Radiological Approach to Deep Neck Space Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Diseases of the Tonsil
DISEASES OF THE TONSIL Dr. Amer salih aljibori Acute Tonsillitis: acute inflammatory condition of the faucial tonsil which may involve the mucosa, crypts,follicles and /or tonsillor parenchyma. Causatve agents; -Viral:Initially starts with viral infection then followed by secondary bacterial infection.Common viruses are influenza,parainfluenza.adenovirus and rhinovirus. -Bacterial:Streptococcus hemolyticus,Hemophilus influenza,pneumococcus,M.catarrahalis. Pathology and pathogenesis: Usually it starts in the childhood when there is low immune status.Depending on the progress of the disease,this can be classified further into the following types. •Catarrhal tonsillitis:It occurs due to viral infection of the upper respiratory tract involving the mucosa of the tonsil •Cryptic tonsillitis: Following viral infection ,secondary bacterial infection supervenes and gets entrapped within the crypts leading to localized form of infection •Acute follicular tonsillitis. It is sever form of tonsillitis caused by virulent organisms like streptococcus hemolyticus and Hemophilus. It causes spread of inflammation from tonsillar crypts to the surrounding tosillar follicles. Acute parenchymal tonsillitis: The secondary bacterial infection will invade to the crypts and it is rapidly spreads into the tonsillar parenchyma.. Cryptic tonsillitis 1- Symptoms -Fever -Generalized malaise and bodyache. -Odynophagia. -Dry cough. -Sorethroat. 2- Signs -Congested and oedematous tonsils -Tonsils may be diffusely swollen in parenchymatous tonsillitis. -Crypts filled with pus in follicular tonsillitis. -Membrane cover the tonsil and termed as membranous tonsillitis. -Tender enlarged jugulodigastric lymph nodes. -Signs of upper respiratory tract infection and adenoiditis. Investigations. -Throat swab for culture and sensitivity. -Blood smear to rule out hemopoeitic disorders like leukemia,agranulocytosis. -Paul-Bunnel test may be required if membrane seen to rulr out infectious mononucleosis. -

A Rare Tumor of Palatine Tonsils: Chondrolipoma
Turkish Archives of Otorhinolaryngology Turk Arch Otorhinolaryngol 2018; 56(3): 180-2 180 Türk Otorinolarengoloji Arşivi A Rare Tumor of Palatine Tonsils: Chondrolipoma Gamze Öztürk1 , Umman Tunç1 , Kadir Balaban2 , Hülya Eyigör1 Case Report 1Department of Otorhinolaryngology, Antalya Training and Research Hospital, Antalya, Turkey 2Department of Pathology, Health Sciences University, Antalya Training and Research Hospital, Antalya, Turkey Abstract Chondrolipomas are benign mesenchymal tumors that 17-year-old male patient, who presented to our clinic have two mature tissues simultaneously and emerge as complaining of dysphagia and was diagnosed with ton- a result of cartilaginous metaplasia in lipomas. They sillar chondrolipoma, is described here, along with the rarely occur in the head and neck area (1%-4%), and radiological, clinical, and immunohistochemical find- occur more frequently in the 60-70 years age group. ings, as well as the review of the literature Although there are cases of the nasopharynx, tongue, lip, and neck reported in the literature, we have been Keywords: Chondrolipoma, palatine tonsil, tonsillar able to find only two cases on tonsils. The case of a neoplasm, dysphagia Introduction magnetic resonance imaging (MRI) of the neck re- Defined by Stout in 1948, chondrolipomas are vealed a well-circumscribed nodular lesion, approx- mesenchymal tumors resulting from cartilaginous imately 1 cm in diameter with a moderate enhance- metaplasia in lipomas and having two mature tissues ment on the anteromedial wall, and fat intensity in simultaneously (1). They may occur anywhere in the all sequences in post contrast series in the right pala- body and generally present as slowly growing, soli- tine tonsil (Figure 2). -
Anatomical Overview
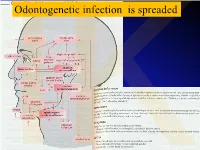
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Vestibule Lingual Frenulum Tongue Hyoid Bone Trachea (A) Soft Palate
