MEC Logo Proctitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -

Introduction Remove the Udder Removing the Pizzle (Penis)
fig . removing the udder, cut outwards through the skin fig 2. removing the pizzle Introduction This guide describes the carcass dressing procedures either side of the pizzle joining the cuts around the that are ideally carried out in a deer larder, after back of the scrotum. Continue the single central cut the gralloch has been performed in the field. The through the skin almost to the anus, taking care not Gralloch guide should be considered essential to damage the haunches. Pull the pizzle free where it companion reading. Both are linked to the Carcass runs over the pelvis, cutting the blood vessels. Use Inspection, Carcass Transport, Basic Hygiene, and the knife to free the pizzle where it turns forward Larder guides. inside the “V” of the pelvis. Leave outside the carcass (draped down the back if the carcass is suspended). Remove the udder It will be removed with the aitch bone, bladder, Fig 1. This is best done in the larder but a large udder remainder of the rectum and anus, later. can prevent access to the rear end and may have to be removed in the field before opening the stomach. Split the aitch bone Pinch the skin just in front of the udder and pulling Figs 3. and 4. Note that some venison processors on it all the time, cut around the udder, removing it would prefer that the aitch bone remains intact, whole, with the skin. Do not take the cut any further check before cutting. While causing the least possible rearwards until back in the larder. -
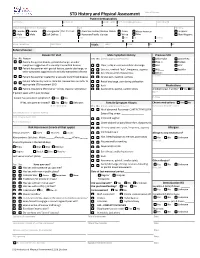
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref
STD History and Physical Assessment Date of Service: Patient Demographics Last Name First Name Middle Initial Pref. name/AKA/pronoun Date of Birth Sex (at birth) Gender (all that apply Race Ethnicity Female Female Transgender Pref. Pronoun: American Indian/Alaskan Native Asian African American Hispanic Male Male Self Define: Hawaiian/Pacific Islander White Other Non-Hispanic Street Address City State Zip County Home Telephone Cell Phone Vitals: Temp: Pulse: RR: BP: Referral Source: Reason for Visit Male Symptom History Previous STD Yes No Reason Yes No (check appropriate boxes) Chlamydia Gonorrhea Patient has genital lesions, genital discharge, or other Hep. C Herpes symptoms suggestive of a sexually transmitted disease Clear, milky or mucoid urethral discharge HIV HPV Patient has partner with genital lesions, genital discharge, or Dysuria , urethral “itch”, frequency, urgency PID Syphilis other symptoms suggestive of a sexually transmitted disease Sore throat and/or hoarseness Other: Patient has partner treated for a sexually transmitted disease Scrotal pain, swelling, redness Comments: Patient referred by local or state DIS. Review labs and refer to Rectal discharge, pain during defecation appropriate STD treatment SDO Rash Medications Patient requesting STD testing – denies reasons listed above Asymmetric, painful, swollen joints Antibiotics last 4 weeks? Yes No If patient seen within past 30 days: Name Purpose Patient has persistent symptoms? Yes No If Yes, was partner treated? Yes No Unknown Female Symptom History Chronic medications -

How to Increase Your Enjoyment of Sex
BETTER SEX BETTER SEX BETTER SEX BETTER SEX BETTER SEX OF SEX ENJO YOUR INCREASE HOW TO for women and women for their partners YMENT “Sexual health is a state of physical, emotional, mental and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled.” Definition of sexual health, World Health Organisation SAFER SEX Using condoms for penetrative sex is the best way to protect yourself and your partners from Sexually Transmitted Infections, including HIV. Condoms also offer good protection from unwanted pregnancy. In the text of this booklet, we have chosen not to refer constantly to the use of condoms. Instead, we encourage you to make your own decisions about protecting yourself and others in each instance of sexual activity you undertake. 1 HOW TO INCREASE YOUR ENJOYMENT OF SEX This leaflet provides information on how to help yourself improve your enjoyment of sex. It has three main parts: Suggestions on how to improve sex generally, without doing formal exercises. These apply to both casual and regular partners. Exercises you can do on your own — for women who have difficulty getting turned on or experiencing orgasm, and who may or may not have a regular partner. Exercises you can do with a partner — for women who have difficulty getting turned on, or who have difficulty having an orgasm or enjoying penetrative sex. -

