, MA, CCC-SLP, Special School District of St. Louis County, Town & Country, Missouri Vocal cord dysfunction involves inappropriate vocal cord motion that produces partial airway obstruction. Patients may present with respiratory distress that is often mistakenly diagnosed as asthma. Exercise, psychological conditions, airborne irritants, rhinosinusitis, gastroesophageal reflux disease, or use of certain medications may trigger vocal cord dysfunction. The differential diagnosis includes asthma, angioedema, vocal cord tumors, and vocal cord paralysis. Pulmo- nary function testing with a flow-volume loop and flexible laryngoscopy are valuable diagnostic tests for confirming vocal cord dysfunction. Treatment of acute episodes includes reassurance, breathing instruction, and use of a helium and oxygen mixture (heliox). Long-term manage- ment strategies include treatment for symptom triggers and speech therapy. (Am Fam Physician. 2010;81(2):156-159, 160. Copyright © 2010 American Academy of Family Physicians.) ▲ Patient information: ocal cord dysfunction is a syn- been previously diagnosed with asthma.8 A handout on vocal cord drome in which inappropriate Most patients with vocal cord dysfunction dysfunction, written by the authors of this article, is vocal cord motion produces par- have intermittent and relatively mild symp- provided on page 160. tial airway obstruction, leading toms, although some patients may have pro- toV subjective respiratory distress. When a per- longed and severe symptoms. son breathes normally, the vocal cords move Laryngospasm, a subtype of vocal cord away from the midline during inspiration and dysfunction, is a brief involuntary spasm of only slightly toward the midline during expi- the vocal cords that often produces aphonia ration.1 However, in patients with vocal cord and acute respiratory distress. -
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019 Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2018 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. TABLE OF CONTENTS FOR NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL FOR MEDICARE SERVICES Introduction Introduction Intro-3 Purpose Intro-3 Policy Manual Background Intro-6 Edit Development and Review Process Intro-7 Sources of Information about NCCI and MUE Intro-9 Correspondence to CMS about NCCI and its Contents Intro-10 Chapter I - General Correct Coding Policies List of Acronyms I-3 A. Introduction I-5 B. Coding Based on Standards of Medical/Surgical I-9 Practice C. Medical/Surgical Package I-12 D. Evaluation and Management (E&M) Services I-17 E. Modifiers and Modifier Indicators I-19 F. Standard Preparation/Monitoring Services for I-27 Anesthesia G. Anesthesia Service Included in the Surgical Procedure I-27 H. HCPCS/CPT Procedure Code Definition I-28 I. CPT Manual and CMS Coding Manual Instructions I-29 J. CPT “Separate Procedure” Definition I-30 K. Family of Codes I-30 L. -

Middle Nasal Valve Collapse: a Way to Resolve
Journal of Otolaryngology-ENT Research Case Report Open Access Middle nasal valve collapse: a way to resolve Abstract Volume 10 Issue 3 - 2018 Middle nasal valve collapse is a partial or complete collapsing of soft structures of Dunja Milicic,1 Carolina Serodio2 nasal pyramid, due to negative intranasal pressures resulting in complete anterior nasal 1 obstruction of air-flow. Even though is relatively common, it is often misdiagnosed or Hospital da Luz Arrabida, Department of Otorhinolaryngology, Portugal neglected in diagnosis. There are too many suggestions of surgical resolution of the 2Hospital da Luz Póvoa de Varzim, Department of problem, giving an idea that all of them are actually only partially or insufficiently Otorhinolaryngology, Portugal resolving the problem. In this paper a possible solution of middle nasal vault collapse was presented. A Correspondence: Dunja Milicic, Hospital da Luz Arrábida, triangle cartilage grafting with respecting of anatomical and functional principles was Praceta de Henrique Moreira 150, 4400-346 Vila Nova de Gaia, Portugal, Tel +351-22 377-6800, suggested. An open rhinoplasty approach by its large exposure was, in our hands, the Email [email protected] election method for resolving the problem. Received: February 01, 2018 | Published: May 21, 2018 Keywords: nasal valve collapse, triangular cartilage, graft, open rhinoplasty Introduction the nostril (lateral alar crura) is usually annoying the patients, by its hardness and cosmetic deformity, even though some authors minimize Collapse -

Thoracoscopy for Spontaneous Pneumothorax
Journal of Clinical Medicine Review Thoracoscopy for Spontaneous Pneumothorax José M. Porcel 1,2,3,* and Pyng Lee 4 1 Pleural Medicine Unit, Department of Internal Medicine, Hospital Universitari Arnau de Vilanova, 25198 Lleida, Spain 2 Institut de Recerca Biomèdica de Lleida Fundació Dr. Pifarré, IRBLleida, 25198 Lleida, Spain 3 School of Medicine, Universitat de Lleida, 25008 Lleida, Spain 4 Division of Respiratory and Critical Care Medicine, The National University Hospital, Singapore 119228, Singapore; [email protected] * Correspondence: [email protected] Abstract: Video-assisted thoracic surgery (VATS) is the treatment of choice for recurrence preven- tion in patients with spontaneous pneumothorax (SP). Although the optimal surgical technique is uncertain, bullous resection using staplers in combination with mechanical pleurodesis, chemical pleurodesis and/or staple line coverage is usually undertaken. Currently, patient satisfaction, post- operative pain and other perioperative parameters have significantly improved with advancements in thoracoscopic technology, which include uniportal, needlescopic and nonintubated VATS variants. Ipsilateral recurrences after VATS occur in less than 5% of patients, in which case a redo-VATS is a feasible therapeutical option. Randomized controlled trials are urgently needed to shed light on the best definitive management of SP. Keywords: thoracoscopy; VATS; spontaneous pneumothorax; bullectomy; pleurodesis Citation: Porcel, J.M.; Lee, P. Thoracoscopy for Spontaneous 1. Introduction Pneumothorax. J. Clin. Med. 2021, 10, Pneumothorax can occur spontaneously or because of trauma or procedural compli- 3835. https://doi.org/10.3390/ cation. Spontaneous pneumothoraces (SP) are divided into primary (PSP) and secondary jcm10173835 (SSP). PSP occurs in someone without a known underlying lung disease, whereas SPP appears as a complication of an underlying lung disease, such as chronic obstructive pul- Academic Editors: Paola Ciriaco and Robert Hallifax monary disease, lung cancer, interstitial lung disease, or tuberculosis. -
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -

