Pediatric Cataract: Challenges and Future Directions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accommodation in the Holmes-Adie Syndrome by G
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.21.4.290 on 1 November 1958. Downloaded from J. Neurol. Neurosurg. Psychiat., 1958, 21, 290. ACCOMMODATION IN THE HOLMES-ADIE SYNDROME BY G. F. M. RUSSELL From the Neurological Research Unit, the National Hospital, Queen Square, London In 1936, Bramwell suggested that the title response to near and far vision respectively. But it "Holmes-Adie syndrome" be given to the clinical has also been noted that the reaction to convergence complex of a slowly reacting pupil and absent tendon may be remarkably wide in its range, considering reflexes in recognition of the descriptions by Holmes that it often follows a stage of complete paralysis (1931) and Adie (1932). Both authors had empha- (Strasburger, 1902). Not only is the reaction to sized the chief clinical features-dilatation of the convergence well preserved when compared to the pupil, apparent loss of the reaction to light, slow reaction to light, but it may in fact be excessive constriction and relaxation in response to near and (Alajouanine and Morax, 1938; Heersema and distant vision, and partial loss of the tendon reflexes. Moersch, 1939). In assessing the degree of tonicity Although the syndrome had been recognized wholly there are, therefore, two criteria: slowness ofguest. Protected by copyright. or in part many years previously (Strasburger, 1902; pupillary movement and preservation of the range Saenger, 1902; Nonne, 1902; Markus, 1906; Weill of movement. and Reys, 1926), credit must go to Adie for stressing Adler and Scheie (1940) showed that the tonic the benign nature of the disorder and distinguishing pupil constricts after the conjunctival instillation it clearly from neurosyphilis. -

Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical on and OFF Poststimulus Responses
1984 • The Journal of Neuroscience, February 22, 2017 • 37(8):1984–1996 Systems/Circuits Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical ON and OFF Poststimulus Responses X Hui Li,1,2 X Xu Liu,1,2 X Ian M. Andolina,1 Xiaohong Li,1 Yiliang Lu,1 Lothar Spillmann,3 and Wei Wang1 1Institute of Neuroscience, State Key Laboratory of Neuroscience, Key Laboratory of Primate Neurobiology, Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Sciences, Shanghai 200031, China, 2University of Chinese Academy of Sciences, Shanghai 200031, China, and 3Department of Neurology, University of Freiburg, 79085 Freiburg, Germany Humans are more sensitive to luminance decrements than increments, as evidenced by lower thresholds and shorter latencies for dark stimuli. This asymmetry is consistent with results of neurophysiological recordings in dorsal lateral geniculate nucleus (dLGN) and primary visual cortex (V1) of cat and monkey. Specifically, V1 population responses demonstrate that darks elicit higher levels of activation than brights, and the latency of OFF responses in dLGN and V1 is shorter than that of ON responses. The removal of a dark or bright disc often generates the perception of a negative afterimage, and here we ask whether there also exist asymmetries for negative afterimages elicited by dark and bright discs. If so, do the poststimulus responses of subcortical ON and OFF cells parallel such afterimage asymmetries? To test these hypotheses, we performed psychophysical experiments in humans and single-cell/S-potential recordings in cat dLGN. Psychophysically, we found that bright afterimages elicited by luminance decrements are stronger and last longer than dark afterimages elicited by luminance increments of equal sizes. -

