Do Not Report Meddra Preferred Term, Please Report the Verbatim Term!
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
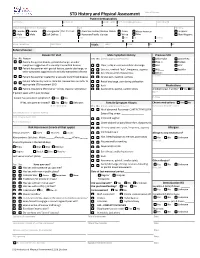
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref. name/AKA/pronoun Date of Birth Sex (at birth) Gender (all that apply Race Ethnicity Female Female Transgender Pref. Pronoun: American Indian/Alaskan Native Asian African American Hispanic Male Male Self Define: Hawaiian/Pacific Islander White Other Non-Hispanic Street Address City State Zip County Home Telephone Cell Phone Vitals: Temp: Pulse: RR: BP: Referral Source: Reason for Visit Male Symptom History Previous STD Yes No Reason Yes No (check appropriate boxes) Chlamydia Gonorrhea Patient has genital lesions, genital discharge, or other Hep. C Herpes symptoms suggestive of a sexually transmitted disease Clear, milky or mucoid urethral discharge HIV HPV Patient has partner with genital lesions, genital discharge, or Dysuria , urethral “itch”, frequency, urgency PID Syphilis other symptoms suggestive of a sexually transmitted disease Sore throat and/or hoarseness Other: Patient has partner treated for a sexually transmitted disease Scrotal pain, swelling, redness Comments: Patient referred by local or state DIS. Review labs and refer to Rectal discharge, pain during defecation appropriate STD treatment SDO Rash Medications Patient requesting STD testing – denies reasons listed above Asymmetric, painful, swollen joints Antibiotics last 4 weeks? Yes No If patient seen within past 30 days: Name Purpose Patient has persistent symptoms? Yes No If Yes, was partner treated? Yes No Unknown Female Symptom History Chronic medications -

Current Concepts in Management of Outlet Obstruction
Current Concepts in Management of Outlet Obstruction A. Infantino, R. Bellomo, F. Galanti, L. Pisegna Cerone Outlet constipation is often characterized by dis- ical defects should always be considered. abling symptoms consisting of the strenuous Incidences of 33% of occult rectal prolapse, 1.7% effort to expel stools, a feeling of incomplete of sigmoidocele, and 10% of anismus have been evacuation, rectal tenesmus and a repeated call defecographically demonstrated after a clinical to toilet, digitations, and the necessity of enemas diagnosis of rectocele and obstructed defecation and/or suppositories [1]. It is related to multiple [4]. This is very important because of the subse- alterations, variously associated and in different quent different approaches: conservative for degrees, of the organs of the pelvis and per- anismus or surgical intervention for other condi- ineum: rectocele, rectal occult-mucosal or full- tions. thickness prolapse, and enterocele. Synchronous anatomic alterations in the urogynecological sector can also be found: uterine, vaginal, and Rectal Intussusception bladder prolapses [2]. A unique pathophysiolog- ic theory has been suggested but not yet demon- Rectal intussusception is often difficult to diag- strated [3]. As a consequence of the variability of nose. Radiological findings that can be indicative the affected organs, great difficulty in reaching a of rectal intussusception can be found also in diagnosis exists, and the management and treat- healthy people [5, 6]. Even the interpretation of ment of outlet constipation is, to date, far from radiological images is still a controversial issue being standardized. [4, 7–10]. There is open discussion as to whether magnetic resonance imaging (MRI) can add more information than cystocolpodefecography Clinical Conditions [9, 10], which remains the most useful and sim- plest test. -

