Committee for Veterinary Medicinal Products
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

A Brief History Behind the Most Used Local Anesthetics
Tetrahedron xxx (xxxx) xxx Contents lists available at ScienceDirect Tetrahedron journal homepage: www.elsevier.com/locate/tet Tetrahedron report XXX A brief history behind the most used local anesthetics * Marco M. Bezerra, Raquel A.C. Leao,~ Leandro S.M. Miranda, Rodrigo O.M.A. de Souza Biocatalysis and Organic Synthesis Group, Chemistry Institute, Federal University of Rio de Janeiro, 21941-909, Brazil article info abstract Article history: The chemistry behind the discovery of local anesthetics is a beautiful way of understanding the devel- Received 13 April 2020 opment and improvement of medicinal/organic chemistry protocols towards the synthesis of biologically Received in revised form active molecules. Here in we present a brief history based on the chemistry development of the most 16 September 2020 used local anesthetics trying to draw a line between the first achievements obtained by the use of Accepted 18 September 2020 cocaine until the synthesis of the mepivacaine analogs nowadays. Available online xxx © 2020 Elsevier Ltd. All rights reserved. Keywords: Anesthetics Medicinal chemistry Organic synthesis Mepivacaíne Contents 1. Introduction . ............................. 00 1.1. Pain and anesthesia . ............................................... 00 1.2. Ancient techniques to achieve anesthesia . ............................... 00 1.3. The objective of this work . .......................................... 00 2. Cocaine .............................................................................................. ............................ -

Anaesthetic Antacids: a Review of Its Pharmacological Properties and Therapeutic Efficacy
International Journal of Research in Medical Sciences Parakh RK et al. Int J Res Med Sci. 2018 Feb;6(2):383-393 www.msjonline.org pISSN 2320-6071 | eISSN 2320-6012 DOI: http://dx.doi.org/10.18203/2320-6012.ijrms20180005 Review Article Anaesthetic antacids: a review of its pharmacological properties and therapeutic efficacy Rajendra Kumar Parakh*, Neelakanth S. Patil Department of Medicine, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India Received: 13 December 2017 Accepted: 27 December 2017 *Correspondence: Dr. Rajendra Kumar Parakh, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Anaesthetic antacids, combination of antacids (Aluminium hydroxide, Magnesium hydroxide) with an anaesthetic (oxethazaine), is becoming a choice of physicians and is re-emerging across all types of GI disorders (esophagitis, peptic ulcer, duodenal ulcer, heartburn, gastritis, functional dyspepsia), despite the discovery of potent and efficacious acid suppressants like H2 receptor blockers and proton pump inhibitors (PPIs). The reason being that anaesthetic antacids increase the gastric pH and provide relief from pain for a longer period of duration at considerably a lower dosage. Furthermore, it significantly increases the duration between the time of medication and the peak pH as compared to antacid alone. Oxethazaine, an anaesthetic component, produces a reversible loss of sensation and provides a prompt and prolonged relief of pain, thereby broadening the therapeutic spectrum of antacids. -

Bicillin CR (Penicillin G Benzathine and Penicillin
® Bicillin C-R (penicillin G benzathine and penicillin G procaine injectable suspension) Disposable Syringe for deep IM injection only WARNING: NOT FOR INTRAVENOUS USE. DO NOT INJECT INTRAVENOUSLY OR ADMIX WITH OTHER INTRAVENOUS SOLUTIONS. THERE HAVE BEEN REPORTS OF INADVERTENT INTRAVENOUS ADMINISTRATION OF PENICILLIN G BENZATHINE WHICH HAS BEEN ASSOCIATED WITH CARDIORESPIRATORY ARREST AND DEATH. Prior to administration of this drug, carefully read the WARNINGS, ADVERSE REACTIONS, and DOSAGE AND ADMINISTRATION sections of the labeling. To reduce the development of drug-resistant bacteria and maintain the effectiveness of Bicillin C-R and other antibacterial drugs, Bicillin C-R should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Bicillin C-R (penicillin G benzathine and penicillin G procaine injectable suspension) contains equal amounts of the benzathine and procaine salts of penicillin G. It is available for deep intramuscular injection. Penicillin G benzathine is prepared by the reaction of dibenzylethylene diamine with two molecules of penicillin G. It is chemically designated as (2S,5R,6R)-3,3-Dimethyl-7-oxo-6-(2 phenylacetamido)-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid compound with N,N’ dibenzylethylenediamine (2:1), tetrahydrate. It occurs as a white, crystalline powder and is very slightly soluble in water and sparingly soluble in alcohol. Its chemical structure is as follows: Reference ID: 3832113 Penicillin G procaine, (2S,5R,6R)-3,3-Dimethyl-7-oxo-6-(2-phenylacetamido)-4-thia-1 azabicyclo[3.2.0]heptane-2-carboxylic acid compound with 2-(diethylamino)ethyl p aminobenzoate (1:1) monohydrate, is an equimolar salt of procaine and penicillin G. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