Cone Contributions to Signals for Accommodation and the Relationship to Refractive Error
Vision Research 46 (2006) 3079–3089 www.elsevier.com/locate/visres Cone contributions to signals for accommodation and the relationship to refractive error Frances J. Rucker ¤, Philip B. Kruger Schnurmacher Institute for Vision Research, State University of New York, State College of Optometry, 33 West 42nd Street, New York, NY 10036, USA Received 18 February 2005; received in revised form 7 April 2006 Abstract The accommodation response is sensitive to the chromatic properties of the stimulus, a sensitivity presumed to be related to making use of the longitudinal chromatic aberration of the eye to decode the sign of the defocus. Thus, the relative sensitivity to the long- (L) and middle-wavelength (M) cones may inXuence accommodation and may also be related to an individual’s refractive error. Accommodation was measured continuously while subjects viewed a sine wave grating (2.2 c/d) that had diVerent cone contrast ratios. Seven conditions tested loci that form a circle with equal vector length (0.27) at 0, 22.5, 45, 67.5, 90, 120, 145 deg. An eighth condition produced an empty Weld stimulus (CIE (x,y) co-ordinates (0.4554, 0.3835)). Each of the gratings moved at 0.2 Hz sinusoidally between 1.00 D and 3.00 D for 40 s, while the eVects of longitudinal chromatic aberration were neutralized with an achromatizing lens. Both the mean level of accommo- dation and the gain of the accommodative response, to sinusoidal movements of the stimulus, depended on the relative L and M cone sen- sitivity: Individuals more sensitive to L-cone stimulation showed a higher level of accommodation (p D 0.01; F D 12.05; ANOVA) and dynamic gain was higher for gratings with relatively more L-cone contrast. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A. -
Pupils and Near Vision
PUPILS AND NEAR VISION Akilesh Gokul PhD Research Fellow Department of Ophthalmology Iris Anatomy Two muscles: • Radially oriented dilator (actually a myo-epithelium) - like the spokes of a wagon wheel • Sphincter/constrictor Pupillary Reflex • Size of pupil determined by balance between parasympathetic and sympathetic input • Parasympathetic constricts the pupil via sphincter muscle • Sympathetic dilates the pupil via dilator muscle • Response to light mediated by parasympathetic; • Increased innervation = pupil constriction • Decreased innervation = pupil dilation Parasympathetic Pathway 1. Three major divisions of neurons: • Afferent division 2. • Interneuron division • Efferent division Near response: • Convergence 3. • Accommodation • Pupillary constriction Pupil Light Parasympathetic – Afferent Pathway 1. • Retinal ganglion cells travel via the optic nerve leaving the optic tracts 2. before the LGB, and synapse in the pre-tectal nucleus. 3. Pupil Light Parasympathetic – Efferent Pathway 1. • Pre-tectal nucleus nerve fibres partially decussate to innervate both Edinger- 2. Westphal (EW) nuclei. • E-W nucleus to ipsilateral ciliary ganglion. Fibres travel via inferior division of III cranial nerve to ciliary ganglion via nerve to inferior oblique muscle. 3. • Ciliary ganglion via short ciliary nerves to innervate sphincter pupillae muscle. Near response: 1. Increased accommodation Pupil 2. Convergence 3. Pupillary constriction Sympathetic pathway • From hypothalamus uncrossed fibres 1. down brainstem to terminate in ciliospinal centre -
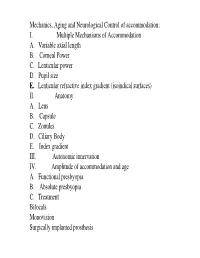
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Restoration of Accommodation: New Perspectives Restauração Da Acomodação: Novas Perspectivas
Editorial Restoration of accommodation: new perspectives Restauração da acomodação: novas perspectivas TRACY SCHROEDER SWARTZ1, KAROLINNE MAIA ROCHA2, MITCH JACKSON3, DAVID HK MA4, DANIEL GOLDBERG5, ANNMARIE HIPSLEY6 Presbyopia is the loss of accommodative ability that occurs with age. Current accommodative theory postu- lates that the lens is primarily responsible for the refractive change that allows us to read. Our understanding of this process has grown substantially with the advent of new technologies, including ultrasound biomicroscopy (UBM), endoscopy, optical coherence tomography (OCT), ray-tracing and wavefront analysis. Goldberg’s Postu- late incorporates all elements of the zonular apparatus into the phenomenon of accommodation(1). The ciliary body contracts during accommodation. Biometry has shown that the lens thickness increases and the anterior chamber depth decreases(2). It has also demonstrated the lens capsule steepens, as the posterior-lens surface moves backwards(2). In addition, there is a decrease in the distance from scleral spur to the ora serrata. UBM identified an attach- ment zone of the posterior zonules adjacent to the ora, and contraction of these zonules is thought to be the etiology of the decrease in distance found with accommodation. This complex action of the zonules is suspec- ted to be reciprocal. As the same time the anterior zonules relax, reducing their tension on the lens such that the lens changes shape anteriorly, the posterior zonules contract, moving the posterior capsule backward. This vitreal-zonular complex stiffens with age, losing its elasticity(1-3). The age-related changes in these structures and their biomechanical interactions with the ciliary-lens complex may contribute to presbyopia(3). -

