Common Anomalies Associated To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H
Hypotonia and Lethargy in a Two-Day-Old Male Infant Adrienne H. Long, MD, PhD,a,b Jennifer G. Fiore, MD,a,b Riaz Gillani, MD,a,b Laurie M. Douglass, MD,c Alan M. Fujii, MD,d Jodi D. Hoffman, MDe A 2-day old term male infant was found to be hypotonic and minimally abstract reactive during routine nursing care in the newborn nursery. At 40 hours of life, he was hypoglycemic and had intermittent desaturations to 70%. His mother had an unremarkable pregnancy and spontaneous vaginal delivery. The mother’s prenatal serology results were negative for infectious risk factors. Apgar scores were 9 at 1 and 5 minutes of life. On day 1 of life, he fed, stooled, and voided well. Our expert panel discusses the differential diagnosis of hypotonia in a neonate, offers diagnostic and management recommendations, and discusses the final diagnosis. DRS LONG, FIORE, AND GILLANI, birth weight was 3.4 kg (56th PEDIATRIC RESIDENTS percentile), length was 52 cm (87th aDepartment of Medicine, Boston Children’s Hospital, d e percentile), and head circumference Boston, Massachusetts; and Neonatology Section, Medical A 2-day old male infant born at Genetics Section, cDivision of Child Neurology, and 38 weeks and 4 days was found to be was 33 cm (12th percentile). His bDepartment of Pediatrics, Boston Medical Center, Boston, limp and minimally reactive during physical examination at birth was Massachusetts routine care in the newborn nursery. normal for gestational age, with Drs Long, Fiore, and Gillani conceptualized, drafted, Just 5 hours before, he had an appropriate neurologic, cardiac, and and edited the manuscript; Drs Douglass, Fujii, and appropriate neurologic status when respiratory components. -

Orthopedic-Conditions-Treated.Pdf
Orthopedic and Orthopedic Surgery Conditions Treated Accessory navicular bone Achondroplasia ACL injury Acromioclavicular (AC) joint Acromioclavicular (AC) joint Adamantinoma arthritis sprain Aneurysmal bone cyst Angiosarcoma Ankle arthritis Apophysitis Arthrogryposis Aseptic necrosis Askin tumor Avascular necrosis Benign bone tumor Biceps tear Biceps tendinitis Blount’s disease Bone cancer Bone metastasis Bowlegged deformity Brachial plexus injury Brittle bone disease Broken ankle/broken foot Broken arm Broken collarbone Broken leg Broken wrist/broken hand Bunions Carpal tunnel syndrome Cavovarus foot deformity Cavus foot Cerebral palsy Cervical myelopathy Cervical radiculopathy Charcot-Marie-Tooth disease Chondrosarcoma Chordoma Chronic regional multifocal osteomyelitis Clubfoot Congenital hand deformities Congenital myasthenic syndromes Congenital pseudoarthrosis Contractures Desmoid tumors Discoid meniscus Dislocated elbow Dislocated shoulder Dislocation Dislocation – hip Dislocation – knee Dupuytren's contracture Early-onset scoliosis Ehlers-Danlos syndrome Elbow fracture Elbow impingement Elbow instability Elbow loose body Eosinophilic granuloma Epiphyseal dysplasia Ewing sarcoma Extra finger/toes Failed total hip replacement Failed total knee replacement Femoral nonunion Fibrosarcoma Fibrous dysplasia Fibular hemimelia Flatfeet Foot deformities Foot injuries Ganglion cyst Genu valgum Genu varum Giant cell tumor Golfer's elbow Gorham’s disease Growth plate arrest Growth plate fractures Hammertoe and mallet toe Heel cord contracture -

