The Near Point
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accommodation in the Holmes-Adie Syndrome by G
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.21.4.290 on 1 November 1958. Downloaded from J. Neurol. Neurosurg. Psychiat., 1958, 21, 290. ACCOMMODATION IN THE HOLMES-ADIE SYNDROME BY G. F. M. RUSSELL From the Neurological Research Unit, the National Hospital, Queen Square, London In 1936, Bramwell suggested that the title response to near and far vision respectively. But it "Holmes-Adie syndrome" be given to the clinical has also been noted that the reaction to convergence complex of a slowly reacting pupil and absent tendon may be remarkably wide in its range, considering reflexes in recognition of the descriptions by Holmes that it often follows a stage of complete paralysis (1931) and Adie (1932). Both authors had empha- (Strasburger, 1902). Not only is the reaction to sized the chief clinical features-dilatation of the convergence well preserved when compared to the pupil, apparent loss of the reaction to light, slow reaction to light, but it may in fact be excessive constriction and relaxation in response to near and (Alajouanine and Morax, 1938; Heersema and distant vision, and partial loss of the tendon reflexes. Moersch, 1939). In assessing the degree of tonicity Although the syndrome had been recognized wholly there are, therefore, two criteria: slowness ofguest. Protected by copyright. or in part many years previously (Strasburger, 1902; pupillary movement and preservation of the range Saenger, 1902; Nonne, 1902; Markus, 1906; Weill of movement. and Reys, 1926), credit must go to Adie for stressing Adler and Scheie (1940) showed that the tonic the benign nature of the disorder and distinguishing pupil constricts after the conjunctival instillation it clearly from neurosyphilis. -
A Virtual Try-On System for Prescription Eyeglasses
Feature Article A Virtual Try-On System for Prescription Eyeglasses Qian Zhang and Yu Guo ■ Nanyang Technological University Pierre-Yves Laffont, Tobias Martin, and Markus Gross ■ ETH Zurich ision-correcting eyeglasses have improved We present a system for virtually trying on pre- the lives of millions of people. Eyeglasses scription eyeglasses. Our system acts as a virtual significantly affect the wearer’s appear- mirror, allowing users to try on a variety of eye- Vance, and the selection of new pairs of eyeglasses is glasses with corrective lenses based on their pre- largely based on how the glasses look when wearers scription (see Figure 2). We use an image sequence try them on. However, an often overlooked fact is of the user without eyeglasses as input, along with that corrective lenses introduce distortion caused the user’s eyeglasses prescription and a 3D model by the refraction effect. As Figure 1 illustrates, the of the desired eyeglasses frame. Our system gen- eyes of a person wearing correc- erates a 3D representation of the corrective lenses tive lenses for nearsightedness mounted into the eyeglasses frame and modifies the Corrective lenses introduce appear smaller compared with video sequence to virtually insert the eyeglasses us- distortion caused by the wearing nonprescription lenses, ing image-based rendering. This approach simulates refraction effect, which whereas the eyes of a person the distortion introduced by the prescription lenses changes the wearer’s wearing lenses for farsightedness and gives users a better idea of how they would look appearance. To give users a appear larger. when wearing the new pair of eyeglasses. -
Intraocular Lenses and Spectacle Correction
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -
A Breakthrough in Myopia Control for Your Child
USER GUIDE FOR MiYOSMART MiYOSMART OPTOMETRIC PROTOCOL FOR MiYOSMART MiYOSMART MiYOSMART: A SMART APPROACH TO MYOPIA MiYOSMART The user guide identies what new MiyoSmart wearers should take note of during the adaptation period. To ensure maximized benets of MiyoSmart are experienced, it is recommended to follow the optometric protocol. If you had a way to halt or slow down the progression of myopia, surely you would want to know how. Adaption to new lenses MiyoSmart delivers on this promise and lls a rapidly growing market need. MiyoSmart is an innovative 1ST VISIT 1. It always takes time to get used to your new lenses. The time needed really depends on the individual but wearers can ophthalmic lens for myopia control developed by Hoya Vision Care in cooperation with its research expect about one to two weeks to adapt. collaborator, The Hong Kong Polytechnic University (PolyU). Engineered specically to correct myopic During the rst visit, all visual functions of the child should be assessed to get a clear overview of the current status. A few 2. During the adaptation time, the wearer should avoid: factors are examined to ascertain if the wearer is suitable for MiyoSmart. refractive error and slow down myopia progression, MiyoSmart comes to market at a time when the 1 It is also essential to know the child and his/her parents' ocular and optical history. incidence of myopia is on the rise. Preliminary investigation will also have to be done, where it is compulsory to conduct the following tests and examinations: An estimated 5 billion Research shows that Intensive sport Operating any Using the new lenses Using them on high people, or activities, e.g. -

Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical on and OFF Poststimulus Responses
1984 • The Journal of Neuroscience, February 22, 2017 • 37(8):1984–1996 Systems/Circuits Asymmetries of Dark and Bright Negative Afterimages Are Paralleled by Subcortical ON and OFF Poststimulus Responses X Hui Li,1,2 X Xu Liu,1,2 X Ian M. Andolina,1 Xiaohong Li,1 Yiliang Lu,1 Lothar Spillmann,3 and Wei Wang1 1Institute of Neuroscience, State Key Laboratory of Neuroscience, Key Laboratory of Primate Neurobiology, Center for Excellence in Brain Science and Intelligence Technology, Chinese Academy of Sciences, Shanghai 200031, China, 2University of Chinese Academy of Sciences, Shanghai 200031, China, and 3Department of Neurology, University of Freiburg, 79085 Freiburg, Germany Humans are more sensitive to luminance decrements than increments, as evidenced by lower thresholds and shorter latencies for dark stimuli. This asymmetry is consistent with results of neurophysiological recordings in dorsal lateral geniculate nucleus (dLGN) and primary visual cortex (V1) of cat and monkey. Specifically, V1 population responses demonstrate that darks elicit higher levels of activation than brights, and the latency of OFF responses in dLGN and V1 is shorter than that of ON responses. The removal of a dark or bright disc often generates the perception of a negative afterimage, and here we ask whether there also exist asymmetries for negative afterimages elicited by dark and bright discs. If so, do the poststimulus responses of subcortical ON and OFF cells parallel such afterimage asymmetries? To test these hypotheses, we performed psychophysical experiments in humans and single-cell/S-potential recordings in cat dLGN. Psychophysically, we found that bright afterimages elicited by luminance decrements are stronger and last longer than dark afterimages elicited by luminance increments of equal sizes. -

Cone Contributions to Signals for Accommodation and the Relationship to Refractive Error
Vision Research 46 (2006) 3079–3089 www.elsevier.com/locate/visres Cone contributions to signals for accommodation and the relationship to refractive error Frances J. Rucker ¤, Philip B. Kruger Schnurmacher Institute for Vision Research, State University of New York, State College of Optometry, 33 West 42nd Street, New York, NY 10036, USA Received 18 February 2005; received in revised form 7 April 2006 Abstract The accommodation response is sensitive to the chromatic properties of the stimulus, a sensitivity presumed to be related to making use of the longitudinal chromatic aberration of the eye to decode the sign of the defocus. Thus, the relative sensitivity to the long- (L) and middle-wavelength (M) cones may inXuence accommodation and may also be related to an individual’s refractive error. Accommodation was measured continuously while subjects viewed a sine wave grating (2.2 c/d) that had diVerent cone contrast ratios. Seven conditions tested loci that form a circle with equal vector length (0.27) at 0, 22.5, 45, 67.5, 90, 120, 145 deg. An eighth condition produced an empty Weld stimulus (CIE (x,y) co-ordinates (0.4554, 0.3835)). Each of the gratings moved at 0.2 Hz sinusoidally between 1.00 D and 3.00 D for 40 s, while the eVects of longitudinal chromatic aberration were neutralized with an achromatizing lens. Both the mean level of accommo- dation and the gain of the accommodative response, to sinusoidal movements of the stimulus, depended on the relative L and M cone sen- sitivity: Individuals more sensitive to L-cone stimulation showed a higher level of accommodation (p D 0.01; F D 12.05; ANOVA) and dynamic gain was higher for gratings with relatively more L-cone contrast. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A. -

Types of Contact Lenses and Their Characteristics1
3 ■ Types of Contact Lenses and Their Characteristics1 The basic categories of contact lenses currently acetate butyrate [CAB], PMMA-silicone, and in use are the original hard (polymethylmethacry- silicone). There are variations within each group, late [PMMA]) lenses, soft hydrogels (hydro- but their respective properties are similar enough xymethylmethacrylate [HEMA] and other mate- to consider them as essentially the same type of rials), and gas-permeable hard lenses (cellulose lenses. HARD PMMA LENSES As discussed in the previous chapter, hard rial and safe for use in the eye. It can be molded PMMA lenses were the first lenses introduced or lathed into lenses with a high degree of preci- onto the market, and corneal PMMA lenses simi- sion. Once made, PMMA lenses can be reworked lar to those currently in use have been available and modified to customize them to an individual’s since the early 1950s. Compared to later types of requirements. The result is a safe lens of excellent lenses, PMMA lenses can be difficult to adapt to, visual properties which very closely conforms to and perhaps as many as half of the people fitted patient requirements. PMMA lenses require min- do not become long-term wearers. Since PMMA imal use of cleaning, soaking, and wetting solu- is not water- or gas-permeable, wearers must rely tions. They may be tinted to reduce excessive light on the “tear pump” action of the eye to provide sensitivity, to make them easier to find when oxygen to the covered portion of the cornea. As dropped, or for appearance reasons. They are the wearer blinks, tear interchange occurs from durable, can be renewed by polishing away mi- outside the lens to beneath it, providing the nec- nor surface scratches, and often last 5 to 7 years essary oxygen. -

