The Physiology of Female Genital System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter V FOLLICULAR DYNAMICS and REPRODUCTIVE
Chapter V FOLLICULAR DYNAMICS AND REPRODUCTIVE TECHNOLOGIES IN BUFFALO Giuseppina Maria Terzano Istituto Sperimentale per la Zootecnia (Animal Production Research Institute) Via Salaria 31, 00016 Monterotondo (Rome), Italy The general characteristics of reproduction like seasonality, cyclicity and ovulation differ widely in mammals for the following reasons: a) reproductive activity may take place during the whole year or at defined seasons, according to the species and their adaptation to environmental conditions; thus, photoperiod plays a determinant role in seasonal breeders such as rodents, carnivores and ruminants (sheep, goats, buffaloes, deer, etc.,). An extreme situation is observed in foxes with only one ovulation per year, occurring in January or February; b) mammals may be distinguished according to the absence or presence of spontaneous ovulations: in the first group of mammals ( rabbits, hares, cats, mink, camels, Llama), the ovulation is induced by mating and cyclicity is not obvious; in the second group, ovulation occurs spontaneously in each cycle, separating the follicular phase from the luteal phase; c) the length of cycles is quite different among species: small rodents have short cycles of four or five days, farm animals and primates have longer cycles (sheep: 17 days; cow, goat, buffalo, horse and pig: 21 days; primates: 28 days), and dogs are characterized by long cycles of six to seven months, including a two month luteal phase (Concannon, 1993); d) ovulation rates differ widely among species and breeds within a given species: in sheep for example, Merinos d'Arles or Ile-de-France breeds have only one ovulation per cycle, whereas average rates of two to four ovulations per cycle are observed in prolific breeds like Romanov or Finn (Land et al., 1973). -
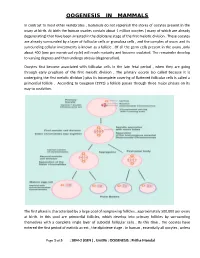
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

Differential Studies of Ovarian Endometriosis Cells from Endometrium Or Oviduct
European Review for Medical and Pharmacological Sciences 2016; 20: 2769-2772 Differential studies of ovarian endometriosis cells from endometrium or oviduct W. LIU1,2, H.-Y. WANG3 1Reproductive Center, the First Affiliated Hospital of Anhui Medical University, Hefei, Anhui, China 2Department of Obstetrics and Gynecology, the Second Affiliated Hospital of Medical University of Anhui, Hefei, Anhui, China 3Department of Gynecologic Oncology, Anhui Provincial Cancer Hospital, the West Branch of Anhui Provincial Hospital, Hefei, Anhui, China Abstract. – OBJECTIVE: To study the promi- In most cases, EMT affects ovary and peritone- nent differences between endometriosis (EMT) um, and as a result a plump shape cyst forms in cells derived from ovary, oviduct and endometri- the ovary. The cyst is called ovarian endometrio- um, and to provided new ideas about the patho- sis cyst (aka ovarian chocolate cyst) which usually genesis of endometriosis. PATIENTS AND METHODS: contains old blood and is covered by endometrioid From June 2010 1 to June 2015, 210 patients diagnosed with en- epithelium. In 1860, Karl von Rokitansky studied dometriosis were enrolled in our study. Patients the disease and observed retrograde menstruation were treated by laparoscopy or conventional in nearly 90% of child-bearing women, and later surgeries in our hospital. Ovarian chocolate proposed “retrograde menstruation implantation cyst and paired normal ovarian tissues, fimbri- theory”. However, this theory explained endo- ated extremity of fallopian and uterine cavity en- metriosis in the abdominopelvic cavity does not domembrane tissues were collected, prepared 2 and observed by microscope. PCR was used for explain endometriosis outside of enterocelia . Lat- 3 4 amplification of target genes (FMO3 and HOXA9) er on, Iwanoff and Meyer proposed “coelomic and Western blot was used to evaluate FMO3 metaplasia theory” which stipulated that endome- and HOXA9 expression levels. -
Gametogenesis: Spermatogenesis & Oogenesis -Structure of Sperm and Egg Fertilization
Gametogenesis: Spermatogenesis & Oogenesis ‐Structure of Sperm and Egg Fertilization ‐ Definition, Mechanism Early development in Frog ‐ Cleavage, Blas tu la, GtlGastrula, DitiDerivatives of Germ layers Vikasana - CET 2012 y Human reproduction y Brief Account of Fertilization: Implantation, Placenta, Role of Gonadotropins and sex hormones , Menstrual cycle. y Fertility Control: Family Planning Methods- y Infertility Control: Meaning, Causes,Treatment y STD: AIDS , Syphilis and Gonorrhea Vikasana - CET 2012 1.Primary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 2.Secondary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 3.Centrioles of sperm control a) Movement of tail b) Hap lo id numb er of ch romosomes c) Help in fertilization d) None of the above. Vikasana - CET 2012 4.The Fertilization membrane is secreted because a) It checks the entry of more sperms after fertilization b) it checks the entry of antigens in ovum c))p it represents the left out tail of the sperm d) it represen tVikasanas the p - l CETasma 2012 mem brane of the sperm 5.Meiosis I occurs in a) Primary spermatocytes b) Secondary spermatocytes c) Both a and b d) Spermatogonia Vikasana - CET 2012 6.Meiosis II occurs in a) Secondary oocyte b))y Primary oocyte c) Spermatogonia d) Oogonia Vikasana - CET 2012 7.Axial filament of sperm is formed by a) Distal centriole b) Prox ima l centitrio le c) Mitochondria d) DNA Vikasana - CET 2012 8.Polar bodies are formed during a) oogenesis -

