Toman's Tuberculosis Case Detection, Treatment, and Monitoring
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019 Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2018 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. TABLE OF CONTENTS FOR NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL FOR MEDICARE SERVICES Introduction Introduction Intro-3 Purpose Intro-3 Policy Manual Background Intro-6 Edit Development and Review Process Intro-7 Sources of Information about NCCI and MUE Intro-9 Correspondence to CMS about NCCI and its Contents Intro-10 Chapter I - General Correct Coding Policies List of Acronyms I-3 A. Introduction I-5 B. Coding Based on Standards of Medical/Surgical I-9 Practice C. Medical/Surgical Package I-12 D. Evaluation and Management (E&M) Services I-17 E. Modifiers and Modifier Indicators I-19 F. Standard Preparation/Monitoring Services for I-27 Anesthesia G. Anesthesia Service Included in the Surgical Procedure I-27 H. HCPCS/CPT Procedure Code Definition I-28 I. CPT Manual and CMS Coding Manual Instructions I-29 J. CPT “Separate Procedure” Definition I-30 K. Family of Codes I-30 L. -

Tuberculosis Prevention, Diagnosis, and Care in Manitoba, 2008-2010
Tuberculosis Prevention, Diagnosis, and Care in Manitoba, 2008-2010: A Performance Analysis by C. Andrew Basham A Thesis submitted to the Faculty of Graduate Studies of The University of Manitoba in partial fulfilment of the requirements for the degree of MASTER OF SCIENCE Department of Community Health Sciences University of Manitoba Winnipeg Copyright © 2016 by C. Andrew Basham ABSTRACT A cross-sectional study of Manitoba TB Registry data was conducted using a set of performance measures based on the US Centers for Disease Control and Prevention TB Performance Objectives and Targets framework. The study investigated all cases of TB diagnosed in Manitoba during the period of 2008 to 2010 (inclusive), and their contacts. Seven performance measures (PMs) were analyzed: treatment completion/cure, early diagnosis, HIV testing/reporting, paediatric cases, retreatment cases, contact elicitation, and contact assessment. Ethnic-origin, age, sex, geographic, and treatment history groups were compared on these PMs through log-binomial and robust Poisson regression analyses, implemented through a generalized estimating equations (GEE) modelling approach. An updated epidemiological profile is provided, along with a baseline of performance in TB prevention, diagnosis, and care in Manitoba. Significant differences were found between Manitoba sub-populations in the PMs. The PM framework developed in this study provided valuable information for TB program planning and evaluation. i ACKNOWLEDGEMENTS I would like to thank my Thesis Committee, and in particular Drs. Elias and Orr, for their commitment of time and energy towards this study. I would also like to acknowledge the Western Regional Training Centre in Health Services and Policy Research (WRTC) for providing me the funding to enter the M.Sc. -

Unusual Case of Non-Resolving Necrotizing Pneumonia: a Last Resort Measure for Cure
eCommons@AKU Department of Surgery Department of Surgery June 2016 Unusual case of non-resolving necrotizing pneumonia: a last resort measure for cure. Naseem Salahuddin Aga Khan University, [email protected] Naila Baig Ansari Aga Khan University Saulat H. Fatimi Aga Khan University, [email protected] Follow this and additional works at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg Part of the Surgery Commons Recommended Citation Salahuddin, N., Ansari, N., Fatimi, S. (2016). Unusual case of non-resolving necrotizing pneumonia: a last resort measure for cure.. JPMA: Journal of the Pakistan Medical Association, 66(6), 754-756. Available at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg/566 754 CASE REPORT Unusual case of non-resolving necrotizing pneumonia: A last resort measure for cure Naseem Salahuddin, 1 Naila Baig-Ansari, 2 Saulat Hasnain Fatimi 3 Abstract pathogen of acute CAP, 2,3 and accounts for most cases of To our knowledge, this is an unusual case of a community- slowly resolving pneumonia.The majority of previously acquired pneumonia (CAP) with sepsis secondary to healthy hospitalized patients with severe CAP responded Streptococcus pneumoniae that required lung resection satisfactorily to prompt initiation of appropriate antibiotic for a non-resolving consolidation. A 74 year old previously therapy; however, it is estimated that 10% of hospitalized healthy woman, presented with acute fever, chills and CAP patients have slowly resolving or nonresolving pleuritic chest pain in Emergency Department (ED). A disease. 4 diagnosis of CAP was established with a Pneumonia Severity Index CURB-65 score of 5/5. In the ER, she was Case Report promptly and appropriately managed with antibiotics History: A 74 year old woman who was previously and aggressive supportive therapy. -
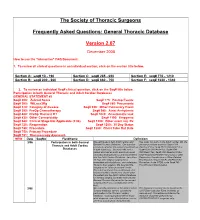
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