COVID-19 Mrna Pfizer- Biontech Vaccine Analysis Print
COVID-19 mRNA Pfizer- BioNTech Vaccine Analysis Print All UK spontaneous reports received between 9/12/20 and 22/09/21 for mRNA Pfizer/BioNTech vaccine. A report of a suspected ADR to the Yellow Card scheme does not necessarily mean that it was caused by the vaccine, only that the reporter has a suspicion it may have. Underlying or previously undiagnosed illness unrelated to vaccination can also be factors in such reports. The relative number and nature of reports should therefore not be used to compare the safety of the different vaccines. All reports are kept under continual review in order to identify possible new risks. Report Run Date: 24-Sep-2021, Page 1 Case Series Drug Analysis Print Name: COVID-19 mRNA Pfizer- BioNTech vaccine analysis print Report Run Date: 24-Sep-2021 Data Lock Date: 22-Sep-2021 18:30:09 MedDRA Version: MedDRA 24.0 Reaction Name Total Fatal Blood disorders Anaemia deficiencies Anaemia folate deficiency 1 0 Anaemia vitamin B12 deficiency 2 0 Deficiency anaemia 1 0 Iron deficiency anaemia 6 0 Anaemias NEC Anaemia 97 0 Anaemia macrocytic 1 0 Anaemia megaloblastic 1 0 Autoimmune anaemia 2 0 Blood loss anaemia 1 0 Microcytic anaemia 1 0 Anaemias haemolytic NEC Coombs negative haemolytic anaemia 1 0 Haemolytic anaemia 6 0 Anaemias haemolytic immune Autoimmune haemolytic anaemia 9 0 Anaemias haemolytic mechanical factor Microangiopathic haemolytic anaemia 1 0 Bleeding tendencies Haemorrhagic diathesis 1 0 Increased tendency to bruise 35 0 Spontaneous haematoma 2 0 Coagulation factor deficiencies Acquired haemophilia -

Post-Operative Clinical, Manometric, and Defecographic Findings in Patients Undergoing Unsuccessful STARR Operation for Obstructed Defecation
International Journal of Colorectal Disease (2019) 34:837–842 https://doi.org/10.1007/s00384-019-03263-9 ORIGINAL ARTICLE Post-operative clinical, manometric, and defecographic findings in patients undergoing unsuccessful STARR operation for obstructed defecation A. Picciariello1 & V. Papagni1 & G. Martines1 & M. De Fazio1 & R. Digennaro1 & D. F. Altomare1 Accepted: 6 February 2019 /Published online: 19 February 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Aim To evaluate the reason for failure of STARR (stapled transanal rectal resection) operation for obstructed defecation. Methods A retrospective study (June 2012–December 2017) was performed using a prospectively maintained database of patients who underwent STARR operation for ODS (obstructed defecation syndrome), complaining of persisting or de novo occurrence of pelvic floor dysfunctions. Postoperative St Mark’s and ODS scores were evaluated. AVASwas used to score pelvic pain. Patients’ satisfaction was estimated administering the CPGAS (clinical patient grading assessment scale) questionnaire. Objective evaluation was performed by dynamic proctography and anorectal manometry. Results Ninety patients (83.3% females) operated for ODS using STARR technique were evaluated. Median ODS score was 19 while 20 patients (22%) reported de novo fecal urgency and 4 patients a worsening of their preoperative fecal incontinence. Dynamic proctography performed in 54/90 patients showed a significant (> 3.0 cm) rectocele in 19 patients, recto-rectal intussusception in 10 patients incomplete emptying in 24 patients. When compared with internal normal standards, anorectal manometry showed decreased rectal compliance and maximum tolerable volume in patients with urgency. Nine patients reported a persistent postoperative pelvic pain (median VAS score 6). Conclusion Failure of STARR to treat ODS, documented by persisting ODS symptoms, fecal urgency, or chronic pelvic pain, is often justified by the persistence or de novo onset of alteration of the anorectal anatomy at defecation. -