Mouth (oral cavity) Parotid gland Tongue Sublingual gland Salivary Submandibular glands gland Esophagus Pharynx Stomach Pancreas (Spleen) Liver Gallbladder Transverse colon Duodenum Descending colon Small Jejunum Ascending colon intestine Ileum Large Cecum intestine Sigmoid colon Rectum Appendix Anus Anal canal © 2018 Pearson Education, Inc. 1 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 2 Upper lip Gingivae Hard palate (gums) Soft palate Uvula Palatine tonsil Oropharynx Tongue (b) © 2018 Pearson Education, Inc. 3 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 4 Visceral peritoneum Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Submucosal glands Mucosa • Surface epithelium • Lamina propria • Muscle layer Submucosa Muscularis externa • Longitudinal muscle layer • Circular muscle layer Serosa (visceral peritoneum) Nerve Gland in Lumen Artery mucosa Mesentery Vein Duct oF gland Lymphoid tissue outside alimentary canal © 2018 Pearson Education, Inc. 5 Diaphragm Falciform ligament Lesser Liver omentum Spleen Pancreas Gallbladder Stomach Duodenum Visceral peritoneum Transverse colon Greater omentum Mesenteries Parietal peritoneum Small intestine Peritoneal cavity Uterus Large intestine Cecum Rectum Anus Urinary bladder (a) (b) © 2018 Pearson Education, Inc. 6 Cardia Fundus Esophagus Muscularis Serosa externa • Longitudinal layer • Circular layer • Oblique layer Body Lesser Rugae curvature of Pylorus mucosa Greater curvature Duodenum Pyloric Pyloric sphincter antrum (a) (valve) © 2018 Pearson Education, Inc. 7 Fundus Body Rugae of mucosa Pyloric Pyloric (b) sphincter antrum © 2018 Pearson Education, Inc. -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Morphological Study of Development and Functional Activity of Palatine
ACTA OTORHINOLARYNGOL ITAL 2003;23:98-101 Morphological study of development and functional activity of palatine tonsils in embryonic age Studio morfologico dello sviluppo e dell’attività funzionale delle tonsille palatine durante l’età embrionale G. NOUSSIOS, J. XANTHOPOULOS, T. ZARABOUKAS, V. VITAL, I. KONSTANTINIDIS Department of Otolaryngology Head and Neck Surgery, Hippokratio General Hospital, Thessaloniki, Greece Key words Parole chiave Palatine tonsils • Histology • Embryology • Lymphocytic Tonsilla palatina • Istologia • Embriologia • Tessuto lin- tissue fatico Summary Riassunto Palatine tonsils play an important role in the development La tonsilla palatina come tutti gli organi a struttura linforetico- of the immune system, being the first organ in the lymph lare esplica una funzione reattiva ed immunitaria nei confronti system which analyses and reacts to antigenic stimulation. dei complessi antigenici batterici e non batterici. In questo stu- In this study, the peritonsillar area of Waldeyer’s ring was dio sono state esaminate, attraverso preparati istologici ed im- investigated in 88 normal human embryos which were munoistochimici, le tonsille palatine di 88 embrioni umani sani examined histologically and immunohistochemically. The (4 embrioni per ogni settimana di sviluppo embrionale, dalla 14a progressive development of palatine tonsils during embry- alla 35a settimana), al fine di valutare lo sviluppo progressivo onic life is discussed. The first appearance of tonsils is in della tonsilla palatina nel corso della vita -

Acinic Cell Carcinoma of the Palatine Tonsil - a Brief Case Report
The Korean Journal of Pathology 2010; 44: 441-3 DOI: 10.4132/KoreanJPathol.2010.44.4.441 Acinic Cell Carcinoma of the Palatine Tonsil - A Brief Case Report - Hun-Soo Kim∙Keum Ha Choi Acinic cell carcinoma (ACC) is a rare, low-grade malignancy of the salivary glands. Most cases occur in the major salivary glands, especially the parotid gland, with only a few cases involving Department of Pathology, Wonkwang the minor salivary gland previously described. A 67-year-old male patient was admitted com- University School of Medicine, Iksan, plaining of an obstructive feeling in the throat. On examination, a lobulated mass in the tonsil- Korea lar surface was noticed. Tonsillectomy was performed under general anesthesia. Histopatho- logical examination of the mass revealed sheets of large, polygonal acinar cells with granu- Received : April 13, 2009 lar, slightly basophilic cytoplasm, which led to the diagnosis of ACC. Here, we present a case Accepted : September 10, 2009 of low-grade ACC of the palatine tonsil, which we believe to be the first reported case