114.3 Cmr: Division of Health Care Finance and Policy Ambulatory Care
114.3 CMR: DIVISION OF HEALTH CARE FINANCE AND POLICY AMBULATORY CARE 114.3 CMR 40.00: RATES FOR SERVICES UNDER M.G.L. c. 152, WORKERS’ COMPENSATION ACT Section 40.01: General Provisions 40.02: General Definitions 40.03: Service and Rate Coverage Provisions 40.04: Provisions Affecting Eligible Providers 40.05: Policies for Individual Service Types 40.06: Fees 40.07: Appendices 40.08: Severability 40.01: General Provisions (1) Scope, Purpose and Effective Date. 114.3 CMR 40.00 governs the payment rates effective April 1, 2009 for purchasers of health care services under M.G.L. c. 152, the Workers’ Compensation Act. Payment rates for services provided by hospitals are set forth in 114.1 CMR 41.00. Program policies relating to medical necessity and clinical appropriateness are determined pursuant to M.G.L. c. 152 and 452 CMR 6.00. (2) Coverage. The payment rates set forth in 114.3 CMR 40.06 are full payment for services provided under M.G.L. c. 152, § 13, including any related administrative or overhead costs. The insurer, employer and health care service provider may agree upon a different payment rate for any service set forth in the fee schedule in 114.3 CMR 40.00. No employee may be held liable for the payment for health care services determined compensable under M.G.L. c. 152, § 13. (3) Administrative Bulletins. The Division may issue administrative bulletins to clarify substantive provisions of 114.3 CMR 40.00, or to publish procedure code updates and corrections. For coding updates and correction, the bulletin will list: (a) new code numbers for existing codes, with the corresponding cross references between existing and new codes numbers; (b) deleted codes for which there are no corresponding new codes; and (c) codes for entirely new services that require pricing. -

Drug Delivery Systems on Leprosy Therapy: Moving Towards Eradication?
pharmaceutics Review Drug Delivery Systems on Leprosy Therapy: Moving Towards Eradication? Luíse L. Chaves 1,2,*, Yuri Patriota 2, José L. Soares-Sobrinho 2 , Alexandre C. C. Vieira 1,3, Sofia A. Costa Lima 1,4 and Salette Reis 1,* 1 Laboratório Associado para a Química Verde, Rede de Química e Tecnologia, Departamento de Ciências Químicas, Faculdade de Farmácia, Universidade do Porto, 4050-313 Porto, Portugal; [email protected] (A.C.C.V.); slima@ff.up.pt (S.A.C.L.) 2 Núcleo de Controle de Qualidade de Medicamentos e Correlatos, Universidade Federal de Pernambuco, Recife 50740-521, Brazil; [email protected] (Y.P.); [email protected] (J.L.S.-S.) 3 Laboratório de Tecnologia dos Medicamentos, Universidade Federal de Pernambuco, Recife 50740-521, Brazil 4 Cooperativa de Ensino Superior Politécnico e Universitário, Instituto Universitário de Ciências da Saúde, 4585-116 Gandra, Portugal * Correspondence: [email protected] (L.L.C.); shreis@ff.up.pt (S.R.) Received: 30 October 2020; Accepted: 4 December 2020; Published: 11 December 2020 Abstract: Leprosy disease remains an important public health issue as it is still endemic in several countries. Mycobacterium leprae, the causative agent of leprosy, presents tropism for cells of the reticuloendothelial and peripheral nervous system. Current multidrug therapy consists of clofazimine, dapsone and rifampicin. Despite significant improvements in leprosy treatment, in most programs, successful completion of the therapy is still sub-optimal. Drug resistance has emerged in some countries. This review discusses the status of leprosy disease worldwide, providing information regarding infectious agents, clinical manifestations, diagnosis, actual treatment and future perspectives and strategies on targets for an efficient targeted delivery therapy. -

