Hypotonia Surestep Product Catalog Page 29 in Step with Pediatric Hypotonia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guide to Quality Individualized Education Program (IEP) Development and Implementation
The University of the State of New York The State Education Department Guide to Quality Individualized Education Program (IEP) Development and Implementation February 2010 (Revised December 2010) THE UNIVERSITY OF THE STATE OF NEW YORK Regents of The University MERRYL H. TISCH, Chancellor, B.A., M.A., Ed.D. .................................................. New York MILTON L. COFIELD, Vice Chancellor, B.S., M.B.A., Ph.D. .................................... Rochester ROBERT M. BENNETT, Chancellor Emeritus, B.A., M.S. ........................................ Tonawanda SAUL B. COHEN, B.A., M.A., Ph.D.......................................................................... Larchmont JAMES C. DAWSON, A.A., B.A., M.S., Ph.D. .......................................................... Plattsburgh ANTHONY S. BOTTAR, B.A., J.D. ............................................................................ Syracuse GERALDINE D. CHAPEY, B.A., M.A., Ed.D. ............................................................. Belle Harbor HARRY PHILLIPS, 3rd, B.A., M.S.F.S. .................................................................... Hartsdale JOSEPH E. BOWMAN, JR., B.A., M.L.S., M.A., M.Ed., Ed.D..................................... Albany JAMES R. TALLON, JR., B.A., M.A. ......................................................................... Binghamton ROGER TILLES, B.A., J.D. ....................................................................................... Great Neck KAREN BROOKS HOPKINS, B.A., M.F.A.................................................................. -

Lower Extremity Orthoses in Children with Spastic Quadriplegic Cerebral Palsy Implications for Nurses, Parents, and Caregivers
NOR200210.qxd 5/5/11 5:53 PM Page 155 Lower Extremity Orthoses in Children With Spastic Quadriplegic Cerebral Palsy Implications for Nurses, Parents, and Caregivers Kathleen Cervasio Understanding trends in the prevalence of children with cerebral prevalence for cerebral palsy in the United States is palsy is vital to evaluating and estimating supportive services for 2.4 per 1,000 children, an increase over previously re- children, families, and caregivers. The majority of children with ported data (Hirtz, Thurman, Gwinn-Hardy, Mohammad, cerebral palsy require lower extremity orthoses to stabilize their Chaudhuri, & Zalusky, 2007). Cerebral palsy is primar- muscles. The pediatric nurse needs a special body of knowledge ily a disorder of movement and posture originating in to accurately assess, apply, manage, teach, and evaluate the use the central nervous system with an incidence of 2.5 per 1,000 live births with spastic quadriplegia being the of lower extremity orthoses typically prescribed for this vulnera- common type of cerebral palsy (Blair & Watson, 2006). ble population. Inherent in caring for these children is the need This nonprogressive neurological disorder is defined as to teach the child, the family, and significant others the proper a variation in movement, coordination, posture, and application and care of the orthoses used in hospital and com- gait resulting from brain injury around birth (Blair & munity settings. Nursing literature review does not provide a Watson, 2006). Numerous associated comorbidities are basis for evidence in designing and teaching orthopaedic care usually present with cerebral palsy requiring various for children with orthoses. A protocol for orthoses management interventions. -

STEP 10: Promote and Market Your Accessibility
STEP 10: Promote and Market Your Accessibility Guidance on Public Information and Marketing How to Write and Speak about People with Disabilities and Older Adults Suggestions for Creating a Public Information and Outreach Checklist Tools for Effective Communication in Promotional and Marketing Materials Best Practices — Marketing and Publicity Guidance on Public Information and Marketing For patrons and visitors with disabilities the option to participate in a cultural event should be based on choice and not limited by lack of access. Evaluate your organizations marketing plan to see that it promotes your accessibility. Central to your outreach, public information, and marketing is communicating to the public about the accessibility of your facility, program and services. Informing the public about the accessibility of your facility and programs is one way to communicate to people with disabilities that they are welcome. The use of appropriate terminology and disability etiquette communicates respect and a positive attitude that is welcoming to people with disabilities. In addition to physical access to programs, auxiliary aids and services provides effective communication and makes programs accessible and enjoyable to everyone. Plan to provide an opportunity for a patron or visitor with a disability to request the auxiliary aid or service that suits their needs. For example, not all persons who are blind use Braille as their primary form of communication. Whereas one person who is blind might request a Braille program, someone else may prefer an audiotape. 217 Ensure that your staff is trained as to the location, usage and maintenance of auxiliary aids such as assistive listening devices in order that they are available and in good working order when requested. -