Endoscopic Characteristics and Causes of Misdiagnosis of Intestinal Schistosomiasis
MOLECULAR MEDICINE REPORTS 8: 1089-1093, 2013 Endoscopic characteristics and causes of misdiagnosis of intestinal schistosomiasis CHUNCUI YE, SHIYUN TAN, LIN JIANG, MING LI, PENG SUN, LEI SHEN and HESHENG LUO Department of Gastroenterology, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060, P.R. China Received February 21, 2013; Accepted July 27, 2013 DOI: 10.3892/mmr.2013.1648 Abstract. The aim of this study was to determine the clinical Introduction and endoscopic manifestations, and pathological character- istics of intestinal schistosomiasis in China, in order to raise Schistosomiasis is one of the most widespread parasitic infec- awareness of intestinal schistosomiasis and prevent misdi- tions worldwide. The three predominant schistosome species agnosis and missed diagnosis. The retrospective analysis of identified to infect humans are Schistosoma haematobium clinical and endoscopic manifestations, and histopathological (endemic in Africa and the eastern Mediterranean), S. mansoni characteristics, were conducted for 96 patients with intestinal (endemic in Africa, the Middle East, the Caribbean and South schistosomiasis. Among these patients, 21 lived in areas that America) and S. japonicum (endemic mainly in China, Japan were not infected with Schistosoma and 25 (26%) had no history and the Philippines) (1). It is estimated that 843,007 individuals of schistosome infection or contact with infected water. These in China are infected with S. japonicum (2). Intestinal schis- patients were mainly hospitalized due to symptoms of diarrhea, tosomiasis is an acute or chronic, specific enteropathy caused mucus and bloody purulent stool. Sixteen cases were of the by the deposition of schistosome ovum on the colon and rectal acute enteritis type, and colonoscopy results determined hyper- walls. -

Seetha Kazhichal
A STUDY ON SEETHA KAZHICHAL Dissertation submitted to THE TAMILNADU DR. M.G.R MEDICAL UNIVERSITY Chennai-32 For the partial fulfillment of the requirements to the Degree of DOCTOR OF MEDICINE (SIDDHA) (Branch IV - Kuzhanthai Maruthuvam) Department of Kuzhanthai Maruthuvam GOVERNMENT SIDDHA MEDICAL COLLEGE PALAYAMKOTTAI – 627 002. MARCH 2008 CONTENTS Page. No INTRODUCTION 1 AIM AND OBJECTIVES 3 REVIEW OF SIDDHA LITERATURES 5 REVIEW OF MODERN LITERATURES 25 MATERIALS AND METHODS 44 RESULTS AND OBSERVATIONS 46 DISCUSSION 67 SUMMARY 73 CONCLUSION 75 ANNEXURES ¾ PREPARATION AND PROPERTIES OF TRIAL MEDICINE 76 ¾ BIOCHEMICAL ANALYSIS OF TRIAL MEDICINE 81 ¾ ANTI MICROBIAL STUDY OF TRIAL MEDICINE 84 ¾ PHARMACOLOGICAL ANALYSIS OF TRIAL MEDICINE 85 ¾ LABORATORY DIAGNOSIS OF SHIGELLA AND ENTAMOEBA HISTOLYTICA 97 ¾ PROFORMA OF CASE SHEET 102 BIBLIOGRAPHY 114 CERTIFICATE Certified that I have gone through the dissertation submitted by ------------------- a student of Final M.D.(s), Branch IV, Kuzhandhai Maruthuvam of this college and the dissertation does not represent or reproduce the dissertation submitted and approved earlier. Place: Palayamkottai Date: Professor and Head of the Department, (PG) Br IV, Kuzhanthai Maruthuvam, Govt. Siddha Medical College, Palayamkottai. ACKNOWLEDGEMENT First of all, I thank God for his blessings to complete my dissertation work successfully. My foremost thanks to The Vice Chancellor, The Tamil Nadu Dr.M.G.R.Medical University-Chennai , for giving permission to undertake this dissertation. I contribute my thanks to Dr.M.Thinakaran M.D(s)., The Principal,Govt. Siddha Medical College, Palayamkottai for granting permission and facilities to complete this dissertation. I owe a deep sense of gratitude to Dr.R.Patrayan M.D (s)., The Head of the department , Dr.N.Chandra Mohan M.D (s)., Lecturer, Department of Kuzhanthai Maruthuvam , Govt.Siddha Medical College, Palaymkottai for their encouragements , valuable suggestions and necessary guidance during this study. -