Translational Deep Phenotyping of Deaths Related to the COVID-19 Pandemic: Protocol for a Prospective Observational Autopsy Study
Open access Protocol BMJ Open: first published as 10.1136/bmjopen-2021-049083 on 27 August 2021. Downloaded from Translational deep phenotyping of deaths related to the COVID-19 pandemic: protocol for a prospective observational autopsy study Mikkel Jon Henningsen ,1 Apameh Khatam- Lashgari,1 Kristine Boisen Olsen,1 Christina Jacobsen,1 Christian Beltoft Brøchner ,2 Jytte Banner1 To cite: Henningsen MJ, ABSTRACT Strengths and limitations of this study Khatam- Lashgari A, Olsen KB, Introduction The COVID-19 pandemic is an international et al. Translational deep emergency with an extreme socioeconomic impact and a ► A standardised, prospective autopsy study on COVID- phenotyping of deaths high mortality and disease burden. The COVID-19 outbreak related to the COVID-19 19- related deaths with systematic data collection. is neither fully understood nor fully pictured. Autopsy studies pandemic: protocol for a ► A multidisciplinary, translational approach elucidat- can help understand the pathogenesis of COVID-19 and has prospective observational ing changes from protein level to whole human. already resulted in better treatment of patients. Structured autopsy study. BMJ Open ► A comprehensive biobank and extensive registry and systematic autopsy of COVID-19- related deaths will 2021;11:e049083. doi:10.1136/ data as an umbrella for planned and future research. bmjopen-2021-049083 enhance the mapping of pathophysiological pathways, not ► The internal control group partly compensates for possible in the living. Furthermore, it provides an opportunity Prepublication history and the observational design. ► to envision factors translationally for the purpose of disease additional supplemental material ► Limited by a selected sample of COVID-19 diseased prevention in this and future pandemics. -

Treatment and Outcomes of Community-Acquired Pneumonia at Canadian Hospitals Research Brian G
Treatment and outcomes of community-acquired pneumonia at Canadian hospitals Research Brian G. Feagan,* Thomas J. Marrie,† Catherine Y. Lau,‡ Recherche Susan L. Wheeler,‡ Cindy J. Wong,* Margaret K. Vandervoort* From *the London Clinical Abstract Trials Research Group, London, Ont.; †the Background: Community-acquired pneumonia is a common disease with a large Department of Medicine, economic burden. We assessed clinical practices and outcomes among patients University of Alberta, with community-acquired pneumonia admitted to Canadian hospitals. Edmonton, Alta.; Methods: A total of 20 hospitals (11 teaching and 9 community) participated. Data and ‡Janssen–Ortho from the charts of adults admitted during November 1996, January 1997 and Incorporated, Toronto, Ont. March 1997 were reviewed to determine length of stay (LOS), admission to an intensive care unit and 30-day in-hospital mortality. Multivariate analyses exam- This article has been peer reviewed. ined sources of variability in LOS. The type and duration of antibiotic therapy and the proportion of patients who were treated according to clinical practice CMAJ 2000;162(10):1415-20 guidelines were determined. Results: A total of 858 eligible patients were identified; their mean age was 69.4 (standard deviation 17.7) years. The overall median LOS was 7.0 days (in- terquartile range [IQR] 4.0–11.0 days); the median LOS ranged from 5.0 to 9.0 days across hospitals (IQR 6.0–7.8 days). Only 22% of the variability in LOS could be explained by known factors (disease severity 12%; presence of chronic obstructive lung disease or bacterial cause for the pneumonia 2%; hospital site 7%). -

Respiratory Tract Infections in the Tropics
9.1 CHAPTER 9 Respiratory Tract Infections in the Tropics Tim J.J. Inglis 9.1 INTRODUCTION Acute respiratory infections are the single most common infective cause of death worldwide. This is also the case in the tropics, where they are a major cause of death in children under five. Bacterial pneumonia is particularly common in children in the tropics, and is more often lethal. Pulmonary tuberculosis is the single most common fatal infection and is more prevalent in many parts of the tropics due to a combination of endemic HIV infection and widespread poverty. A lack of diagnostic tests, limited access to effective treatment and some traditional healing practices exacerbate the impact of respiratory infection in tropical communities. The rapid urbanisation of populations in the tropics has increased the risk of transmitting respiratory pathogens. A combination of poverty and overcrowding in the peri- urban zones of rapidly expanding tropical cities promotes the epidemic spread of acute respiratory infection. PART A. INFECTIONS OF THE LOWER RESPIRATORY TRACT 9.2 PNEUMONIA 9.2.1 Frequency Over four million people die from acute respiratory infection per annum, mostly in developing countries. There is considerable overlap between these respiratory deaths and deaths due to tuberculosis, the single commonest fatal infection. The frequency of acute respiratory infection differs with location due to host, pathogen and environmental factors. Detailed figures are difficult to find and often need to be interpreted carefully, even for tuberculosis where data collection is more consistent. But in urban settings the enormity of respiratory infection is clearly evident. Up to half the patients attending hospital outpatient departments in developing countries have an acute respiratory infection. -