Caring for Children with Disabilities and Other Special Needs Important?
Children with Disabilities and Other Special Needs First Edition, 2006 California Childcare Health Program Administered by the University of California, San Francisco School of Nursing, Department of Family Health Care Nursing (510) 839-1195 • (800) 333-3212 Healthline www.ucsfchildcarehealth.org Funded by First 5 California with additional support from the California Department of Education Child Development Division and Federal Maternal and Child Health Bureau. This module is part of the California Training Institute’s curriculum for Child Care Health Consultants. Acknowledgements Th e California Childcare Health Program is administered by the University of California, San Francisco School of Nursing, Department of Family Health Care Nursing. We wish to credit the following people for their contributions of time and expertise to the development and review of this curriculum since 2000. Th e names are listed in alphabetical order: Main Contributors Abbey Alkon, RN, PhD Jane Bernzweig, PhD Lynda Boyer-Chu, RN, MPH Judy Calder, RN, MS Lyn Dailey, RN, PHN Robert Frank, MS Lauren Heim Goldstein, PhD Gail D. Gonzalez, RN Susan Jensen, RN, MSN, PNP Judith Kunitz, MA Mardi Lucich, MA Cheryl Oku, BA Pamm Shaw, MS, EdD Marsha Sherman, MA, MFCC Eileen Walsh, RN, MPH Sharon Douglass Ware, RN, EdD Rahman Zamani, MD, MPH Additional Contributors Robert Bates, Vella Black-Roberts, Judy Blanding, Terry Holybee, Karen Sokal-Gutierrez Outside Reviewers, 2003 Edition Jan Gross, RN, BSN, Greenbank, WA Jacqueline Quirk, RN, BSN, Chapel Hill, NC Angelique M. White, RNc, MA, MN, CNS, New Orleans, LA CCHP Staff Ellen Bepp, Robin Calo, Catherine Cao, Sara Evinger, Joanna Farrer, Krishna Gopalan, Maleya Joseph, Cathy Miller, Dara Nelson, Bobbie Rose, Griselda Th omas, Kim To, Mimi Wolff Graphic Designers Edi Berton (2006), Eva Guralnick (2001-2005) We also want to thank the staff and Advisory Committee members of the California Childcare Health Program for their support and contributions. -

Design and Development of a Soft Pediatric Support
DESIGN AND DEVELOPMENT OF A SOFT PEDIATRIC SUPPORT GARMENT FOR ANKLE-FOOT ORTHOSES WEARERS by Danielle A Civil A thesis submitted to the Faculty of the University of Delaware in partial fulfillment of the requirements for Master of Science in Fashion and Apparel Studies Spring 2019 © 2019 Danielle Civil All Rights Reserved DESIGN AND DEVELOPMENT OF A SOFT PEDIATRIC SUPPORT GARMENT FOR ANKLE-FOOT ORTHOSES WEARERS by Danielle A Civil Approved: __________________________________________________________ Michele Lobo, PT, Ph.D. Professor in charge of thesis on behalf of the Advisory Committee Approved: __________________________________________________________ Huantian Cao, Ph.D. Interim Chair of the Department of Fashion and Apparel Studies Approved: __________________________________________________________ John Pelesko, Ph.D. Interim Dean of the College of Arts and Sciences Approved: __________________________________________________________ Douglas J. Doren, Ph.D. Interim Vice Provost for Graduate and Professional Education ACKNOWLEDGMENTS Throughout the course of this research and my master’s program, I have received an incredible amount of support, guidance, and assistance. I would first like to thank my advisor Dr. Michele Lobo whose guidance and expertise was incredibly invaluable. I am extremely appreciative of her support and encouragement throughout this process and so inspired by her passion and drive to help children. I’d also like to thank the rest of my committee, Dr. Huantian Cao and Dr. Karin Grävare Silbernagel, for their expertise and feedback that made my research stronger. Thank you so much to the Move To Learn lab team who has offered an incredible amount of support to me during the span of this research. Specifically, thank you to Andrea Cunha for your helpful contributions to the functional testing and data analysis; her expertise, hard work, and kindness was invaluable throughout the duration of this research. -

Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H
Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H. Long, MD, PhD,a,b Jennifer G. Fiore, MD,a,b Riaz Gillani, MD,a,b Laurie M. Douglass, MD,c Alan M. Fujii, MD,d Jodi D. Hoffman, MDe A 2-day old term male infant was found to be hypotonic and minimally abstract reactive during routine nursing care in the newborn nursery. At 40 hours of life, he was hypoglycemic and had intermittent desaturations to 70%. His mother had an unremarkable pregnancy and spontaneous vaginal delivery. The mother’s prenatal serology results were negative for infectious risk factors. Apgar scores were 9 at 1 and 5 minutes of life. On day 1 of life, he fed, stooled, and voided well. Our expert panel discusses the differential diagnosis of hypotonia in a neonate, offers diagnostic and management recommendations, and discusses the final diagnosis. DRS LONG, FIORE, AND GILLANI, birth weight was 3.4 kg (56th PEDIATRIC RESIDENTS percentile), length was 52 cm (87th aDepartment of Medicine, Boston Children’s Hospital, d e percentile), and head circumference Boston, Massachusetts; and Neonatology Section, Medical A 2-day old male infant born at Genetics Section, cDivision of Child Neurology, and 38 weeks and 4 days was found to be was 33 cm (12th percentile). His bDepartment of Pediatrics, Boston Medical Center, Boston, limp and minimally reactive during physical examination at birth was Massachusetts routine care in the newborn nursery. normal for gestational age, with Drs Long, Fiore, and Gillani conceptualized, drafted, Just 5 hours before, he had an appropriate neurologic, cardiac, and and edited the manuscript; Drs Douglass, Fujii, and appropriate neurologic status when respiratory components. -

Choosing the Right Words
Nicole Koester “Choosing the NCDJ, Program Manager Walter Cronkite School of Journalism Right Words” and Mass Communication, Arizona State University “Until we learn to appreciate the power of language and the importance of using it responsibly, we will continue to produce negative social consequences for those victimized by dangerous language habits.” J. Dan Rothwell, Telling It Like It Isn’t: Language Misuse and Malpractice/ What We Can Do About It Our responsibility Use relevant disability terms that are: ● Accurate ● Objective ● Fair ● Neutral ● Respectful & Inclusive “Are we ‘handicapped’ or ‘disabled,’ ‘disabled people’ or ‘people with disabilities,’ ‘differently abled’ or ‘special needs?’” My Journey with Disability Language and Identity Andrew Pulrang, disability blogger, co-coordinator of #CripTheVote Monday, April 10, 2017 The disability community is not monolithic How has the disability language conversation evolved in the United States? Prior to 1960’s acceptable terms: idiot, imbecile, moron, crippled, lame, handicap 1970’s-1980’s disability advocacy expands along with the civil rights movement “People with disabilities” starts replacing “handicap” Source: http://www.disabilitymuseum.org/ 1990 - The “Capitol Crawl” and Americans with Disabilities Act On July 26, 1990, the Americans with Disabilities Act of 1990 was signed into law by President George H.W. Bush. “Spread the Word to End the Word” 2009 Disability Advocacy Campaign encouraging people to stop using the R-word – retard(ed) Rosa’s Law ● President Obama signs October, 5 2010 ● U.S. law that replaces several instances of “mental retardation” with “intellectual disability” in federal health, labor and education statutes. People-first language vs. Identity-first language People-first language Puts the emphasis on the person first; followed by a description of the disability. -