Spinal Dysraphism an Orthopaedic Syndrome in Children Accompanying Occult Forms
Arch Dis Child: first published as 10.1136/adc.35.182.315 on 1 August 1960. Downloaded from SPINAL DYSRAPHISM AN ORTHOPAEDIC SYNDROME IN CHILDREN ACCOMPANYING OCCULT FORMS BY C. C. MICHAEL JAMES and L. P. LASSMAN From the Departments of Orthopaedic Surgery and Neurological Surgery, Newcastle General Hospital, Newcastle upon Tyne (RECEIVED FOR PUBLICATION OCTOBER 19, 1959) Much interest has been shown in the pathology which usually suffer. The treatment in the first of the more gross developmental anomalies of the place is principally in the field of neurosurgery since spinal cord and its coverings and in their clinical the removal of the primary cause, when it is possible, manifestations, most of which are not amenable to demands laminectomy and exploration around the treatment. It has not been appreciated that lesser spinal cord within the dura mater. Subsequent anomalies can also produce disabilities, that they orthopaedic care will be needed only to correct can be diagnosed in life and that they can frequently established deformity if the diagnosis has been be treated by surgery before the secondary effects made late. have become severe and irreversible. Clinical Spinal dysraphism is a term which has been experience over a number of years of the many applied to failure of complete development in the copyright. children sent to orthopaedic clinics with various midline of the dorsal aspect of the embryo. The types of foot or lower limb defect led us to suspect extent of this failure may be of mild, moderate or the presence in some children of a spinal cord severe degree. -

Etiology and Treatment of Congenital Vertical Talus: a Clinical Review Seema Sehmi
REVIEW ARTICLE Etiology and Treatment of Congenital Vertical Talus: A Clinical Review Seema Sehmi ABSTRACT Congenital vertical talus is a rare rigid flat foot deformity. Although the cause of the congenital vertical talus is heterogeneous, recent researches strongly support a genetic cause linking the genes expressed during early limb development. If remain untreated, it causes a lot of disability like pain and functional limitations. Traditional treatment for vertical talus involves extensive surgeries, which are associated with short and long complications. A minimally invasive approach involving serial manipulation and casting will produce excellent short-term results with regard to clinical and radiographic correction. To achieve correction without extensive surgery leading to more flexible and functional foot, a long-term research study is required. Keywords: Clinical, Congenital, Limb, Talus. AMEI’s Current Trends in Diagnosis & Treatment (2020): 10.5005/jp-journals-10055-0102 INTRODUCTION Department of Anatomy, Sri Guru Ram Das Institute of Medical The ankle joint complex involves articulation of talus with tibia and Sciences and Research, Vallah (Amritsar), Punjab, India fibula.1 The movements of the ankle joint are plantar flexion and Corresponding Author: Seema Sehmi, Department of Anatomy, dorsiflexion in sagittal plane and abduction and adduction in the 2 Sri Guru Ram Das Institute of Medical Sciences and Research, Vallah coronal plane. Talus also articulates with plantar calcaneonavicular (Amritsar), Punjab, India, Phone: +91 9914754354, e-mail: drseema16@ 3 ligament and calcaneus to form talocalcaneonavicular joint. gmail.com Congenital vertical talus is a rare foot deformity, which is How to cite this article: Sehmi S. Etiology and Treatment of Congenital characterized by hindfoot valgus and equinus, with associated Vertical Talus: A Clinical Review. -

Hypotonia Surestep Product Catalog Page 29 in Step with Pediatric Hypotonia
SPECIAL EDUCATIONAL SERIES DIAGNOSTIC INSIGHTS ANALYZING GAIT CHANGES GROSS MOTOR SKILLS ORTHOTIC MANAGEMENT CLI N I CAL CASE STUDIES Sponsored by an educational grant from: In Step With Pediatric Hypotonia SureStep Product Catalog Page 29 In Step With Pediatric Hypotonia Contents VIEWPOINT FROM THE EDITOR: An Unexpected Path, Mobility and More an Invaluable Perspective At the most basic level, mobility is about get- PAGE 3 ting from point A to point B. But, for many children with hypotonia, it’s about so much 4 more. FEATURES It’s about independence. It’s about con- fidence. It’s about maintaining strength, fit- ness, and healthy bones. It’s about not being Understanding Hypotonia excluded from activities enjoyed by their PAGE 4 typically developing peers. And improved mobility may have even Gait: The Cornerstone more benefits in those children whose hy- potonia is associated with social and behav- of Intervention ioral developmental delays. New research PAGE 8 has identified an association between motor skills and sociobehavioral milestones in chil- 8 The Importance of Gross dren with autism spectrum disorder, who often present with hypotonia (see “The Im- Motor Skills portance of Gross Motor Skills,” page 12). PAGE 12 This suggests that early intervention to improve gross motor skills—including or- thotic devices and physical therapy—may Orthotic Solutions for also help certain children interact more Children with Hypotonia comfortably with others. That won’t come as PAGE 16 a surprise to the clinicians and parents who 12 have personally seen it happen. This special issue is filled with evidence- Orthotic Success Stories: based information and personal success sto- Four Cases in a Series ries illustrating how effective interventions can enhance mobility in children with hy- PAGE 20 potonia. -

