Management of Odontogenic Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Anatomical Overview
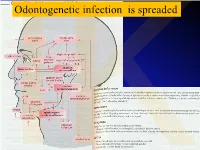
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Head & Neck Surgery Course
Head & Neck Surgery Course Parapharyngeal space: surgical anatomy Dr Pierfrancesco PELLICCIA Pr Benjamin LALLEMANT Service ORL et CMF CHU de Nîmes CH de Arles Introduction • Potential deep neck space • Shaped as an inverted pyramid • Base of the pyramid: skull base • Apex of the pyramid: greater cornu of the hyoid bone Introduction • 2 compartments – Prestyloid – Poststyloid Anatomy: boundaries • Superior: small portion of temporal bone • Inferior: junction of the posterior belly of the digastric and the hyoid bone Anatomy: boundaries Anatomy: boundaries • Posterior: deep fascia and paravertebral muscle • Anterior: pterygomandibular raphe and medial pterygoid muscle fascia Anatomy: boundaries • Medial: pharynx (pharyngobasilar fascia, pharyngeal wall, buccopharyngeal fascia) • Lateral: superficial layer of deep fascia • Medial pterygoid muscle fascia • Mandibular ramus • Retromandibular portion of the deep lobe of the parotid gland • Posterior belly of digastric muscle • 2 ligaments – Sphenomandibular ligament – Stylomandibular ligament Aponeurosis and ligaments Aponeurosis and ligaments • Stylopharyngeal aponeurosis: separates parapharyngeal spaces to two compartments: – Prestyloid – Poststyloid • Cloison sagittale: separates parapharyngeal and retropharyngeal space Aponeurosis and ligaments Stylopharyngeal aponeurosis Muscles stylohyoidien Stylopharyngeal , And styloglossus muscles Prestyloid compartment Contents: – Retromandibular portion of the deep lobe of the parotid gland – Minor or ectopic salivary gland – CN V branch to tensor -

Deep Neck Infections 55
Deep Neck Infections 55 Behrad B. Aynehchi Gady Har-El Deep neck space infections (DNSIs) are a relatively penetrating trauma, surgical instrument trauma, spread infrequent entity in the postpenicillin era. Their occur- from superfi cial infections, necrotic malignant nodes, rence, however, poses considerable challenges in diagnosis mastoiditis with resultant Bezold abscess, and unknown and treatment and they may result in potentially serious causes (3–5). In inner cities, where intravenous drug or even fatal complications in the absence of timely rec- abuse (IVDA) is more common, there is a higher preva- ognition. The advent of antibiotics has led to a continu- lence of infections of the jugular vein and carotid sheath ing evolution in etiology, presentation, clinical course, and from contaminated needles (6–8). The emerging practice antimicrobial resistance patterns. These trends combined of “shotgunning” crack cocaine has been associated with with the complex anatomy of the head and neck under- retropharyngeal abscesses as well (9). These purulent col- score the importance of clinical suspicion and thorough lections from direct inoculation, however, seem to have a diagnostic evaluation. Proper management of a recog- more benign clinical course compared to those spreading nized DNSI begins with securing the airway. Despite recent from infl amed tissue (10). Congenital anomalies includ- advances in imaging and conservative medical manage- ing thyroglossal duct cysts and branchial cleft anomalies ment, surgical drainage remains a mainstay in the treat- must also be considered, particularly in cases where no ment in many cases. apparent source can be readily identifi ed. Regardless of the etiology, infection and infl ammation can spread through- Q1 ETIOLOGY out the various regions via arteries, veins, lymphatics, or direct extension along fascial planes. -

