Nonexcisional, Minimally Invasive Rejuvenation of the Neck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Anatomical Overview
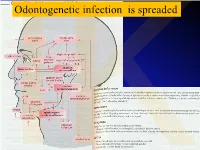
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

Acute Fascial Space Abscess Upon Dental Implantation to Patients with Diabetes Mellitus
CASE REPORT J Korean Dent Sci. 2015;8(2):89-94 http://dx.doi.org/10.5856/JKDS.2015.8.2.89 ISSN 2005-4742 Acute Fascial Space Abscess upon Dental Implantation to Patients with Diabetes Mellitus Chae Yoon Lee, Baek Soo Lee, Yong Dae Kwon, Joo Young Oh, Jung Woo Lee, Suk Huh, Byeong Joon Choi Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyung Hee University, Seoul, Korea As popularity of dental implantation is increasing, the number of cases associated with complications also increase. Evaluation on diabetes mellitus is often neglected due to the disease's irrelevance to implantability. However, patients with diabetes mellitus are susceptible to infection due to impaired bactericidal ability of neutrophils, cellular immunity and activity of complements. Due to this established connection between diabetes mellitus and infection, a couple of cases were selected to present patients with diabetes mellitus with glycemic incontrollability, suffering from post-implantation dentigerous inter-fascial space abscess. Key Words: Deep neck abscess; Diabetes mellitus; Implant complication; Klebsiella pneumoniae Introduction to other conditions involved with administration of anticoagulant formulation and bisphosphonate As popularity of dental implantation is increasing, formulation associated with bisphosphonate-related the number of cases associated with complications osteonecrosis of the jaw (BRONJ) which have direct also increase. While there are plenty of researches association with implantability. on locally manifested etiological causes of dental Being the most common systemic disease affecting implant failure, systemic causes have barely been infection of deep neck, diabetes mellitus hinders studied and reported. In clinical settings, there is immunity1) and causes prolonged healingwith poor insufficient evaluation of systemic factors prior to prognosis1). -

Neck Formation and Growth. MAIN TOPOGRAPHIC REGIONS in NECK
Neck formation and growth. MAIN TOPOGRAPHIC REGIONS IN NECK. ANATOMICAL BACKGROUND FOR URGENT LIFE SAVING PERFORMANCES. orofac Ivo Klepáček orofac Vymezení oblasti krku Extent of the neck region Sensitivní oblasti V1, V2, V3., plexus cervicalis orofac * * * * * orofac** * orofac orofac orofaccranial middle caudal orofac orofac Clinical classification of neck lymph nodes orofacClinical classification of neck lymphatic nodes: I - VI Nodi lymphatici out of regiones above: Perifacial, periparotic, retroauricular, suboccipital, retropharyngeal Metastasa v krčních uzlinách Metastasis in cervical orofaclymphonodi TOPOGRAPHIC REGIONS orofacand SPACES Regio colli anterior anterior neck triangle Trigonae : submentale, submandibulare, caroticum (musculare), regio suprasternalis Triangles : submental, submandibular, carotic (muscular), orofacsuprasternal region podkožní sval na povrchové krční fascii r. colli nervi facialis ovládá napětí kůže krku Platysma orofac proc. mastoideus manubrium sterni, clavicula Sternocleidomastoid m. n.accessorius (XI) + branches sternocleidomastoideus from plexus cervicalis orofac Punctum nervosum (Erb ´s point) : there C5 and C6 nerves are connected, + branches from suprascapulari and subclavian nerves orofacWilhelm Heinrich Erb (1840 - 1921), German neurologist orofac orofac mm. suprahyoid suprahyoidei and et mm. infrahyoid orofacinfrahyoidei muscles orofac Thyroid gland and vascular + nerve bundle in neck orofac orofac Žíly veins orofac štítná žláza příštitné orofactělísko a. thyroidea inferior n. laryngeus inferior -