Peds Ortho: What Is Normal, What Is Not, and When to Refer
Peds Ortho: What is normal, what is not, and when to refer Future of Pedatrics June 10, 2015 Matthew E. Oetgen Benjamin D. Martin Division of Orthopaedic Surgery AGENDA • Definitions • Lower Extremity Deformity • Spinal Alignment • Back Pain LOWER EXTREMITY ALIGNMENT DEFINITIONS coxa = hip genu = knee cubitus = elbow pes = foot varus valgus “bow-legged” “knock-knee” apex away from midline apex toward midline normal varus hip (coxa vara) varus humerus valgus ankle valgus hip (coxa valga) Genu varum (bow-legged) Genu valgum (knock knee) bow legs and in toeing often together Normal Limb alignment NORMAL < 2 yo physiologic = reassurance, reevaluate @ 2 yo Bow legged 7° knock knee normal Knock knee physiologic = reassurance, reevaluate in future 4 yo abnormal 10 13 yo abnormal + pain 11 Follow-up is essential! 12 Intoeing 1. Femoral anteversion 2. Tibial torsion 3. Metatarsus adductus MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE! BRACES ARE HISTORY! Femoral Anteversion “W” sitters Internal rotation >> External rotation knee caps point in MOST LIKELY PHYSIOLOGIC AND MAY RESOLVE! Internal Tibial Torsion Thigh foot angle MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE BY SCHOOL AGE Foot is rotated inward Internal Tibial Torsion (Fuchs 1996) Metatarsus Adductus • Flexible = correctible • Observe vs. casting CURVED LATERAL BORDER toes point in NOT TO BE CONFUSED WITH… Clubfoot talipes equinovarus adductus internal varus rotation equinus CAN’T DORSIFLEX cavus Clubfoot START19 CASTING JUST AFTER BIRTH Calcaneovalgus Foot • Intrauterine positioning • Resolve -

Flexible Flatfoot
REVIEW ORTHOPEDICS & TRAUMATOLOGY North Clin Istanbul 2014;1(1):57-64 doi: 10.14744/nci.2014.29292 Flexible flatfoot Aziz Atik1, Selahattin Ozyurek2 1Department of Orthopedics and Tarumatology, Balikesir University Faculty of Medicine, Balikesir, Turkey; 2Department of Orthopedics and Traumatology, Aksaz Military Hospital, Marmaris, Mugla, Turkey ABSTRACT While being one of the most frequent parental complained deformities, flatfoot does not have a universally ac- cepted description. The reasons of flexible flatfoot are still on debate, but they must be differentiated from rigid flatfoot which occurs secondary to other pathologies. These children are commonly brought up to a physician without any complaint. It should be kept in mind that the etiology may vary from general soft tissue laxities to intrinsic foot pathologies. Every flexible flatfoot does not require radiological examination or treatment if there is no complaint. Otherwise further investigation and conservative or surgical treatment may necessitate. Key words: Children; flatfoot; flexible; foot problem; pes planus. hough the term flatfoot (pes planus) is gener- forms again (Figure 2). When weight-bearing forces Tally defined as a condition which the longitu- on feet are relieved this arch can be observed. If the dinal arch of the foot collapses, it has not a clinically foot is not bearing any weight, still medial longitu- or radiologically accepted universal definition. Flat- dinal arch is not seen, then it is called rigid (fixed) foot which we frequently encounter in routine out- flatfoot. To differentiate between these two condi- patient practice will be more accurately seen as a re- tions easily, Jack’s test (great toe is dorisflexed as the sult of laxity of ligaments of the foot. -