The Selection and Use of Essential Medicines
WHO Technical Report Series 958 THE SELECTION AND USE OF ESSENTIAL MEDICINES This report presents the recommendations of the WHO Expert THE SELECTION AND USE Committee responsible for updating the WHO Model List of Essential Medicines. The fi rst part contains a review of the OF ESSENTIAL MEDICINES report of the meeting of the Expert Subcommittee on the Selection and Use of Essential Medicines, held in October 2008. It also provides details of new applications for paediatric medicines and summarizes the Committee’s considerations and justifi cations for additions and changes to the Model List, including its recommendations. Part Two of the publication is the report of the second meeting of the Subcommittee of the Expert Committee on the Selection and Use of Essential Medicines. Annexes include the revised version of the WHO Model List of Essential Medicines (the 16th) and the revised version of the WHO Model List of Report of the WHO Expert Committee, 2009 Essential Medicines for Children (the 2nd). In addition there is a list of all the items on the Model List sorted according to their (including the 16th WHO Model List of Essential Medicines Anatomical Therapeutic Chemical (ATC) classifi cation codes. and the 2nd WHO Model List of Essential Medicines for Children) WHO Technical Report Series — 958 WHO Technical ISBN 978-92-4-120958-8 Geneva TTRS958cover.inddRS958cover.indd 1 110.06.100.06.10 008:328:32 The World Health Organization was established in 1948 as a specialized agency of the United Nations serving as the directing and coordinating authority for SELECTED WHO PUBLICATIONS OF RELATED INTEREST international health matters and public health. -

Veterinary Medicines
VETERINARY MEDICINES A compact collection of information on Veterinary drugs/medicines in practice Prepared By : Dr. ANWAR ALAM KHAN eMail and FaceBook : [email protected] Sep-2013 CHAPTERS 1 Gastrointestinal & Hepatobiliary System 2 Infection and Infestations 3 Cardiovascular System 4 Nervous System 5 Respiratory System 6 Allergic Disorders 7 Urinary System 8 Genital System 9 Eye & Ear 10 Topical Applications 11 Nutrition and Metabolism 12 Exclusive Formulations 13 Surgical 14 Livestock Biologicals 15 Diagnostics 16 Ayurvedics Page 2 1...Gastrointestinal & Hepatobiliary System GASTROINTESTINAL & HEPATOBILIARY SYSTEM Antemetics PROMETHAZINE Phenothiazines. Anti-Histaminic, H1 receptar antagonist Phenergan NPIL Promethazine inj 2ml Dog 1-2ml--IM or Nausea, Vomition Slow-IV syp 60 ml tab 10mg Dog 25mg DOMPERIDONE Dopamine receptar Antagonist Domstal Torrent Domperidone drops 5 ml Dog Puppies, 2--3 Nausea, Vomiting. drops susp 30 ml Dog 5-10 ml orally tab 5,10,20 mg Dog 1-2 tab before meals Vomistop Cipla Domperidone drops 30ml Dog 5-10 ml tab 10mg Dog 1-2 tab METACLOPRAMIDE Perinorm IPCA Metaclopramide inj 2ml, 10ml Dog 0.05~2ml--IV Nausia, Vomition liq 30 ml Dog 5-10 ml tab 5mg, 10mg, Dog 5-10 mg DT-5mg ONDANESTRON Belongs to the class of serotonin (5HT3) antagonists Emeset Cipla Ondanestron inj 2ml, 4ml Dog 2-4 ml Nausea, Vomiting syp 30 ml Dog 5-10 ml orally tab 4mg, 8mg Dog 4mg, 8mg Ondem Alkem Ondanestron inj 2ml, 4ml Dog 1--2 ml, IM Nausea, Vomiting (2mg/ml) susp 30 ml Dog Page 3 1...Gastrointestinal & Hepatobiliary System Antacids, -
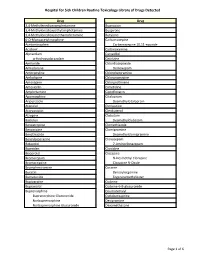
Page 1 S C Routine Toxicology Library Drug 3,4
Hospital for Sick Children Routine Toxicology Library of Drugs Detected Drug Drug 3,4-Methylenedioxyamphetamine Bupropion 3,4-Methylenedioxyethylamphetamine Buspirone 3,4-Methylenedioxymethamphetamine Butylone 6-O-Monoacetylmorphine Carbamazepine Acetaminophen Carbamazepine 10,11-epoxide Aciclovir Carbinoxamine Alprazolam Carvedilol α-Hydroxyalprazolam Cetirizine Amiloride Chlordiazepoxide Amiodarone Demoxepam Amitriptyline Chlorpheniramine Amlodipine Chlorpromazine Amoxapine Chlorprothixene Amoxicillin Cimetidine Amphetamine Ciprofloxacin Apomorphine Citalopram Aripiprazole Desmethylcitalopram Atenolol Clemastine Atorvastatin Clenbuterol Atropine Clobazam Baclofen Desmethylclobazam Benzatropine Clomethiazole Benzocaine Clomipramine Benzthiazide Desmethylclomipramine Benzylpiperazine Clonazepam Betaxolol 7-Aminoclonazepam Biperiden Clonidine Bisoprolol Clozapine Bromazepam N-Desmethyl Clozapine Bromocriptine Clozapine N-Oxide Brompheniramine Cocaine Bucetin Benzoylecgonine Bumetanide Ecgoninemethylester Bupivacaine Codeine Bupranolol Codeine-6-B-glucuronide Buprenorphine Coumatetralyl Buprenorphine Glucuronide Cyclobenzaprine Norbuprenorphine Desipramine Norbuprenorphine Glucuronide Dexamethasone Page 1 of 6 Hospital for Sick Children Routine Toxicology Library of Drugs Detected Drug Drug Dextromethorphan Fluoxetine Dextrorphan Norfluoxetine Diazepam Fluphenazine Nordiazepam Flurazepam 4-Hydroxynordiazepam Desalkylflurazepam Diclofenac 2-Hydroxyethylflurazepam Dihydrocodeine Fluvoxamine Dihydrocodeine-6-β-glucuronide Gabapentin Dihydroergotamine -