Lenses and Optics
PHYS 1400: Physical Science for General Education Laboratory Manual LENSES AND OPTICS INTRODUCTION If you (or your cat) wear glasses or contact lenses, you are already familiar with the science of optics. Whether you realize it or not, you understand the idea of a focal point. You are very aware when an image is out of focus (no glasses) or in focus (put your glasses back on). You even know the difference between a real and a virtual image, although you have probably never said to yourself, “I wish that the real image formed by the lens in my eye was better focused on my retina!” Or may be you have. OBJECTIVES ๏ Identify the differences between concave and convex lenses ๏ Use the lens equation to Steampunk Cat is equipped for any ocular emergency. determine the focal length of a convex lens Convex lenses are converging lenses. ๏ Construct ray diagrams to accurately show how an image is formed Concave lenses are diverging lenses. ๏ Demonstrate the difference between a near– and far–sighted eye, and show how each vision problem can be corrected ACTIVITY 1: CONVERGING AND DIVERGING LENSES ๏ Use the converging and diverging lenses to observe objects around the room. ๏ Try to use both as magnifying glasses to enlarge text. ๏ While observing a single object, move the lens toward and away from your eye. Do this for both types of lens. ๏ Try observing objects using various combinations of lenses: two converging, two diverging, one of each. QUESTIONS 1. Which type of lens can you use to magnify text? What happens to the magnified image as you draw the lens farther from the text? 2. -
Pupils and Near Vision
PUPILS AND NEAR VISION Akilesh Gokul PhD Research Fellow Department of Ophthalmology Iris Anatomy Two muscles: • Radially oriented dilator (actually a myo-epithelium) - like the spokes of a wagon wheel • Sphincter/constrictor Pupillary Reflex • Size of pupil determined by balance between parasympathetic and sympathetic input • Parasympathetic constricts the pupil via sphincter muscle • Sympathetic dilates the pupil via dilator muscle • Response to light mediated by parasympathetic; • Increased innervation = pupil constriction • Decreased innervation = pupil dilation Parasympathetic Pathway 1. Three major divisions of neurons: • Afferent division 2. • Interneuron division • Efferent division Near response: • Convergence 3. • Accommodation • Pupillary constriction Pupil Light Parasympathetic – Afferent Pathway 1. • Retinal ganglion cells travel via the optic nerve leaving the optic tracts 2. before the LGB, and synapse in the pre-tectal nucleus. 3. Pupil Light Parasympathetic – Efferent Pathway 1. • Pre-tectal nucleus nerve fibres partially decussate to innervate both Edinger- 2. Westphal (EW) nuclei. • E-W nucleus to ipsilateral ciliary ganglion. Fibres travel via inferior division of III cranial nerve to ciliary ganglion via nerve to inferior oblique muscle. 3. • Ciliary ganglion via short ciliary nerves to innervate sphincter pupillae muscle. Near response: 1. Increased accommodation Pupil 2. Convergence 3. Pupillary constriction Sympathetic pathway • From hypothalamus uncrossed fibres 1. down brainstem to terminate in ciliospinal centre -
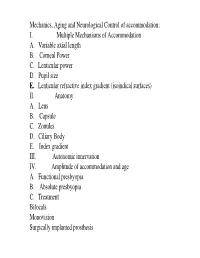
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Primal Contact Lenses Care Instructions and Waiver Page 1 PRIMAL CONTACTS
PRIMAL CONTACTS - Soft (Hydrophilic) Contact Lenses Eye Care Instructions IMPORTANT: Please read carefully and keep this information for future use. Primal Brand Contacts Lenses are available as corrective and non-corrective lens designs. The Lenses are composed of 62% Polymacon and 38% water a silicone-containing hydrogel. PRIMAL (NON-CORRECTIVE) CONTACT LENSES PARAMETERS Diameter : 14,0 mm to 14,8 mm Base Curve : 8,6 mm to 8,8 mm Power : Plano INDICATIONS (USES) AND WEARING RESTRICTIONS Primal ® Brand Fashion Lenses is indicated for non-corrective use in the colour enhancement of the iris and have no therapeutic effects for daily wear. CONTRAINDICATIONS (REASONS NOT TO USE PRIMAL BRAND CONTACT LENSES) Inflammation or infection in or around the eye or eyelids. Any eye disease, injury, or abnormality that affects the cornea, conjunctiva, or eyelids. Any previously diagnosed condition that makes contact lens wear uncomfortable. Any systemic disease that may affect the eye or be exaggerated by wearing contact lenses. Allergic reactions of ocular surfaces of the eye (adnexa) that may be induced or exaggerated by wearing contact lenses or use of contact lens solutions. Allergy to any ingredient, such as mercury or Thimerosal, in a solution which is to be used to care for your contact lenses. Severe dry eye. Any active corneal infection (bacterial, fungal, protozoal or viral). Not to be used if you are unable to follow the lens care regimen or unable to obtain assistance to do so. POTENTIAL ADVERSE SIDE EFFECTS FROM WEARING PRIMAL BRAND CONTACT LENSES Stinging, burning, itching (irritation), pain, tearing or other eye discomfort or sensation of foreign object in the eye.