Maternal Use of Opioids During Pregnancy and Congenital Malformations: a Systematic Review
Maternal Use of Opioids During Jennifer N. Lind, PharmD, MPH, a, b Julia D. Interrante, MPH, a, c Elizabeth C. Ailes, PhD, MPH, a Suzanne M. Gilboa, PhD, a PregnancySara Khan, MSPH, a, d, e Meghan T. Frey, and MA, MPH, a CongenitalApril L. Dawson, MPH, a Margaret A. Honein, PhD, MPH, a a a, b f, g a Malformations:Nicole F. Dowling, PhD, Hilda Razzaghi, PhD, MSPH, A Andreea Systematic A. Creanga, MD, PhD, Cheryl Review S. Broussard, PhD CONTEXT: abstract Opioid use and abuse have increased dramatically in recent years, particularly OBJECTIVES: among women. We conducted a systematic review to evaluate the association between prenatal DATA SOURCES: opioid use and congenital malformations. We searched Medline and Embase for studies published from 1946 to 2016 and STUDY SELECTION: reviewed reference lists to identify additional relevant studies. We included studies that were full-text journal articles and reported the results of original epidemiologic research on prenatal opioid exposure and congenital malformations. We assessed study eligibility in multiple phases using a standardized, DATA EXTRACTION: duplicate review process. Data on study characteristics, opioid exposure, timing of exposure during pregnancy, congenital malformations (collectively or as individual subtypes), length of RESULTS: follow-up, and main findings were extracted from eligible studies. Of the 68 studies that met our inclusion criteria, 46 had an unexposed comparison group; of those, 30 performed statistical tests to measure associations between maternal opioid use during pregnancy and congenital malformations. Seventeen of these (10 of 12 case-control and 7 of 18 cohort studies) documented statistically significant positive associations. Among the case-control studies, associations with oral clefts and ventricular septal defects/atrial septal defects were the most frequently reported specific malformations. -
IUGR: Intrauterine Growth Restriction
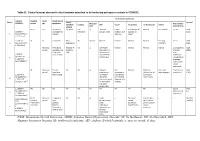
Table S1. Clinical features observed in the 6 patients described so far harboring pathogenic variants in FOXRED1. Evolutionary symptoms Variants Prenatal Onset Onset clinical Patient Lactic/ Survival FOXRED1 period age symptoms Muscular Psychomotor Metabolic Epilepsy MRI Visual Respiratory Cardiovascular Others tone development acidosis IUGR 2m Hypotonia Yes (+++) Yes ↓ Normal Latent Bronchospasm Normal AEP normal IQ: 48 Alive c.920G>A Development refractary (2m,4y,7y3m) strabismus of episodes in (15y) 1 (p.Gly307Glu) / al delay right eye infant c.733+1G>A c.920G>A NI 4y Clumsiness With No Normal Normal Normal Normal Normal Learning IQ: 99 Alive 2 (p.Gly307Glu) / exercise (+) disorders (19y) c.733+1G>A - Neonatal Premature; No (only ↑ Yes ↓ Decreased Normal Normal Normal Normal Gradually loss Alive period Hypoglycemia lactate in attenuation in of motor (22y)) Congenital LCR) the putamen skills; c.694C>T lactic acidosis and cerebellar wheelchair; (p.Gln232X) / 3 atrophy (6y) no expressive c.1289A>G language; 18 (p.Asn430Ser) understands simple commands NI Neonatal Truncal Yes Yes ↓ Delayed Eye Normal Mild non- Persistent Psychomotor Alive period hypotonia myelination movements obstructive left hepatomegaly retardation (10y) c.1054 C>T Poor feeding ventricular have always ventricular (p.Arg352Trp) / dilatation; been roving hypertrophy 4 c.1054 C>T abnormal signal bilateral optic (p.Arg352Trp) 19 in the thalami atrophy and basal ganglia (8m) c.1308G>A ND ND ND ND Yes NA NA NA NA NA NA Severe Alive (p.Val421Met) / psychomotor (¿) 5 c.1308G>A retardation (p.Val421Met)20 IUGR; Neonatal Congenital Yes Yes ↓ Large -- Persistent Dilated right - - Death (3 c.612_615dupA Cerebral period lactic periventricular severe ventricle and months) CTG intraventric acidosis. -