Learning Disability
Learning Disability Distributed By: Maine Parent Federation PO Box 2067 Augusta, Maine 04338 1-800-870-7746 (Maine Only) 207-588-1933 Email: [email protected] Online community: www.mpf.org Original: 01/2000 Updated: 05/2017 Learning Disability Information Disclaimer The purpose of the information packet is to provide individuals with reader friendly information. We believe that a good overview is a realistic one. For this reason we have included a variety of information that may include the more difficult characteristics of a diagnosis or topic along with medical, educational and best practice information. All information contained in this packet is for general knowledge, personal education and enrichment purposes. It is not intended to be a substitute for professional advice. For specific advice, diagnosis and treatment you should consult with a qualified professional. When this packet was developed, Maine Parent Federation made every effort to ensure that the information contained in this packet was accurate, current and reliable. Packets are reviewed and updated periodically as changes occur. 09/2011 Disclaimer The contents of this Information Packet were developed under a grant from the US Department of Education, #H328M110002. However, those contents do not necessarily represent the policy of the US Department of Education, and you should not assume endorsement by the Federal Government. Project Officer, Marsha Goldberg. 1 Distributed by Maine Parent Federation 1-800-870-7746 www.mpf.org 05/2017 Learning Disability Table of Content Learning Disabilities (LD) 3 Supports, Modifications, and Accommodations for Students 10 State Resources 15 National Resources 16 Library Materials 17 2 Distributed by Maine Parent Federation 1-800-870-7746 www.mpf.org 05/2017 Learning Disability Learning Disabilities (LD) A legacy resource from NICHCY Disability Fact Sheet 7 (FS-7) January 2011 | Links updated, July 2015 Sara’s Story When Sara was in the first grade, her teacher started teaching the students how to read. -

CHAPTER-4 Physical Education and Sports for CWSN
CHAPTER-4 Physical Education and Sports for CWSN (Children with Special Needs) 4.1 AIMS & OBJECTIVES OF ADAPTED PHYSICAL EDUCATION Adapted Physical Education is a science of developing, implementing, and monitoring a designed physical education instructional programme for an individual with a disability, based on a comprehensive assessment, to give the learner the skills necessary for a lifetime of rich recreation, leisure and sport experiences to increase physical fitness and wellness. Adapted physical education is physical education that is individualized and specially designed to address the needs of students with disabilities who require adaptations or modifications to be physically active, participate safely, and make progress toward the standards for Health, Safety, and Physical Education. In simple words, we can say the physical education program designed for individuals with disabilities is called adapted physical education. The program is adapted to meet the needs of each student through modifications and accommodations. According to Auxter, D., Pyfer, J. & Huettig, C. “ Adapted physical education is the art and science of developing and implementing a carefully designed physical education instructional program for an individual with a disability, based on a comprehensive assessment, to give the individual the skills necessary for a lifetime of rich leisure, recreation, and sport experiences”. Adapted physical education is used to emphasise the importance of understanding the scientific bases of human development as it bring into relations to teaching appropriate concepts and practices in the adapted physical education program which will serve to maximize the quality of life among individuals with disabilities. Adapted physical education is clear that practices that influencing exercise, fitness, diet and nutritional status can significantly impact the quality and duration of life of an individuals with disabilities. -
IUGR: Intrauterine Growth Restriction
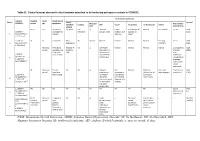
Table S1. Clinical features observed in the 6 patients described so far harboring pathogenic variants in FOXRED1. Evolutionary symptoms Variants Prenatal Onset Onset clinical Patient Lactic/ Survival FOXRED1 period age symptoms Muscular Psychomotor Metabolic Epilepsy MRI Visual Respiratory Cardiovascular Others tone development acidosis IUGR 2m Hypotonia Yes (+++) Yes ↓ Normal Latent Bronchospasm Normal AEP normal IQ: 48 Alive c.920G>A Development refractary (2m,4y,7y3m) strabismus of episodes in (15y) 1 (p.Gly307Glu) / al delay right eye infant c.733+1G>A c.920G>A NI 4y Clumsiness With No Normal Normal Normal Normal Normal Learning IQ: 99 Alive 2 (p.Gly307Glu) / exercise (+) disorders (19y) c.733+1G>A - Neonatal Premature; No (only ↑ Yes ↓ Decreased Normal Normal Normal Normal Gradually loss Alive period Hypoglycemia lactate in attenuation in of motor (22y)) Congenital LCR) the putamen skills; c.694C>T lactic acidosis and cerebellar wheelchair; (p.Gln232X) / 3 atrophy (6y) no expressive c.1289A>G language; 18 (p.Asn430Ser) understands simple commands NI Neonatal Truncal Yes Yes ↓ Delayed Eye Normal Mild non- Persistent Psychomotor Alive period hypotonia myelination movements obstructive left hepatomegaly retardation (10y) c.1054 C>T Poor feeding ventricular have always ventricular (p.Arg352Trp) / dilatation; been roving hypertrophy 4 c.1054 C>T abnormal signal bilateral optic (p.Arg352Trp) 19 in the thalami atrophy and basal ganglia (8m) c.1308G>A ND ND ND ND Yes NA NA NA NA NA NA Severe Alive (p.Val421Met) / psychomotor (¿) 5 c.1308G>A retardation (p.Val421Met)20 IUGR; Neonatal Congenital Yes Yes ↓ Large -- Persistent Dilated right - - Death (3 c.612_615dupA Cerebral period lactic periventricular severe ventricle and months) CTG intraventric acidosis. -