Sexually Transmitted Diseases Treatment Guidelines, 2015
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 64 / No. 3 June 5, 2015 Sexually Transmitted Diseases Treatment Guidelines, 2015 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Gonococcal Infections ...................................................................................... 60 Methods ....................................................................................................................1 Diseases Characterized by Vaginal Discharge .......................................... 69 Clinical Prevention Guidance ............................................................................2 Bacterial Vaginosis .......................................................................................... 69 Special Populations ..............................................................................................9 Trichomoniasis ................................................................................................. 72 Emerging Issues .................................................................................................. 17 Vulvovaginal Candidiasis ............................................................................. 75 Hepatitis C ......................................................................................................... 17 Pelvic Inflammatory -

ESMO Colorectal Cancer Guide for Patients English
Colorectal Cancer What is colorectal cancer? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines COLORECTAL CANCER: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of colorectal cancer and appreciate the best treatment choices available according to the subtype of colorectal cancer. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of colorectal cancer. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the leading author of the clinical practice guidelines for professionals. It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Colorectal Cancer: a guide for patients - Information based on ESMO Clinical Practice Guidelines - v.2016.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO. -

Clinical Guidelines for Diagnosis and Treatment of Common Conditions in Kenya
Clinical Guidelines for Diagnosis and Treatment of Common Conditions in Kenya Table of Contents Clinical Guidelines for Diagnosis and Treatment of Common Conditions in Kenya..................................1 FOREWORD..........................................................................................................................................3 PREFACE...............................................................................................................................................4 ACKNOWLEDGEMENTS.......................................................................................................................5 ABBREVIATIONS...................................................................................................................................5 1. ACUTE INJURIES AND TRAUMA & SELECTED EMERGENCIES..................................................7 1.1. Anaphylaxis & Cardiac Arrest...................................................................................................7 1.2. Abdominal Trauma....................................................................................................................8 1.3. Bites & Rabies.........................................................................................................................10 1.4. Burns.......................................................................................................................................13 1.5. Disaster Plan...........................................................................................................................16 -

Bacillus Cereus
PHR 250 4/25/07, 6p Bacillus cereus Mehrdad Tajkarimi Materials from Maha Hajmeer Introduction: Bacillus cereus is a Gram-positive, spore-forming microorganism capable of causing foodborne disease At present three enterotoxins, able to cause the diarrheal syndrome, have been described: hemolysin BL (HBL), nonhemolytic enterotoxin (NHE) and cytotoxin K. HBL and NHE are three-component proteins, whereas cytotoxin K is a single protein toxin. Symptoms caused by the latter toxin are more severe and may even involve necrosis. In general, the onset of symptoms is within 6 to 24 h after consumption of the incriminated food. B. cereus food poisoning is underestimated probably because of the short duration of the illness (~24 h). History In 1887, Bacillus cereus isolated from air in a cowshed by Frankland and Frankland. Since 1950, many outbreaks from a variety of foods including meat and vegetable soups, cooked meat and poultry, fish, milk and ice cream were described in Europe. In 1969, the first well-characterized B. cereus outbreak in the USA was documented. Since 1971, a number of B. cereus poisonings of a different type, called the vomiting type, were reported. This type of poisoning was characterized by an acute attack of nausea and vomiting 1–5 h after consumption of the incriminated meal. Sometimes, the incubation time was as short as 15–30 min or as long as 6–12 h. Almost all the vomiting type outbreaks were associated with consumption of cooked rice. This type of poisoning resembled staphylococcal food poisoning. B. Cereus in the US Table 1: Best estimates of the annual cases and deaths caused by B. -