Anatomy of Male Reproductive System
Reproductive System Anatomy of Male Reproductive System Function: producing offspring Major Organs propagation of the species External Reproductive Organs !in terms of evolution penis and scrotum – the only reason all the other systems exist Internal Organs: only major system that doesn’t work continuously ! only activated at puberty these structures form continuous tube: unlike most other organisms on planet Testes ! mammals only reproduce sexually epididymus humans are dieocious vas deferens ! separate sexed (many animals are monoecious or ejaculatory duct hermaphrodites) urethra in penis th in 7 week of embryonic development genes are activated that trigger differentiation of gonads Accessory organs seminal vesicles prostate gland bulbourethral glands 1. Penis and Scrotum penis is transfer organ glans ! expanded head prepuce ! foreskin both have modified sebaceous glands that produce waxy secretion = smegma Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 1 Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 2 a. seminiferous tubules penis contains erectile tissues that surrounds (700’ of seminiferous tubules in testes) the urethra ! functions in spermatogenesis: ! fill with blood during sexual arousal formation and maturation of sperm cells corpus spongiosum (lower – surrounds urethra) passes along ventral side of penis and in cross section: encloses urethra seminiferous tubules appear roughly circular and contain germinal epithelium 2 coropora cavernosum (upper) (containing germ cells) and sustentacular on dorsal side (Sertoli) cells Sertoli cells protect germ cells and promote all contain numerous tiny blood sinuses their development = lacunae b. interstitial cells scrotum keeps testes at cooler temperature are scattered between the seminiferous tubules ! sperm can only be produced at several degrees below function in hormone secretion normal body temp !testosterone 2. -