The Onset of Clinical Manifestations in Inflammatory Bowel Disease Patients
AG-2018-65 ORIGINAL ARTICLE dx.doi.org/10.1590/S0004-2803.201800000-73 The onset of clinical manifestations in inflammatory bowel disease patients Viviane Gomes NÓBREGA1, Isaac Neri de Novais SILVA1, Beatriz Silva BRITO1, Juliana SILVA1, Maria Carolina Martins da SILVA1 and Genoile Oliveira SANTANA2,3 Received 29/10/2017 Accepted 10/8/2018 ABSTRACT – Background – The diagnosis of inflammatory bowel disease is often delayed because of the lack of an ability to recognize its major clinical manifestations. Objective – Our study aimed to describe the onset of clinical manifestations in inflammatory bowel disease patients. Methods – A cross-sec- tional study. Investigators obtained data from interviews and the medical records of inflammatory bowel disease patients from a reference centre located in Brazil. Results – A total of 306 patients were included. The mean time between onset of symptoms and diagnosis was 28 months for Crohn’s disease and 19 months for ulcerative colitis. The main clinical manifestations in Crohn’s disease patients were weight loss, abdominal pain, diarrhoea and asthenia. The most relevant symptoms in ulcerative colitis patients were blood in the stool, faecal urgency, diarrhoea, mucus in the stool, weight loss, abdominal pain and asthenia. It was observed that weight loss, abdominal pain and distension, asthenia, appetite loss, anaemia, insomnia, fever, nausea, perianal disease, extraintestinal manifestation, oral thrush, vomiting and abdominal mass were more frequent in Crohn’s patients than in ulcerative colitis patients. The frequencies of urgency, faecal incontinence, faeces with mucus and blood, tenesmus and constipation were higher in ulcerative colitis patients than in Crohn’s disease patients. -
Ulcerative Proctitis
Patient & Family Guide 2016 Ulcerative Proctitis www.nshealth.ca Ulcerative Proctitis What is Inflammatory Bowel Disease? Inflammatory bowel disease (IBD) is the general name for diseases that cause inflammation (swelling and irritation) in the intestines (“gut”). It includes the following: • Ulcerative proctitis • Crohn’s disease • Ulcerative colitis What are your questions? Please ask. We are here to help you. 1 What is ulcerative proctitis and how is it different from ulcerative colitis? Ulcerative proctitis (UP) is a type of ulcerative colitis (UC). UC is an inflammatory disease of the colon (large intestine or large bowel). The inner lining of the colon becomes inflamed and has ulcerations (sores). The entire large bowel is involved in UC. When only the lowest part of the colon is involved (the rectum, 15 to 20 cm from the anus), it is called ulcerative proctitis. 15-20 cm Rectum Large intestine (large bowel) 2 How is ulcerative proctitis diagnosed? • A test called a sigmoidoscopy will tell us if you have this problem. The doctor uses a special tube which bends and has a small light and camera on the end to look at the inside of your lower bowel and rectum. The tube is passed through the anus to the rectum and into the last 25 cm of the large bowel. • A biopsy (small piece of bowel tissue is taken) during the test and sent to the lab for study. • Most people do not find the test and biopsy uncomfortable and medicine to relax or make you sleepy is not usually needed. What are the symptoms of ulcerative proctitis? • Rectal bleeding and itching, passing mucus through the rectum, and feeling like you always need to pass stool (poop) even though your bowel is empty. -