Rectal Prolapse: an Overview of Clinical Features, Diagnosis, and Patient-Specific Management Strategies
J Gastrointest Surg (2014) 18:1059–1069 DOI 10.1007/s11605-013-2427-7 EVIDENCE-BASED CURRENT SURGICAL PRACTICE Rectal Prolapse: An Overview of Clinical Features, Diagnosis, and Patient-Specific Management Strategies Liliana Bordeianou & Caitlin W. Hicks & Andreas M. Kaiser & Karim Alavi & Ranjan Sudan & Paul E. Wise Received: 11 November 2013 /Accepted: 27 November 2013 /Published online: 19 December 2013 # 2013 The Society for Surgery of the Alimentary Tract Abstract Rectal prolapse can present in a variety of forms and is associated with a range of symptoms including pain, incomplete evacuation, bloody and/or mucous rectal discharge, and fecal incontinence or constipation. Complete external rectal prolapse is characterized by a circumferential, full-thickness protrusion of the rectum through the anus, which may be intermittent or may be incarcerated and poses a risk of strangulation. There are multiple surgical options to treat rectal prolapse, and thus care should be taken to understand each patient’s symptoms, bowel habits, anatomy, and pre-operative expectations. Preoperative workup includes physical exam, colonoscopy, anoscopy, and, in some patients, anal manometry and defecography. With this information, a tailored surgical approach (abdominal versus perineal, minimally invasive versus open) and technique (posterior versus ventral rectopexy +/− sigmoidectomy, for example) can then be chosen. We propose an algorithm based on available outcomes data in the literature, an understanding of anorectal physiology, and expert opinion that can serve as a guide to determining the rectal prolapse operation that will achieve the best possible postoperative outcomes for individual patients. Keywords Rectal prolapse . Management . Surgery . ’ . Liliana Bordeianou and Caitlin W. Hicks are co-first authors. -

Speed Dating with a Palliative Care Pharmacist
Speed Dating with a Palliative Care Pharmacist Mary Lynn McPherson, PharmD, MA, MDE, BCPS Professor and Executive Program Director Online Master of Science, Graduate Certificates, and PhD* in Palliative Care Graduate.umaryland.edu/palliative | [email protected] *pending MHEC approval Objectives 1. Discuss 3 pearls related to pharmacology of palliative medications. 2. Discuss 3 pearls related to appropriateness of maintenance medications in EOL care. 3. Discuss 3 pearls related to using palliative medications in a safe and effective manner. Equianalgesic Opioid Dosing 2010 Equianalgesic Doses (mg) 2018 Equianalgesic Doses (mg) Drug Parenteral Oral Drug Parenteral Oral Morphine 10 30 Morphine 10 25 Fentanyl 0.1 NA Fentanyl 0.15 NA Hydrocodone NA 30 Hydrocodone NA 25 Hydromorphone 1.5 7.5 Hydromorphone 2 5 Oxycodone 10* 20 Oxycodone 10* 20 *Not available in the US Reprinted with permission from McPherson ML. Demystifying opioid conversion calculations: a guide for effective dosing, 2nd ed. Bethesda: ASHP; ©2018. NOTE: Learner is STRONGLY encouraged to access original work to review all caveats and explanations pertaining to this chart. Equianalgesic Opioid Dosing 2010 Equianalgesic Doses (mg) 2018 Equianalgesic Doses (mg) Drug Parenteral Oral Drug Parenteral Oral Morphine 10 30 Morphine 10 25 Fentanyl 0.1 NA Fentanyl 0.15 NA Hydrocodone NA 30 Hydrocodone NA 25 Hydromorphone 1.5 7.5 Hydromorphone 2 5 Oxycodone 10* 20 Oxycodone 10* 20 *Not available in the US Reprinted with permission from McPherson ML. Demystifying opioid conversion calculations: a guide for effective dosing, 2nd ed. Bethesda: ASHP; ©2018. NOTE: Learner is STRONGLY encouraged to access original work to review all caveats and explanations pertaining to this chart.