Dorsal Approach Rhinoplasty Dorsal Approach Rhinoplasty
AIJOC 10.5005/jp-journals-10003-1105 ORIGINAL ARTICLE Dorsal Approach Rhinoplasty Dorsal Approach Rhinoplasty Kenneth R Dubeta Part I: Historical Milestones in Rhinoplasty ABSTRACT Direct dorsal excision of skin and subcutaneous tissue is employed in rhinoplasty cases characterized by thick rigid skin to achieve satisfactory esthetic results, in which attempted repair by more conventional means would most likely frustrate both surgeon and patient. This historical review reminds us of the lesson: ‘History repeats itself.’ Built on a foundation of reconstructive rhinoplasty, modern cosmetic and corrective rhinoplasty have seen the parallel development of both open and closed techniques as ‘new’ methods are introduced and reintroduced again. It is from the perspective of constant evolution in the art of rhinoplasty surgery that the author presents, in Part II, his unique ‘eagle wing’ chevron incision technique of dorsal approach rhinoplasty, to overcome the problems posed by the rigid skin nose. Keywords: Dorsal approach rhinoplasty, Eagle wing incision, Fig. 1: Ancient Greek ‘perikephalea’ to support the Rigid skin nose, External approach rhinoplasty, Historical straightened nose1 milestones. How to cite this article: Dubeta KR. Dorsal Approach and functions of the nose. Refinement of these techniques Rhinoplasty. Int J Otorhinolaryngol Clin 2013;5(1):1-23. seemingly had to await three antecedent developments; Source of support: Nil topical vasoconstriction; topical, systemic and local Conflict of interest: None declared anesthesia; and safe, reliable sources of illumination. The last half of the 20th century has seen the dissemination of INTRODUCTION two of the most important developments in the history of Throughout the ages, numerous techniques of altering, nasal surgery: correcting and more recently, improving the appearance and 1. -
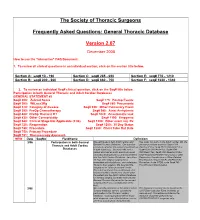
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Nonintubated Thoracoscopic Surgery Using Regional Anesthesia and Vagal Block and Targeted Sedation
Original Article Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation Ke-Cheng Chen1,2, Ya-Jung Cheng3, Ming-Hui Hung3, Yu-Ding Tseng1, Jin-Shing Chen1,2 1Department of Surgery, National Taiwan University Hospital Yun-Lin Branch, Yun-Lin County, Taiwan; 2Division of Thoracic Surgery, Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan; 3Department of Anesthesiology, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan Corresponding to: Dr. Jin-Shing Chen. Department of Surgery, National Taiwan University Hospital, No. 7, Chung Shan South Road, Taipei, Taiwan. Email: [email protected]. Objective: Thoracoscopic surgery without endotracheal intubation is a novel technique for diagnosis and treatment of thoracic diseases. This study reported the experience of nonintubated thoracoscopic surgery in a tertiary medical center in Taiwan. Methods: From August 2009 through August 2013, 446 consecutive patients with lung or pleural diseases were treated by nonintubated thoracoscopic surgery. Regional anesthesia was achieved by thoracic epidural anesthesia or internal intercostal blockade. Targeted sedation was performed with propofol infusion to achieve a bispectral index value between 40 and 60. The demographic data and clinical outcomes were evaluated by retrospective chart review. Results: Thoracic epidural anesthesia was used in 290 patients (65.0%) while internal intercostal blockade was used in 156 patients (35.0%). The final diagnosis were primary lung cancer in 263 patients (59.0%), metastatic lung cancer in 38 (8.5%), benign lung tumor in 140 (31.4%), and pneumothorax in 5 (1.1%). The median anesthetic induction time was 30 minutes by thoracic epidural anesthesia and was 10 minutes by internal intercostal blockade. -

Your Lung Operation Booklet
1 AMERICAN COLLEGE OF SURGEONS DIVISION OF EDUCATION SURGICAL PATIENT EDUCATION Table of Contents Welcome ...................................................................................1 Your Lungs ...............................................................................2 Lung Cancer ...........................................................................3 SURGICAL Understanding Your Operation ........................................4 PATIENT Preoperative Tests ................................................................5 EDUCATION Home Preparation ................................................................8 The Day of Your Operation ...............................................13 After Your Operation ..........................................................14 Your Recovery and Discharge .........................................17 When to Call Your Doctor .................................................19 Welcome You and your family are important members of the surgical team. The American College of Surgeons (ACS) “Your Lung Operation: Education for a Better Recovery” program will help you prepare for your operation and recovery. You and your family will know what to expect. You will learn how to work with your surgical team to ensure that you have the best surgical outcomes. COMPLETE THE “YOUR LUNG OPERATION” EDUCATION PROGRAM: Watch the DVD Read the booklet Review the Medication List and Quit Smoking Resources (inside front cover) Complete the Activity Log (inside front cover) Send us your evaluation after