Ulcerative Proctitis
Ulcerative Proctitis Ulcerative proctitis is a mild form of ulcerative colitis, a ulcerative proctitis are not at any greater risk for developing chronic inflammatory bowel disease (IBD) consisting of fine colorectal cancer than those without the disease. ulcerations in the inner mucosal lining of the large intestine that do not penetrate the bowel muscle wall. In this form of colitis, Diagnosis the inflammation begins at the rectum, and spreads no more Typically, the physician makes a diagnosis of ulcerative than about 20cm (~8″) into the colon. About 25-30% of people proctitis after taking the patient’s history, doing a general diagnosed with ulcerative colitis actually have this form of the examination, and performing a standard sigmoidoscopy. A disease. sigmoidoscope is an instrument with a tiny light and camera, The cause of ulcerative proctitis is undetermined but there inserted via the anus, which allows the physician to view the is considerable research evidence to suggest that interactions bowel lining. Small biopsies taken during the sigmoidoscopy between environmental factors, intestinal flora, immune may help rule out other possible causes of rectal inflammation. dysregulation, and genetic predisposition are responsible. It is Stool cultures may also aid in the diagnosis. X-rays are not unclear why the inflammation is limited to the rectum. There is a generally required, although at times they may be necessary to slightly increased risk for those who have a family member with assess the small intestine or other parts of the colon. the condition. Although there is a range of treatments to help ease symptoms Management and induce remission, there is no cure. -

Bowel Function Anatomy
BOWEL FUNCTION ANATOMY Most of America gives little thought to bowel control. However, bowel control is actually a complex process involving the coordination of many different muscles and nerves. The bowel is considered to be a part of the digestive or gastrointestinal system. It is designed to help the body absorb nutrients and fluids from the foods we eat and drink. After taking out everything the body needs, the bowel then expels the leftover waste. The beginning of the bowel is the small intestine, sometimes referred to as the small bowel. This is where the useful nutrients are absorbed from what you eat. The small bowel delivers the waste to the colon, or large bowel. The colon is a 5-6 foot long muscular tube that delivers stool to the rectum. As the stool moves through the colon, the fluids are removed and absorbed into the body. The consistency of the stool is dependent upon many things, including how long the stool sits in the colon, how much of the water has been absorbed from the waste, and the amount of fiber and fluids in your diet. Stool consistency can vary from hard lumps to mushy to very loose, watery stool. The best and easiest consistency of stool is soft, like toothpaste; this consistency may be attained by adding fiber to your diet. Fiber helps move waste through the colon because it is indigestible by the human body. In other words, fiber adds ‘bulk’ to the stool. It is important to eat a diet high in fiber, however, most Americans lack fiber in their diet. -

Anal Sex an Informative Guide by Bedroom Kandi
AN INTRODUCTION TO ANAL SEX AN INFORMATIVE GUIDE BY BEDROOM KANDI Anal sex encompasses a variety of sexual acts involving the anus and rectum. These can include anal fingering, analingus (oral-anal sex, sometimes called “rimming”), anal insertion (using an object like a strap-on or other toy) and anal intercourse (penis-in-anus sex). Anal sex can be enjoyed by individuals of any gender, and any orientation. Everyone has a back door, after all! But it requires preparation, care, and patience to make it pleasurable. Communication is Key! No surprise butt-sex. Always check in with your partner, talk things through, and 36% communicate about whether you’re Of American Women both on board for trying anal. Check in during anal sex to report having tried ? make sure you’re both enjoying yourselves! ANAL SEX “Is Anal Sex Common?” International Society for Sexual Medicine :) http://www.issm.info/sexual-health-qa/is-anal-sex-common/ www.bedroomkandi.com ©2017 Bedroom Kandi WHY TRY ANAL? IT FEELS GOOD - There are a lot IT FEELS BAD - in a good way! The of nerve endings to stimulate around taboos around anal sex can make it a the anus, including those in the man’s thrill and add something exciting to your prostate. bedroom routine. You naughty thing! IT SPICES THINGS UP - Trying IT CAN SUBVERT GENDER new things keeps things fresh, and ROLES - Either partner can penetrate anal sex will open up a whole new or receive, (using strap-ons or other toys range of sexual positions and activities for Lesbian or Straight couples), so you for you and your partner to share. -