Rare Case of Plunging Ranula with Parapharyngeal Extension and Absent Submandibular Gland: Excision by Transcervical Approach
Central Journal of Ear, Nose and Throat Disorders Bringing Excellence in Open Access Case Report *Corresponding author Abhishek Bhardwaj, Department of Otorhinolaryngology, Safdarjung Hospital Rare Case of Plunging Ranula &Vardhmann Mahavir Medical College, Ansari Nagar, New Delhi-110029, India, Tel: 91-989907792; Email: with Parapharyngeal Extension Submitted: 04 January 2017 Accepted: 29 March 2017 and Absent Submandibular Published: 31 March 2017 ISSN: 2475-9473 Copyright Gland: Excision by Transcervical © 2017 Bhardwaj et al. Approach OPEN ACCESS Keywords Abhishek Bhardwaj*, Sudhagar Eswaran, and Hari Shankar • Ranula Niranjan • Submandibular gland Department of Otorhinolaryngology, Vardhmann Mahavir Medical College and • Pharynx Safdarjung Hospital, India • Skull Base • Neck Abstract Plunging ranula extending into parapharyngeal space till the skull base with associated absence of submandibular gland is a rare finding. Transcervical approach for its excision is a challenging procedure in view of limited exposure and presence of important neurovascular structures in the field. We present a clinical case of a left sided plunging ranula extending into the parapharyngeal space till skull base in a 19 year old male who presented to a tertiary care hospital with complaints of slowly increasing swelling in neck and oral cavity for duration of six months. Ultrasound neck revealed well defined heterogeneously hypoechoic collection in left submandibular region. Contrast enhanced computed tomography revealed a non-enhancing, cystic mass involving left submandibular space extending into left parapharyngeal space till skull base and absent left submandibular gland. Ranula measuring 10cm*6cm was excised in to by tanscervical approach without damage to any neurovascular structure. Histopathology was consistent with low ranula. Patient is in follow up for past six months without any recurrence. -

Complex Odontogenic Infections
Complex Odontogenic Infections Larry ). Peterson CHAPTEROUTLINE FASCIAL SPACE INFECTIONS Maxillary Spaces MANDIBULAR SPACES Secondary Fascial Spaces Cervical Fascial Spaces Management of Fascial Space Infections dontogenic infections are usually mild and easily and causes infection in the adjacent tissue. Whether or treated by antibiotic administration and local sur- not this becomes a vestibular or fascial space abscess is 0 gical treatment. Abscess formation in the bucco- determined primarily by the relationship of the muscle lingual vestibule is managed by simple intraoral incision attachment to the point at which the infection perfo- and drainage (I&D) procedures, occasionally including rates. Most odontogenic infections penetrate the bone dental extraction. (The principles of management of rou- in such a way that they become vestibular abscesses. tine odontogenic infections are discussed in Chapter 15.) On occasion they erode into fascial spaces directly, Some odontogenic infections are very serious and require which causes a fascial space infection (Fig. 16-1). Fascial management by clinicians who have extensive training spaces are fascia-lined areas that can be eroded or dis- and experience. Even after the advent of antibiotics and tended by purulent exudate. These areas are potential improved dental health, serious odontogenic infections spaces that do not exist in healthy people but become still sometimes result in death. These deaths occur when filled during infections. Some contain named neurovas- the infection reaches areas distant from the alveolar cular structures and are known as coinpnrtments; others, process. The purpose of this chapter is to present which are filled with loose areolar connective tissue, are overviews of fascial space infections of the head and neck known as clefts. -

A Guide to Deep Neck Space Fascial Infections for the Dental Team
Main, B. , Collin, J., Coyle, M., Hughes, C., & Thomas, S. (2017). A guide to deep neck space fascial infections for the dental team. Dental Update, 43(8), 745-752. https://doi.org/10.12968/denu.2016.43.8.745 Peer reviewed version Link to published version (if available): 10.12968/denu.2016.43.8.745 Link to publication record in Explore Bristol Research PDF-document This is the accepted author manuscript (AAM). The final published version (version of record) is available online via George Warman Publications at http://www.dental-update.co.uk/articleMatchListArticle.asp?aKey=1577. Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ Oral Surgery A guide to deep neck space fascial infections for the dental team Authors: Mr Barry Main MRCS (Ed), MFDS (Ed), MB ChB (Hons), BDS (Hons), BMSc (Hons) Doctoral Research Fellow and Honorary Specialty Registrar in Oral and Maxillofacial Surgery, School of Oral and Dental Science, University of Bristol, Lower Maudlin Street, Bristol BS1 2LY Mr John Collin BSc, MB ChB, MRCS, BDS Specialty Registrar in Oral and Maxillofacial Surgery, Division of Oral and Maxillofacial Surgery, School of Oral and Dental Science, University of Bristol, Lower Maudline Street, Bristol BS1 2LY Ms Margaret Coyle BA, -