Emblemhealth's Pre-Authorization List
EmblemHealth's Pre-authorization List This is a complete list of all services requiring a Prior Approval for HIP members or a Pre-Certification for GHI members* (jointly referred to as "pre-authorization") subject to their benefit plan's coverage for all places of service, including Office (POS 11). The list accounts for EmblemHealth's medical policies, medical technology database, provider manual, and special utilization management programs. Pre-authorization is not a guarantee of payment. Payment is subject to a member's eligibility for benefits on the date of service. Emergency services do not require a pre-authorization. *GHI PPO City of New York employees and non-Medicare eligible retirees with GHI PPO benefits will be managed by Empire BCBS for inpatient and outpatient services. To see what needs authorization, use their look-up tool: https://www.empireblue.com/wps/portal/ehpprovider. CPT/ HCPCS Description Code 0008M Oncology (breast), mRNA analysis of 58 genes using hybrid capture, on formalin-fixed paraffin- embedded (FFPE) tissue, prognostic algorithm reported as a risk score 00640 Anesthesia for manipulation of the spine or for closed procedures on the cervical, thoracic or lumbar spine 0085T Breath test for heart transplant rejection 0100T Placement of a subconjunctival retinal prosthesis receiver and pulse generator, and implantation of intra-ocular retinal electrode array, with vitrectomy 0195T Arthrodesis, pre-sacral interbody technique, disc space preparation, discectomy, without instrumentation, with image guidance, includes -

World Bank Document
Document of The World Bank Public Disclosure Authorized Report No. 15894-IN STAFF APPRAISAL REPORT INDIA Public Disclosure Authorized PROPOSED TUBERCULOSIS CONTROL PROJECT January 6, 1997 Public Disclosure Authorized Public Disclosure Authorized South Asia Country Department II (Bhutan, India and Nepal) Population and Huaman Resources Operations Division CURRENCY EQUIVALENTS (As of July 1996) Currency Unit = Rupee Rupee 34.70 =US$ 1.00 Rupee 1.0 US$ 0.0288 METRIC EQUIVALENTS 1 Meter (m) 3.28 Feet (ft) 1 Kilometer 0.62 Miles GOVERNMENT FISCAL YEAR April 1 - March 31 ABBREVIATIONS AND ACRONYMS ADGHS Assistant Director General of Health Services AFB Acid Fast Bacilli AIDS Acquired Immunodeficiency Syndrome ARI Annual Risk of Infection BCG Bacilli of Calmette and Guerin BRS Basic Radiological System CDC Centers for Disease Control and Prevention CHC Community Health Center CHEB Central Health Education Bureau DALYs Disability Adjusted Life Years DANIDA Danish Development Agency DDG Deputy Director General DGHS Director General of Health Services DHO District Health (Medical) Officer DOT Directly-Observed Therapy DTC District Tuberculosis Center DTO District Tuberculosis Officer E Ethambutol GOI Government of India H or INH Isoniazid - ii - ABBREVIATIONS AND ACRONYMS (Continued) HIV Human Immunodeficiency Virus IDA International Development Agency IMA Indian Medical Association LCC Long Course Chemotherapy LSHTM London School of Hygiene and Tropical Medicine MIS Management Information System MO Medical Officer MOHFW Ministry of Health and -

2017 Pulmonary Coding and Payment Quick Reference
2017 Coding & Payment Quick Reference Select Pulmonary Procedures Payer policies will vary and should be verified prior to treatment for limitations on diagnosis, coding or site of service requirements. The coding options listed within this guide are commonly used codes and are not intended to be an all-inclusive list. We recommend consulting your relevant manuals for appropriate coding options. Medicare Physician, Hospital Outpatient, and ASC Payments The bronchoscopy procedures listed below (except CPT® Codes 31622, 31660, and 31661) all include a diagnostic bronchoscopy when performed by the same physician. 2017 Medicare National Average Payment RVUs Physician‡,2 Facility3 CPT® Total Total Hospital Code Description Work In-Office In-Facility ASC Code1 Office Facility Outpatient Biopsy 31625 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, 3.11 9.43 4.53 $338 $163 $1,270† $569 when performed; with bronchial or endobronchial biopsy(s), single or multiple sites 31628 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, 3.55 10.00 5.09 $359 $183 $2,431† $1,117 when performed; with transbronchial lung biopsy(s), single lobe 31632 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, 1.03 1.84 1.42 $66 $51 $0 $0 when performed; with transbronchial lung biopsy(s), each additional lobe (List separately in addition to code for primary procedure)* Cytology and Brush 31622 Bronchoscopy, rigid or flexible, including fluoroscopic guidance, 2.53 6.86 3.81 $246 $137 $1,270† $569 when performed; diagnostic,