Nontraumatic Head and Neck Injuries: a Clinical Approach. Part 2 183
Radiología. 2017;59(3):182---195 www.elsevier.es/rx UPDATE IN RADIOLOGY Nontraumatic head and neck injuries: A clinical ଝ approach. Part 2 ∗ B. Brea Álvarez , L. Esteban García, M. Tunón˜ Gómez, Y. Cepeda Ibarra Hospital Universitario Puerta de Hierro-Majadahonda, Majadahonda, Madrid, Spain Received 3 May 2016; accepted 16 February 2017 KEYWORDS Abstract Nontraumatic emergencies of the head and neck represent a challenge in the field of Emergencies; neuroradiology for two reasons. As explained in the first part of this update, these entities affect Neck injuries; an area where the thorax joins the cranial cavity and can thus compromise both structures; Orbital diseases; second, they are uncommon, so they are not well known. Diseases of the Maintaining the same approach as in the first part, focusing on the clinical presentations in the paranasal sinus; emergency department rather than on the anatomic regions affected, we will study the entities Sialadenitis; that present with two patterns: those that present with a combination of cervical numbness, Cellulitis; dysphagia, and dyspnoea and those that present with acute sensory deficits. In the latter group, Diagnostic imaging; we will specifically focus on visual deficits, because this is the most common symptom that calls Computed for urgent imaging studies. tomography; © 2017 SERAM. Published by Elsevier Espana,˜ S.L.U. All rights reserved. Magnetic resonance imaging PALABRAS CLAVE Urgencias no traumáticas de cabeza y cuello: aproximación desde la clínica. Parte 2 Urgencias; Resumen Las urgencias no traumáticas de cabeza y cuello son un reto en el campo neurorra- Lesiones del cuello; Enfermedades diológico por los motivos referidos en la primera parte: su área de afectación, en la encrucijada orbitarias; del tórax y la cavidad craneal, y su baja incidencia en la urgencia, lo que supone que sean poco conocidas. -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

Acute Fascial Space Abscess Upon Dental Implantation to Patients with Diabetes Mellitus
CASE REPORT J Korean Dent Sci. 2015;8(2):89-94 http://dx.doi.org/10.5856/JKDS.2015.8.2.89 ISSN 2005-4742 Acute Fascial Space Abscess upon Dental Implantation to Patients with Diabetes Mellitus Chae Yoon Lee, Baek Soo Lee, Yong Dae Kwon, Joo Young Oh, Jung Woo Lee, Suk Huh, Byeong Joon Choi Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyung Hee University, Seoul, Korea As popularity of dental implantation is increasing, the number of cases associated with complications also increase. Evaluation on diabetes mellitus is often neglected due to the disease's irrelevance to implantability. However, patients with diabetes mellitus are susceptible to infection due to impaired bactericidal ability of neutrophils, cellular immunity and activity of complements. Due to this established connection between diabetes mellitus and infection, a couple of cases were selected to present patients with diabetes mellitus with glycemic incontrollability, suffering from post-implantation dentigerous inter-fascial space abscess. Key Words: Deep neck abscess; Diabetes mellitus; Implant complication; Klebsiella pneumoniae Introduction to other conditions involved with administration of anticoagulant formulation and bisphosphonate As popularity of dental implantation is increasing, formulation associated with bisphosphonate-related the number of cases associated with complications osteonecrosis of the jaw (BRONJ) which have direct also increase. While there are plenty of researches association with implantability. on locally manifested etiological causes of dental Being the most common systemic disease affecting implant failure, systemic causes have barely been infection of deep neck, diabetes mellitus hinders studied and reported. In clinical settings, there is immunity1) and causes prolonged healingwith poor insufficient evaluation of systemic factors prior to prognosis1). -

Neck Formation and Growth. MAIN TOPOGRAPHIC REGIONS in NECK
Neck formation and growth. MAIN TOPOGRAPHIC REGIONS IN NECK. ANATOMICAL BACKGROUND FOR URGENT LIFE SAVING PERFORMANCES. orofac Ivo Klepáček orofac Vymezení oblasti krku Extent of the neck region Sensitivní oblasti V1, V2, V3., plexus cervicalis orofac * * * * * orofac** * orofac orofac orofaccranial middle caudal orofac orofac Clinical classification of neck lymph nodes orofacClinical classification of neck lymphatic nodes: I - VI Nodi lymphatici out of regiones above: Perifacial, periparotic, retroauricular, suboccipital, retropharyngeal Metastasa v krčních uzlinách Metastasis in cervical orofaclymphonodi TOPOGRAPHIC REGIONS orofacand SPACES Regio colli anterior anterior neck triangle Trigonae : submentale, submandibulare, caroticum (musculare), regio suprasternalis Triangles : submental, submandibular, carotic (muscular), orofacsuprasternal region podkožní sval na povrchové krční fascii r. colli nervi facialis ovládá napětí kůže krku Platysma orofac proc. mastoideus manubrium sterni, clavicula Sternocleidomastoid m. n.accessorius (XI) + branches sternocleidomastoideus from plexus cervicalis orofac Punctum nervosum (Erb ´s point) : there C5 and C6 nerves are connected, + branches from suprascapulari and subclavian nerves orofacWilhelm Heinrich Erb (1840 - 1921), German neurologist orofac orofac mm. suprahyoid suprahyoidei and et mm. infrahyoid orofacinfrahyoidei muscles orofac Thyroid gland and vascular + nerve bundle in neck orofac orofac Žíly veins orofac štítná žláza příštitné orofactělísko a. thyroidea inferior n. laryngeus inferior -