Mimicry and Deception in Inflammatory Bowel Disease and Intestinal Behçet Disease
Mimicry and Deception in Inflammatory Bowel Disease and Intestinal Behçet Disease Erika L. Grigg, MD, Sunanda Kane, MD, MSPH, and Seymour Katz, MD Dr. Grigg is a Gastroenterology Fellow Abstract: Behçet disease (BD) is a rare, chronic, multisystemic, inflam- at Georgia Health Sciences University in matory disease characterized by recurrent oral aphthous ulcers, genital Augusta, Georgia. Dr. Kane is a Professor ulcers, uveitis, and skin lesions. Intestinal BD occurs in 10–15% of BD of Medicine in the Division of Gastro- patients and shares many clinical characteristics with inflammatory enterology and Hepatology at the Mayo Clinic in Rochester, Minnesota. Dr. Katz bowel disease (IBD), making differentiation of the 2 diseases very diffi- is a Clinical Professor of Medicine at cult and occasionally impossible. The diagnosis of intestinal BD is based Albert Einstein College of Medicine in on clinical findings—as there is no pathognomonic laboratory test—and Great Neck, New York. should be considered in patients who present with abdominal pain, diarrhea, weight loss, and rectal bleeding and who are susceptible to Address correspondence to: intestinal BD. Treatment for intestinal BD is similar to that for IBD, but Dr. Seymour Katz overall prognosis is worse for intestinal BD. Although intestinal BD is Albert Einstein College of Medicine extremely rare in the United States, physicians will increasingly encoun- 1000 Northern Boulevard ter these challenging patients in the future due to increased immigration Great Neck, NY 11021; rates of Asian and Mediterranean populations. Tel: 516-466-2340; Fax: 516-829-6421; E-mail: [email protected] ehçet disease (BD) is a rare, chronic, recurrent, multisys- temic, inflammatory disease that was first described by the Turkish dermatologist Hulusi Behçet in 1937 as a syndrome Bwith oral and genital ulcerations and ocular inflammation.1,2 Prevalence BD is more common and severe in East Asian and Mediter- ranean populations. -

Sexually Transmitted Diseases Treatment Guidelines, 2015
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 64 / No. 3 June 5, 2015 Sexually Transmitted Diseases Treatment Guidelines, 2015 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Gonococcal Infections ...................................................................................... 60 Methods ....................................................................................................................1 Diseases Characterized by Vaginal Discharge .......................................... 69 Clinical Prevention Guidance ............................................................................2 Bacterial Vaginosis .......................................................................................... 69 Special Populations ..............................................................................................9 Trichomoniasis ................................................................................................. 72 Emerging Issues .................................................................................................. 17 Vulvovaginal Candidiasis ............................................................................. 75 Hepatitis C ......................................................................................................... 17 Pelvic Inflammatory -

ESMO Colorectal Cancer Guide for Patients English
Colorectal Cancer What is colorectal cancer? Let us explain it to you. www.anticancerfund.org www.esmo.org ESMO/ACF Patient Guide Series based on the ESMO Clinical Practice Guidelines COLORECTAL CANCER: A GUIDE FOR PATIENTS PATIENT INFORMATION BASED ON ESMO CLINICAL PRACTICE GUIDELINES This guide for patients has been prepared by the Anticancer Fund as a service to patients, to help patients and their relatives better understand the nature of colorectal cancer and appreciate the best treatment choices available according to the subtype of colorectal cancer. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of disease. The medical information described in this document is based on the clinical practice guidelines of the European Society for Medical Oncology (ESMO) for the management of colorectal cancer. This guide for patients has been produced in collaboration with ESMO and is disseminated with the permission of ESMO. It has been written by a medical doctor and reviewed by two oncologists from ESMO including the leading author of the clinical practice guidelines for professionals. It has also been reviewed by patient representatives from ESMO’s Cancer Patient Working Group. More information about the Anticancer Fund: www.anticancerfund.org More information about the European Society for Medical Oncology: www.esmo.org For words marked with an asterisk, a definition is provided at the end of the document. Colorectal Cancer: a guide for patients - Information based on ESMO Clinical Practice Guidelines - v.2016.1 Page 1 This document is provided by the Anticancer Fund with the permission of ESMO.