The Disabled People's Movement
The Disabled People’s Movement Book Four A Resource Pack for Local Groups of Disabled People Published by the BCODP The publication of this booklet was made possible by a grant from Charity Projects. First published in 1997 by The British Council of Organisations of Disabled People (BCODP). © BCODP All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means without the prior permission of the publishers and copyright owners except for the quotation of brief passages by reviewers for the public press. Composed by Equal Ability for BCODP Printed by Bailey & Sons Ltd., Somercotes, Derbyshire About this booklet This booklet will not tell you how to run your group, or how to do things. It is designed to signpost you to the information that you need. It will: - Give you ideas about areas you need to think about - Point you in the direction of books and organisations that may help. Some of these books will tell you how to do things. - Fill-in some of the gaps that these books leave about being a group of disabled people. While we were working on these booklets, we talked to many local groups of disabled people. They told us about the hard work and determination you need to succeed. This Resource Pack has been written to help you find support and information so that your hard work does not go to waste. We hope that you will find these signposts get you where you want to go a bit more quickly than you would get there without them! Full details of all books and reference materials mentioned in this booklet is contained in Resource Booklet 6 Introduction What this booklet covers This booklet covers the Disabled People's Movement: • Disability and the Disabled People's Movement • The History of the Movement • International Issues • Integration and inclusion • Campaigning • Self-organisation • BCODP There are some good books that will help you understand more about these subjects. -

Cerebral Hypotonia by Mihee Bay MD (Dr
Cerebral hypotonia By Mihee Bay MD (Dr. Bay of Kennedy Krieger Institute and Johns Hopkins School of Medicine has no relevant financial relationships to disclose.) Originally released July 12, 2006; last updated February 1, 2016; expires February 1, 2019 Introduction This article includes discussion of cerebral hypotonia, central hypotonia, essential hypotonia, benign congenital hypotonia, and floppy infant. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Hypotonia is a clinical manifestation of numerous diseases affecting the central and/or peripheral motor nervous system. The key to accurate diagnosis involves integral steps of evaluation that include a detailed history, examination, and diagnostic tests. “Cerebral” (or central) hypotonia implies pathogenesis from abnormalities from the central nervous system, and related causal disorders include cerebral dysgenesis and genetic or metabolic disorders. Patients with central hypotonia generally have hypotonia without associated weakness, in contrast to the peripheral (lower motor neuron) causes, which typically produce both hypotonia and muscle weakness. Hypotonia is a clinical manifestation of over 500 genetic disorders; thus, a logical, stepwise approach to diagnosis is essential. With recent advances in the field of genetic testing, diagnostic yield will undoubtedly improve. There is no cure, but treatment includes supportive therapies, such as physical and occupational therapy, and diagnosis-specific management. Key points • Hypotonia is reduced tension or resistance of passive range of motion. • The first step in the evaluation of a child with hypotonia is localization to the central (“cerebral”) or peripheral nervous system, or both. • Central hypotonia is more likely to be noted axially with normal strength and hyperactive to normal deep tendon reflexes.