Shifteh Retropharyngeal Danger and Paraspinal Spaces ASHNR 2016
Acknowledgment • Illustrations Courtesy Amirsys, Inc. Retropharyngeal, Danger, and Paraspinal Spaces Keivan Shifteh, M.D. Professor of Clinical Radiology Director of Head & Neck Imaging Program Director, Neuroradiology Fellowship Montefiore Medical Center Albert Einstein College of Medicine Bronx, New York Retropharyngeal, Danger, and Retropharyngeal Space (RPS) Paraspinal Spaces • It is a potential space traversing supra- & infrahyoid neck. • Although diseases affecting these spaces are relatively uncommon, they can result in significant morbidity. • Because of the deep location of these spaces within the neck, lesions arising from these locations are often inaccessible to clinical examination but they are readily demonstrated on CT and MRI. • Therefore, cross-sectional imaging plays an important role in the evaluation of these spaces. Retropharyngeal Space (RPS) Retropharyngeal Space (RPS) • It is seen as a thin line of fat between the pharyngeal • It is bounded anteriorly by the MLDCF (buccopharyngeal constrictor muscles anteriorly and the prevertebral fascia), posteriorly by the DLDCF (prevertebral fascia), and muscles posteriorly. laterally by sagittaly oriented slips of DLDCF (cloison sagittale). Alar fascia (AF) Retropharyngeal Space • Coronally oriented slip of DLDCF (alar fascia) extends from • The anterior compartment is true or proper RPS and the the medial border of the carotid space on either side and posterior compartment is danger space. divides the RPS into 2 compartments: Scali F et al. Annal Otol Rhinol Laryngol. 2015 May 19. Retropharyngeal Space Danger Space (DS) • The true RPS extends from the clivus inferiorly to a variable • The danger space extends further inferiorly into the posterior level between the T1 and T6 vertebrae where the alar fascia mediastinum just above the diaphragm. -

Rare Case of Plunging Ranula with Parapharyngeal Extension and Absent Submandibular Gland: Excision by Transcervical Approach
Central Journal of Ear, Nose and Throat Disorders Bringing Excellence in Open Access Case Report *Corresponding author Abhishek Bhardwaj, Department of Otorhinolaryngology, Safdarjung Hospital Rare Case of Plunging Ranula &Vardhmann Mahavir Medical College, Ansari Nagar, New Delhi-110029, India, Tel: 91-989907792; Email: with Parapharyngeal Extension Submitted: 04 January 2017 Accepted: 29 March 2017 and Absent Submandibular Published: 31 March 2017 ISSN: 2475-9473 Copyright Gland: Excision by Transcervical © 2017 Bhardwaj et al. Approach OPEN ACCESS Keywords Abhishek Bhardwaj*, Sudhagar Eswaran, and Hari Shankar • Ranula Niranjan • Submandibular gland Department of Otorhinolaryngology, Vardhmann Mahavir Medical College and • Pharynx Safdarjung Hospital, India • Skull Base • Neck Abstract Plunging ranula extending into parapharyngeal space till the skull base with associated absence of submandibular gland is a rare finding. Transcervical approach for its excision is a challenging procedure in view of limited exposure and presence of important neurovascular structures in the field. We present a clinical case of a left sided plunging ranula extending into the parapharyngeal space till skull base in a 19 year old male who presented to a tertiary care hospital with complaints of slowly increasing swelling in neck and oral cavity for duration of six months. Ultrasound neck revealed well defined heterogeneously hypoechoic collection in left submandibular region. Contrast enhanced computed tomography revealed a non-enhancing, cystic mass involving left submandibular space extending into left parapharyngeal space till skull base and absent left submandibular gland. Ranula measuring 10cm*6cm was excised in to by tanscervical approach without damage to any neurovascular structure. Histopathology was consistent with low ranula. Patient is in follow up for past six months without any recurrence. -