Submandibular Space Infection: a Potentially Lethal Infection
International Journal of Infectious Diseases (2009) 13, 327—333 http://intl.elsevierhealth.com/journals/ijid Submandibular space infection: a potentially lethal infection Paolo Boscolo-Rizzo *, Maria Cristina Da Mosto Department of Medical and Surgical Specialities, Otolaryngology Clinic — Regional Center for Head and Neck Cancer, University of Padua, School of Medicine, Treviso Regional Hospital, Treviso, Italy Received 4 March 2008; received in revised form 19 June 2008; accepted 14 July 2008 Corresponding Editor: William Cameron, Ottawa, Canada KEYWORDS Summary Deep neck infections; Objectives: The aims of this study were to review the clinical characteristics and management of Submandibular infection; submandibular space infections and to identify the predisposing factors of life-threatening Airway control; complications. Treatment; Design and methods: This was a retrospective study at a tertiary academic center. We retrieved Ludwig’s angina; and evaluated the records of all patients admitted to the University of Padua Otolaryngology Clinic Complications at Treviso Regional Hospital with the diagnosis of submandibular space infection for the period 1998—2006. The following variables were reviewed: demographic data, pathogenesis, clinical presentation, associated systemic diseases, bacteriology, imaging studies, medical and surgical treatment, and complications. A multivariate logistic regression analysis was undertaken using a forward stepwise technique. Results: Multivariate analysis identified four risk factors for complications. Anterior visceral space involvement (odds ratio (OR) 54.44; 95% confidence interval (CI) 5.80—511.22) and diabetes mellitus (OR 17.46; 95% CI 2.10—145.29) were the most important predictive factors in the model. Logistic regression analysis also confirmed other comorbidities (OR 11.66; 95% CI 1.35—100.10) and bilateral submandibular swelling (OR 10.67; 95% CI 2.73—41.75) as independent predictors for life- threatening complications. -

Submandibular Space Infection: a Potentially Lethal Infection
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector International Journal of Infectious Diseases (2009) 13, 327—333 http://intl.elsevierhealth.com/journals/ijid Submandibular space infection: a potentially lethal infection Paolo Boscolo-Rizzo *, Maria Cristina Da Mosto Department of Medical and Surgical Specialities, Otolaryngology Clinic — Regional Center for Head and Neck Cancer, University of Padua, School of Medicine, Treviso Regional Hospital, Treviso, Italy Received 4 March 2008; received in revised form 19 June 2008; accepted 14 July 2008 Corresponding Editor: William Cameron, Ottawa, Canada KEYWORDS Summary Deep neck infections; Objectives: The aims of this study were to review the clinical characteristics and management of Submandibular infection; submandibular space infections and to identify the predisposing factors of life-threatening Airway control; complications. Treatment; Design and methods: This was a retrospective study at a tertiary academic center. We retrieved Ludwig’s angina; and evaluated the records of all patients admitted to the University of Padua Otolaryngology Clinic Complications at Treviso Regional Hospital with the diagnosis of submandibular space infection for the period 1998—2006. The following variables were reviewed: demographic data, pathogenesis, clinical presentation, associated systemic diseases, bacteriology, imaging studies, medical and surgical treatment, and complications. A multivariate logistic regression analysis was undertaken using a forward stepwise technique. Results: Multivariate analysis identified four risk factors for complications. Anterior visceral space involvement (odds ratio (OR) 54.44; 95% confidence interval (CI) 5.80—511.22) and diabetes mellitus (OR 17.46; 95% CI 2.10—145.29) were the most important predictive factors in the model. -

SNODENT (Systemized Nomenclature of Dentistry)
ANSI/ADA Standard No. 2000.2 Approved by ANSI: December 3, 2018 American National Standard/ American Dental Association Standard No. 2000.2 (2018 Revision) SNODENT (Systemized Nomenclature of Dentistry) 2018 Copyright © 2018 American Dental Association. All rights reserved. Any form of reproduction is strictly prohibited without prior written permission. ADA Standard No. 2000.2 - 2018 AMERICAN NATIONAL STANDARD/AMERICAN DENTAL ASSOCIATION STANDARD NO. 2000.2 FOR SNODENT (SYSTEMIZED NOMENCLATURE OF DENTISTRY) FOREWORD (This Foreword does not form a part of ANSI/ADA Standard No. 2000.2 for SNODENT (Systemized Nomenclature of Dentistry). The ADA SNODENT Canvass Committee has approved ANSI/ADA Standard No. 2000.2 for SNODENT (Systemized Nomenclature of Dentistry). The Committee has representation from all interests in the United States in the development of a standardized clinical terminology for dentistry. The Committee has adopted the standard, showing professional recognition of its usefulness in dentistry, and has forwarded it to the American National Standards Institute with a recommendation that it be approved as an American National Standard. The American National Standards Institute granted approval of ADA Standard No. 2000.2 as an American National Standard on December 3, 2018. A standard electronic health record (EHR) and interoperable national health information infrastructure require the use of uniform health information standards, including a common clinical language. Data must be collected and maintained in a standardized format, using uniform definitions, in order to link data within an EHR system or share health information among systems. The lack of standards has been a key barrier to electronic connectivity in healthcare. Together, standard clinical terminologies and classifications represent a common medical language, allowing clinical data to be effectively utilized and shared among EHR systems. -