Cerebral Hypotonia by Mihee Bay MD (Dr
Cerebral hypotonia By Mihee Bay MD (Dr. Bay of Kennedy Krieger Institute and Johns Hopkins School of Medicine has no relevant financial relationships to disclose.) Originally released July 12, 2006; last updated February 1, 2016; expires February 1, 2019 Introduction This article includes discussion of cerebral hypotonia, central hypotonia, essential hypotonia, benign congenital hypotonia, and floppy infant. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Hypotonia is a clinical manifestation of numerous diseases affecting the central and/or peripheral motor nervous system. The key to accurate diagnosis involves integral steps of evaluation that include a detailed history, examination, and diagnostic tests. “Cerebral” (or central) hypotonia implies pathogenesis from abnormalities from the central nervous system, and related causal disorders include cerebral dysgenesis and genetic or metabolic disorders. Patients with central hypotonia generally have hypotonia without associated weakness, in contrast to the peripheral (lower motor neuron) causes, which typically produce both hypotonia and muscle weakness. Hypotonia is a clinical manifestation of over 500 genetic disorders; thus, a logical, stepwise approach to diagnosis is essential. With recent advances in the field of genetic testing, diagnostic yield will undoubtedly improve. There is no cure, but treatment includes supportive therapies, such as physical and occupational therapy, and diagnosis-specific management. Key points • Hypotonia is reduced tension or resistance of passive range of motion. • The first step in the evaluation of a child with hypotonia is localization to the central (“cerebral”) or peripheral nervous system, or both. • Central hypotonia is more likely to be noted axially with normal strength and hyperactive to normal deep tendon reflexes. -

On the Inheritance of Hand and Foot Anomalies in Six Families
On the Inheritance of Hand and Foot Anomalies in Six Families OLA JOHNSTON AND RALPH WALDO DAVIS Department of Biology, North Texas State College, Denton, Texas INTRODUCTION Malformations of the hands and feet are common and of many kinds. Ac- cording to Gates (1946) there probably are more abnormalities of the hands and feet than of any other part of the body, with the exception of the eye. It is true that some hand and foot anomalies are the result of accident and disease but it is equally true that many are the result of variation in heredity. The extent to which the latter is true and the mode of inheritance of those variations which have some genetic basis are questions which are not com- pletely answered. Hence when an opportunity presented itself to study a number of different hand and foot anomalies which appeared to have a he- reditary basis, it seemed worthwhile to investigate them and to present the findings. The malformations which are included are syndactyly and split hand and foot, polydactyly, and brachydactyly. Each will be considered more or less independently and in the order indicated. A BRIEF REVIEW OF LITERATURE 1. Syndactyly and Split Hand and Foot Syndactyly is the condition in which two or more fingers or toes are adherent or are more or less completely grown together. Split hand and foot (also called lobster claw) is a deformity in which the central digits of the hands and/or feet are lacking. It may represent an extreme variant of syndactyly. According to Lewis (1909) a description of split hand and foot is difficult because of the great variation in the deformity even within the same family. -

Prevalence and Associated Factors of Flat Feet Among Patients With
Arch Physiother Rehabil 2020; 3 (4): 076-083 DOI: 10.26502/fapr0016 Research Article Prevalence and Associated Factors of Flat Feet among Patients with Hypertension; Findings from a Cross Sectional Study Carried Out at a Tertiary Care Hospital in Sri Lanka Jithmi N Samarakoon1, Nipun Lakshitha de Silva2, Deepika Fernando3* 1Department of Allied Health Sciences, Faculty of Medicine, Colombo, Sri Lanka 2Department of Clinical Sciences, Faculty of Medicine, General Sir John Kotelawala Defence University, Ratmalana, Sri Lanka 3Department of Parasitology, Faculty of Medicine, Colombo, Sri Lanka *Corresponding author: Deepika Fernando, Department of Parasitology, Faculty of Medicine, Colombo, 00800, Sri Lanka, Tel: +94717229509; E-mail: [email protected] Received: 24 October 2020; Accepted: 03 November 2020; Published: 05 November 2020 Citation: Jithmi N Samarakoon, Nipun Lakshitha de Silva, Deepika Fernando. Prevalence and Associated Factors of Flat Feet among Patients with Hypertension; Findings from a Cross Sectional Study Carried Out at a Tertiary Care Hospital in Sri Lanka. Archives of Physiotherapy and Rehabilitation 3 (2020): 076-083. Abstract recognized risk factors were enrolled. Socio- Background: Hypertension is considered a risk factor demographic details and clinical information were for flat feet as it causes posterior tibial tendon collected using a pre-tested interviewer administered dysfunction. The objectives of this study were to questionnaire. Arch index was obtained by a static identify the prevalence and associated factors of flat feet footprint on the Harris mat. Body weight and height among patients with hypertension. were measured using standard instruments. Body Mass Index was calculated. Descriptive statistics, Independent Methods: A cross sectional study with systematic t- test, Chi-square test and Pearson correlation were sampling was done in three selected hypertension used for data analysis.