Deep Neck Space Infectionsdeep Neck Space Infections
Deep Neck Space InfectionsDeep Neck Space Infections Disclaimer: The pictures used in this presentation and its content has been obtained from a number of sources. Their use is purely for academic and teaching purposes. The contents of this presentation do not have any intended commercial use. In case the owner of any of the pictures has any objection and seeks their removal please contact at [email protected] . These pictures will be removed immediately. The fibrous connective tissue that constitutes the cervical fascia varies from loose areolar tissue to dense fibrous bands. This fascia serves to envelope the muscles, nerves, vessels and viscera of the neck, thereby forming planes and potential spaces that serve to divide the neck into functional units. It functions to both direct and limit the spread of disease processes in the neck. The cervical fascia can be divided into a simpler superficial layer and a more complex deep layer that is further subdivided into superficial, middle and deep layers. The superficial layer of cervical fascia ensheaths the platysma in the neck and extends superiorly in the face to cover the mimetic muscles. It is the equivalent of subcutaneous tissue elsewhere in the body and forms a continuous sheet from the head and neck to the chest, shoulders and axilla. The superficial layer of the deep cervical fascia is also known as the investing layer. It follows the “rule of twos”—it envelops two muscles, two glands and forms two spaces. It originates from the spinous processes of the vertebral column and spreads circumferentially around the neck. -

Fascia and Spaces on the Neck: Myths and Reality Fascije I Prostori Vrata: Mit I Stvarnost
Review/Pregledni članak Fascia and spaces on the neck: myths and reality Fascije i prostori vrata: mit i stvarnost Georg Feigl* Institute of Anatomy, Medical University of Graz, Graz, Austria Abstract. The ongoing discussion concerning the interpretation of existing or not existing fas- ciae on the neck needs a clarification and a valid terminology. Based on the dissection experi- ence of the last four decades and therefore of about 1000 cadavers, we investigated the fas- cias and spaces on the neck and compared it to the existing internationally used terminology and interpretations of textbooks and publications. All findings were documented by photog- raphy and the dissections performed on cadavers embalmed with Thiel´s method. Neglected fascias, such as the intercarotid fascia located between both carotid sheaths and passing be- hind the visceras or the Fascia cervicalis media as a fascia between the two omohyoid mus- cles, were dissected on each cadaver. The ”Danger space” therefore was limited by fibrous walls on four sides at level of the carotid triangle. Ventrally there was the intercarotid fascia, laterally the alar fascia, and dorsally the prevertebral fascia. The intercarotid fascia is a clear fibrous wall between the Danger Space and the ventrally located retropharyngeal space. Lat- ter space has a continuation to the pretracheal space which is ventrally limited by the middle cervical fascia. The existence of an intercarotid fascia is crucial for a correct interpretation of any bleeding or inflammation processes, because it changes the topography of the existing spaces such as the retropharyngeal or “Danger space” as well. As a consequence, the existing terminology should be discussed and needs to be adapted. -

Complex Odontogenic Infections
Complex Odontogenic Infections Larry ). Peterson CHAPTEROUTLINE FASCIAL SPACE INFECTIONS Maxillary Spaces MANDIBULAR SPACES Secondary Fascial Spaces Cervical Fascial Spaces Management of Fascial Space Infections dontogenic infections are usually mild and easily and causes infection in the adjacent tissue. Whether or treated by antibiotic administration and local sur- not this becomes a vestibular or fascial space abscess is 0 gical treatment. Abscess formation in the bucco- determined primarily by the relationship of the muscle lingual vestibule is managed by simple intraoral incision attachment to the point at which the infection perfo- and drainage (I&D) procedures, occasionally including rates. Most odontogenic infections penetrate the bone dental extraction. (The principles of management of rou- in such a way that they become vestibular abscesses. tine odontogenic infections are discussed in Chapter 15.) On occasion they erode into fascial spaces directly, Some odontogenic infections are very serious and require which causes a fascial space infection (Fig. 16-1). Fascial management by clinicians who have extensive training spaces are fascia-lined areas that can be eroded or dis- and experience. Even after the advent of antibiotics and tended by purulent exudate. These areas are potential improved dental health, serious odontogenic infections spaces that do not exist in healthy people but become still sometimes result in death. These deaths occur when filled during infections. Some contain named neurovas- the infection reaches areas distant from the alveolar cular structures and are known as coinpnrtments; others, process. The purpose of this chapter is to present which are filled with loose areolar connective tissue, are overviews of fascial space infections of the head and neck known as clefts.