Review of Existing Classification Efforts
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.1.1 Review of existing classification efforts Due date of deliverable: (15.01.2008) Actual submission date: (07.02.2008) Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UGent Revision 1.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public X PP Restricted to other programme participants (including the Commission Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) Task 4.1 : Review of existing classification efforts Authors: Kristof Pil, Elke Raes, Thomas Van den Neste, An-Sofie Goessaert, Jolien Veramme, Alain Verstraete (Ghent University, Belgium) Partners: - F. Javier Alvarez (work package leader), M. Trinidad Gómez-Talegón, Inmaculada Fierro (University of Valladolid, Spain) - Monica Colas, Juan Carlos Gonzalez-Luque (DGT, Spain) - Han de Gier, Sylvia Hummel, Sholeh Mobaser (University of Groningen, the Netherlands) - Martina Albrecht, Michael Heiβing (Bundesanstalt für Straßenwesen, Germany) - Michel Mallaret, Charles Mercier-Guyon (University of Grenoble, Centre Regional de Pharmacovigilance, France) - Vassilis Papakostopoulos, Villy Portouli, Andriani Mousadakou (Centre for Research and Technology Hellas, Greece) DRUID 6th Framework Programme Deliverable D.4.1.1. Revision 1.0 Review of Existing Classification Efforts Page 2 of 127 Introduction DRUID work package 4 focusses on the classification and labeling of medicinal drugs according to their influence on driving performance. -

Production of Gel with Menthol, Benzocaine and Procaine Hcl for Topical Application in Rheumatoid Arthritis Patients
Journal of Pharmacy and Pharmacology 5 (2017) 245-248 doi: 10.17265/2328-2150/2017.05.003 D DAVID PUBLISHING Production of Gel with Menthol, Benzocaine and Procaine HCl for Topical Application in Rheumatoid Arthritis Patients B. Angelovska1, S. Maleska-Stojadinovikj2, E. Drakalska1 and B. Gjorgjeska1 1. Facutly of medical sciences, University “Goce Delcev”-Stip, Stip 2000, R. Macedonia 2. Public Hospital-Ohrid, R. Macedonia,-“Dimitar Vlahov” Ohrid, 33- 6000, R.Macedonia Abstract: Antirheumatic and analgesics drugs are the most commonly prescribed medications for treatment of acute and chronic pain. Frequent application of these agents often causes adverse effects. So, in order to avoid the incidence of side effects, topical analgesics are treatment of choice for localized muscle pain. Topical analgesics offer the potential to provide the same analgesic relief provided by oral analgesics but with minimal adverse systemic effects. The aim of this study is to present the preparation and characterization of topical analgesic gel named “Russian water”. Gel is composed of Menthol, Benzocaine, Procaine HCl as topical analgesic agents indicated for temporary relief of pain. Obtained results showed prolonged analgesic effect compared with liquid ethanol solution composed of the same components. Key words: Pain, gel, Russian water, antirheumatic, analgesic. 1. Introduction According to the health requirements, the preparation of pharmaceutical dosage formed in a Antirheumatic and analgesics drugs are the most galenic laboratory, mainly aims to provide a dosage commonly used agents to treat diseases of the form, which is designed as an opportunity for changes musculoskeletal system and to alleviate all sorts of in the composition and consistency of the product.