Management of Odontogenic Infections
Management of Odontogenic Infections David B. Ettinger MD,DMD Stages of Infection I. Cellulitis II. Abscess III. Sinus Tract/Fistula CELLULITIS A painful swelling of the soft tissue of the mouth and face resulting from a diffuse spreading of purulent exudate along the fascial planes that separate the muscle bundles. Abscess Well defined borders Pus accumulation in tissues Fluctuant to palpation Cellulitis – “spreading” infection Abscess – “localized” infection FISTULA A drainage pathway or abnormal communication between two epithelium-lined surfaces due to destruction of the intervening tissue. Sinus Tract Abscess ruptures to produce a draining sinus tract Management of Infection Determine the severity of the infection Evaluate the host defense Decide on setting of care Treat surgically Support medically Choose and prescribe antibiotics appropriately Evaluate patient frequently Severity of Infection Rate of progression Potential for airway compromise or affecting vital organs Anatomic location of infection HISTORY Duration of infectious process. Sequence of events and changes in symptoms or signs. Antibiotics prescribed, dosages and responses. Review of systems with emphasis on neuro-ophthalmologic and cardiopulmonary and immune systems. Social history – exposure, travel, (fungal or parasitic infections), chemical dependency. SIGNS OF SEVERITY Fever Dehydration Rapid progression of swelling Trismus Marked pain Quality and/or location of swelling Elevation of tongue Difficulty with speech and swallowing Anatomic -

CPT Code CPT Code Description Standard Fee 0191T INSERT ANT
CPT Code CPT Code Description Standard Fee 0191T INSERT ANT SEGMENT DRAIN INT $ 1,177.00 0184T EXC RECTAL TUMOR ENDOSCOPIC $ 2,669.00 0165T REVISE LUMB ARTIF DISC ADDL $ 1,412.00 0102T EXTRACORP SHOCKWV TX ANESTH $ 1,016.00 0101T EXTRA CORP SHOCKWV TX HI ENERGY $ 1,016.00 99496 TRANSITIONAL CARE MANAGE SERVICE 7 $ 571.00 99495 TRANSITIONAL CARE MANAGE SERVICE 14 $ 431.00 99490 CHRON CARE MANAGEMENT SRVC 20 MIN P $ 115.00 99480 Ic inf pbw 2501‐5000 g subsq $ 420.00 99479 Ic lbw inf 1500‐2500 g subsq $ 438.00 99478 Ic, lbw inf < 1500 gm subsq $ 483.00 99477 INIT DAY HOSP NEONATE CARE $ 1,229.00 99476 Ped crit care age 2‐5, subsq $ 1,228.00 99475 Ped crit care age 2‐5, init $ 1,968.00 99472 Ped critical care, subsq $ 1,423.00 99471 Ped critical care, initial $ 2,797.00 99469 Neonate crit care, subsq $ 1,398.00 99468 Neonate crit care, initial $ 3,230.00 99467 Ped crit care transport addl $ 420.00 99466 Ped crit care transport $ 838.00 99465 Nb resuscitation $ 514.00 99464 Attendance at delivery $ 262.00 99463 Same day nb discharge $ 388.00 99462 Sbsq nb em per day, hosp $ 149.00 99461 Init nb em per day, non‐fac $ 223.00 99460 Init nb em per day, hosp $ 335.00 99407 BEHAV CHNG SMOKING < 10 MIN $ 95.00 99406 BEHAV CHNG SMOKING 3‐10 MIN $ 44.00 99359 PROLONGED SERV, W/O CONTACT, ADD'L $ 194.00 99358 PROLONGED SERV, W/O CONTACT, 1ST HR $ 392.00 99357 PROLONGED SERV, INPATIENT, ADD'L 30 $ 329.00 99356 PROLONGED SERV, INPATIENT, 1ST HR $ 326.00 99355 PROLONGED SERV, OFFICE, ADD'L 30MIN $ 322.00 99354 PROLONGED SERVICE, OFFICE, 1ST HR $ 429.00