Forward and Inward Movement of the Ciliary Muscle Apex with Accommodation in Adults
Forward and Inward Movement of the Ciliary Muscle Apex with Accommodation in Adults THESIS Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Trang Pham Prosak Graduate Program in Vision Science The Ohio State University 2014 Master's Examination Committee: Melissa D. Bailey, OD, PhD, Advisor Donald O. Mutti, OD, PhD Marjean Kulp, OD, PhD Copyright by Trang Pham Prosak 2014 Abstract Purpose: to study the inward and forward movement of the ciliary muscle during accommodation and to investigate the effects of one hour of reading on the ciliary muscle behavior in young adults. Methods: Subjects included 23 young adults with a mean age of 23.7 ± 1.9 years. Images of the temporal ciliary muscle of the right eye were obtained using the Visante™ Anterior Segment Ocular Coherence Tomography while accommodative response was monitored simultaneously by the Power-Refractor. Four images were taken at each accommodative response level (0, 4.0 and 6.0 D) before and after one hour of reading. Ciliary muscle thickness was measured at every 0.25 mm posterior to the scleral spur. SSMAX, which is the distance between scleral spur and the thickest point of the muscle (CMTMAX), was also measured. The change in the ciliary muscle thickness and SSMAX with accommodation from 0 to 4.0 D and 0 to 6.0 D was calculated. Paired t-tests were used to determine if the ciliary muscle thickness and SSMAX for the 4.0 and 6.0 diopters of accommodative response were different after one hour of reading. -

Effects of H-7 on the Iris and Ciliary Muscle in Monkeys
LABORATORY SCIENCES Effects of H-7 on the Iris and Ciliary Muscle in Monkeys Baohe Tian, MD; Cameron Millar, PhD; Paul L. Kaufman, MD; Alexander Bershadsky, PhD; Eitan Becker, PhD; Benjamin Geiger, PhD Objectives: To determine the effects of H-7 on (1) iris Results: Topical H-7 prevented anesthesia-induced and ciliary muscles (CMs) in living monkeys; (2) iso- miosis but did not affect resting refraction. Intracam- lated monkey CM strips; (3) actomyosin contractility in eral or intravitreal H-7 dilated the pupil and inhibited cultured Swiss 3T3 cells. miotic but not accommodative responses to pilocar- pine. H-7 inhibited pilocarpine-induced contraction of Methods: (1) Pupillary diameter (calipers) and accom- isolated monkey CM strips and reduced Swiss 3T3 cell modation (refractometer) in living monkeys were mea- contraction. sured after topical, intracameral, or intravitreal admin- istration of H-7 followed by systemic pilocarpine Conclusions: H-7 inhibits actin-based contractility in hydrochloride. (2) Pilocarpine-induced contraction of iso- non-muscle cells and in monkey iris sphincter and CM. lated monkey CM strips following administration of H-7 Under our in vivo experimental conditions, the effect on was measured in a perfusion chamber. (3) Actomyosin the iris predominates over that on the CM. contractility in Swiss 3T3 cells cultured on thin silicone rubber film was determined by measuring cell-induced film wrinkles before and after administration of H-7. Arch Ophthalmol. 1998;116:1070-1077 MOOTH MUSCLE contraction pressure in living -