of ACC in this location. Corresponding Author Hun-Soo Kim, M.D. Department of Pathology, Wonkwang University School of Medicine, 344-2 Sinyong-dong, Iksan 570-711, Korea Tel: 82-63-859-1813 Fax: 82-63-852-2110 E-mail: [email protected] *This paper was supported by Wonkwang University Key Words : Carcinoma, acinar cell; Palatine tonsil; Salivary glands, minor; Tonsillectomy; in 2008. Secretory vesicles Acinic cell carcinoma (ACC) is a relatively rare, malignant the left palatine tonsil, measuring 2.5 × 1.5 cm in size (Fig.1 epithelial neoplasm in which the tumor cells exhibit acinar inset). -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

TAR and Non-Benefit List: Codes 40000 Thru 49999 Page Updated: January 2021
tar and non cd4 1 TAR and Non-Benefit List: Codes 40000 thru 49999 Page updated: January 2021 Surgery Digestive System Note: Refer to the TAR and Non-Benefit: Introduction to List in this manual for more information about the categories of benefit restrictions. Lips Excision Code Description Benefit Restrictions 40490 Biopsy of lip Assistant Surgeon services not payable Other Procedures Code Description Benefit Restrictions 40799 Unlisted procedure, lips Requires TAR, Primary Surgeon/ Provider Vestibule of Mouth Incision Code Description Benefit Restrictions 40800 Drainage of abscess/cyst, mouth, simple Assistant Surgeon services not payable 40801 Drainage of abscess/cyst, mouth, complicated Assistant Surgeon services not payable 40804 Removal of embedded foreign body, mouth, simple Assistant Surgeon services not payable 40805 Removal of embedded foreign body, mouth, Assistant Surgeon complicated services not payable 40806 Incision labial frenum Non-Benefit Excision Code Description Benefit Restrictions 40808 Biopsy, vestibule of mouth Assistant Surgeon services not payable 40810 Excision of lesion mucosa/submucosa, mouth, without Non-Benefit repair Part 2 – TAR and Non-Benefit List: Codes 40000 thru 49999 tar and non cd4 2 Page updated: January 2021 Excision (continued) Code Description Benefit Restrictions 40812 Excision of lesion mucosa/submucosa, mouth, simple Assistant Surgeon repair services not payable 40816 Excision of lesion, mouth, mucosa/submucosa, Assistant Surgeon complex services not payable 40819 Excision of frenum, labial -

Acute Fascial Space Abscess Upon Dental Implantation to Patients with Diabetes Mellitus
CASE REPORT J Korean Dent Sci. 2015;8(2):89-94 http://dx.doi.org/10.5856/JKDS.2015.8.2.89 ISSN 2005-4742 Acute Fascial Space Abscess upon Dental Implantation to Patients with Diabetes Mellitus Chae Yoon Lee, Baek Soo Lee, Yong Dae Kwon, Joo Young Oh, Jung Woo Lee, Suk Huh, Byeong Joon Choi Department of Oral and Maxillofacial Surgery, School of Dentistry, Kyung Hee University, Seoul, Korea As popularity of dental implantation is increasing, the number of cases associated with complications also increase. Evaluation on diabetes mellitus is often neglected due to the disease's irrelevance to implantability. However, patients with diabetes mellitus are susceptible to infection due to impaired bactericidal ability of neutrophils, cellular immunity and activity of complements. Due to this established connection between diabetes mellitus and infection, a couple of cases were selected to present patients with diabetes mellitus with glycemic incontrollability, suffering from post-implantation dentigerous inter-fascial space abscess. Key Words: Deep neck abscess; Diabetes mellitus; Implant complication; Klebsiella pneumoniae Introduction to other conditions involved with administration of anticoagulant formulation and bisphosphonate As popularity of dental implantation is increasing, formulation associated with bisphosphonate-related the number of cases associated with complications osteonecrosis of the jaw (BRONJ) which have direct also increase. While there are plenty of researches association with implantability. on locally manifested etiological causes of dental Being the most common systemic disease affecting implant failure, systemic causes have barely been infection of deep neck, diabetes mellitus hinders studied and reported. In clinical settings, there is immunity1) and causes prolonged healingwith poor insufficient evaluation of systemic factors prior to prognosis1).