Resolving the Vergence-Accommodation Conflict
1 Resolving the Vergence-Accommodation Conflict in Head-Mounted Displays A review of problem assessments, potential solutions, and evaluation methods Gregory Kramida Abstract—The vergence-accommodation conflict (VAC) remains a major problem in head-mounted displays for virtual and augmented reality (VR and AR). In this review, I discuss why this problem is pivotal for nearby tasks in VR and AR, present a comprehensive taxonomy of potential solutions, address advantages and shortfalls of each design, and cover various ways to better evaluate the solutions. The review describes how VAC is addressed in monocular, stereoscopic, and multiscopic HMDs, including retinal scanning and accommodation-free displays. Eye-tracking-based approaches that do not provide natural focal cues – gaze-guided blur and dynamic stereoscopy – are also covered. Promising future research directions in this area are identified. Index Terms—Vergence-Accommodation Conflict, Head-Mounted Displays F 1 INTRODUCTION solutions. Finally, Section 6 identifies under-explored areas The vergence-accommodation conflict (henceforth referred within the solution space. to as VAC), sometimes called “accommodation-convergence mismatch”, is a well-known problem in the realm of head- 1.1 The Vergence-Accommodation Conflict or helmet-mounted displays (HMDs), also referred to as head-worn displays (HWDs) [1]: it forces the viewer’s brain The human visual system employs multiple depth stimuli, a to unnaturally adapt to conflicting cues and increases fusion more complete classification of which can be found in a sur- time of binocular imagery, while decreasing fusion accuracy vey by Reichelt et al. [5]. This survey finds that occulomotor [2]. This contributes to (sometimes, severe) visual fatigue cues of consistent vergence and accommodation, which are, (asthenopia), especially during prolonged use [3], [4], [5], in turn, related to retinal cues of blur and disparity, are which, for some people, can even cause serious side-effects critical to comfortable 3D viewing experience. -

The Role of Accommodation in the Control of Binocular Rivalry (BR) Has Been the Basis of BR Control Because Granted Various Degrees of Importance by Es in the Past
Therefore, he concluded that in the The role of accommodation in the case of direct stimulation of the two eyes with rivalry patterns, BR control control of binocular rivalry is effected through accommodation by the blurring of retinal images. However, Fry (1936) has not in fact shown that accommodation changes LEONC. LACK do take place during BR control with Flinders University of South Australia, Bedford Park, South Australia 5042 the eyes in the normal unparalyzed state. He infers that accommodation is The role of accommodation in the control of binocular rivalry (BR) has been the basis of BR control because granted various degrees of importance by Es in the past. The most recent control is lost when his S's eyes are investigation by Fry (1936) concluded that accommodation provides the basis of paralyzed. However, neither BR control through the blurring of retinal images. However, the present study McDougall (1903) nor George (1936) found that the introduction of very small artificial pupils (0.5 mm) did not found BR control to be obliterated by reduce BR control. It was concluded that if accommodation changes are paralyzing the intrinsic eye muscles. occurring with large pupils, the resulting image blurring plays no part in control Indeed, McDougall found hardly any of rivalry. Experiment 2 tested the effect of paralyzed intrinsic eye muscles and effect and warned (1906) against the found almost the same degree of control as in the normal state. The slight overemphasis of peripheral motor decrease of control that was present was attributed to a general performance systems in the control of attention. -

Pediatric Ophthalmology Congress March 22-23, 2018 | London, UK
Koshits Ivan et al., J Clin Exp Ophthalmol 2018, Volume 9 conferenceseries.com DOI: 10.4172/2155-9570-C2-081 3rd Global Pediatric Ophthalmology Congress March 22-23, 2018 | London, UK Koshits Ivan1, Svetlova Olga2 1Petercom-Network / Management Systems Consulting Grope Cl. Corp., 2Department Ophthalmology of North-Western State Medical University named after I.I. Mechnikov, Saint-Petersburg, Russia. Theory: Morpho-physiological characteristics of macula for forming shaped binocular vision 1. Morphology and physiology of the macula. Cones in the Fovea are susceptible to three colors: blue spectrum (440-480 nm), green (510-550 nm) and red (620-770 nm). The foveola (2.2 mm diameter) consists from only red and green cones. Dark blue cones are found inside the rings located around the foveola, with an outside diameter of approximately 4.5 mm (stereo-angle of 180o). The density of blue cones within this ring has the highest concentration [1]. This ring apparently plays a leading role in the physiological mechanism of aiming the eye for the highest accuracy of the image (fig. 1). Fig. 1. Electron Microscopy [1]. Foveola (1) and the ring of blue cones within the macula of the normal eye(А) and in color blind eye (B) [2]. This morphofunctional structure of the macula allows you to reliably "aim" for the area of space even in low-light conditions when the coming light mostly consists from the most powerful violet-blue part of the spectrum. Chart of optical center organization in retina presented in Fig. 2 will help you to better understand the Organization of the incoming optical signal with the functioning of the accommodation system.