The Effectiveness and Safety of the Early Follicular Phase Full-Dose Down
The effectiveness and safety of the early follicular phase full-dose down- regulation protocol for controlled ovarian hyperstimulation: a randomized, paralleled controlled, multicenter trial 2018-12-29 Background Since the first “tube baby”, Louise Brown, was born in the United Kingdom in 1978, many infertile couples have been benefitted from in vitro fertilization and embryo transfer (IVF-ET) and intracytoplasmic sperm injection (ICSI). It is reported that there are over 5 million babies born with the help of assisted reproductive technology (ART). According to the 2015 national data published by Human Fertility and Embryology Authority (HFEA, 48,147 women received 61,726 IVF/ICSI cycles and gave birth to 17,041 newborns [1]. In the United States, 169,602 IVF/ICSI cycles were performed in 2014 and 68,791 tubal babies were born [2]. China has a huge population base, and therefore has a substantial number of infertile couples. Although a late starter, China is developing rapidly in ART and playing a more and more important role in the area of reproductive medicine. In spite of the continuous development in ART, so far, the overall success rate of IVF/ICSI is still hovering around 25-40%. The live birth rate per stimulated cycle is 25.6% in the UK in 2015, fluctuating from 1.9% in women aged 45 and elder to 32.2% in women younger than 35 years old [1]. The IVF/ICSI success rate in 2014 in the US is similar [2]. In China, according to the data submitted by 115 reproductive medicine centers on the ART data reporting system developed by Chinese Society of Reproductive Medicine, the delivery rate is about 40% [3]. -

Luteal Phase Deficiency: What We Now Know
■ OBGMANAGEMENT BY LAWRENCE ENGMAN, MD, and ANTHONY A. LUCIANO, MD Luteal phase deficiency: What we now know Disagreement about the cause, true incidence, and diagnostic criteria of this condition makes evaluation and management difficult. Here, 2 physicians dissect the data and offer an algorithm of assessment and treatment. espite scanty and controversial sup- difficult to definitively diagnose the deficien- porting evidence, evaluation of cy or determine its incidence. Further, while Dpatients with infertility or recurrent reasonable consensus exists that endometrial pregnancy loss for possible luteal phase defi- biopsy is the most reliable diagnostic tool, ciency (LPD) is firmly established in clinical concerns remain about its timing, repetition, practice. In this article, we examine the data and interpretation. and offer our perspective on the role of LPD in assessing and managing couples with A defect of corpus luteum reproductive disorders (FIGURE 1). progesterone output? PD is defined as endometrial histology Many areas of controversy Linconsistent with the chronological date of lthough observational and retrospective the menstrual cycle, based on the woman’s Astudies have reported a higher incidence of LPD in women with infertility and recurrent KEY POINTS 1-4 pregnancy losses than in fertile controls, no ■ Luteal phase deficiency (LPD), defined as prospective study has confirmed these find- endometrial histology inconsistent with the ings. Furthermore, studies have failed to con- chronological date of the menstrual cycle, may be firm the superiority of any particular therapy. caused by deficient progesterone secretion from the corpus luteum or failure of the endometrium Once considered an important cause of to respond appropriately to ovarian steroids. -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -
Variability in the Length of Menstrual Cycles Within and Between Women - a Review of the Evidence Key Points
Variability in the Length of Menstrual Cycles Within and Between Women - A Review of the Evidence Key Points • Mean cycle length ranges from 27.3 to 30.1 days between ages 20 and 40 years, follicular phase length is 13-15 days, and luteal phase length is less variable and averages 13-14 days1-3 • Menstrual cycle lengths vary most widely just after menarche and just before menopause primarily as cycles are anovulatory 1 • Mean length of follicular phase declines with age3,11 while luteal phase remains constant to menopause8 • The variability in menstrual cycle length is attributable to follicular phase length1,11 Introduction Follicular and luteal phase lengths Menstrual cycles are the re-occurring physiological – variability of menstrual cycle changes that happen in women of reproductive age. Menstrual cycles are counted from the first day of attributable to follicular phase menstrual flow and last until the day before the next onset of menses. It is generally assumed that the menstrual cycle lasts for 28 days, and this assumption Key Points is typically applied when dating pregnancy. However, there is variability between and within women with regard to the length of the menstrual cycle throughout • Follicular phase length averages 1,11,12 life. A woman who experiences variations of less than 8 13-15 days days between her longest and shortest cycle is considered normal. Irregular cycles are generally • Luteal phase length averages defined as having 8 to 20 days variation in length of 13-14 days1-3 cycle, whereas over 21 days variation in total cycle length is considered very irregular. -

Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal
Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal intimately part of the endocrine responsibility of the ovary. Introduction If there are no gametes, then hormone production is drastically curtailed. Depletion of oocytes implies depletion of the major Oogenesis is an area that has long been of interest in medicine, hormones of the ovary. In the male this is not the case. as well as biology, economics, sociology, and public policy. Androgen production will proceed normally without a single Almost four centuries ago, the English physician William spermatozoa in the testes. Harvey (1578–1657) wrote ex ovo omnia —“all that is alive This chapter presents basic aspects of human ovarian comes from the egg.” follicle growth, oogenesis, and some of the regulatory mech- During a women’s reproductive life span only 300–400 of anisms involved [ 1 ] , as well as some of the basic structural the nearly 1–2 million oocytes present in her ovaries at birth morphology of the testes and the process of development to are ovulated. The process of oogenesis begins with migra- obtain mature spermatozoa. tory primordial germ cells (PGCs). It results in the produc- tion of meiotically competent oocytes containing the correct genetic material, proteins, mRNA transcripts, and organ- Structure of the Ovary elles that are necessary to create a viable embryo. This is a tightly controlled process involving not only ovarian para- The ovary, which contains the germ cells, is the main repro- crine factors but also signaling from gonadotropins secreted ductive organ in the female. -

Grade 12 Life Science Human Reproduction Notes
KNOWLEDGE AREA: Life Processes in Plants and Animals TOPIC 2.1: Reproduction in Vertebrates Human Reproduction Introduction Structure of Male Reproductive System Structure of Female Reproductive System Main Changes that occur during Puberty Gametogenesis Menstrual Cycle Fertilization and Embryonic Development Implantation and Development Gestation Role of Placenta There are 2 types of reproduction. These are… 1. Sexual and 2. Asexual reproduction We are studying reproduction in humans. Therefore we need to know what is sexual reproduction. Sexual reproduction is reproduction that occurs with the use of gametes. In humans fertilization occurs during sexual reproduction. This means a haploid sperm fuses with a haploid egg to form a diploid zygote. The zygote has 46 chromosomes or 23 pairs of chromosomes therefore it is called diploid. So how many chromosomes does the egg and sperm have? The sperm has 23 chromosomes The egg has 23 chromosomes The zygote then divides by mitosis to produce a large number of identical cells. All the cells have the same number of chromosomes and identical DNA. Some of these cells become differentiated. This means that the cells undergo physical and chemical changes to perform specialized function. Therefore these cells are adapted for their functions. This is how the body parts are formed. Therefore the zygote eventually develops into a fully formed adult. Sexual maturity occur between 11-15. It is known as puberty. During puberty meiosis occurs in the male and female reproductive organs to produce the gametes. Since the gametes are produced by meiosis, each gamete will have a haploid number of chromosomes and each egg or sperm will be genetically different from the other. -

Effects of Caffeine, Alcohol and Smoking on Fertility
Pre-Conception Health Special Interest Group Effects of caffeine, alcohol and smoking on fertility There is an increasing body of evidence that health behaviours affect fertility. As most health behaviours can be modified, providing advice and support in making healthy changes can promote fertility. The evidence relating to the effects on fertility of caffeine, alcohol consumption and smoking is reviewed here. Your Fertility is a national public education campaign funded by the Australian Government Department of Health and Ageing under the Family Planning Grants Program. 1 Updated October 2015 Pre-Conception Health Special Interest Group Effects of caffeine, alcohol and smoking on fertility Evidence review Caffeine Smoking Caffeine is widely consumed as it is present in coffee, tea, some soft drinks There is strong evidence that smoking adversely affects male and female and chocolate. Some evidence suggests that the consumption of caffeine, fertility. Smokers are more likely to be infertile [7, 20-21] and women with a possible dose-response effect, may prolong the time to pregnancy who are exposed to smoking take longer to conceive [22]. Furthermore, and affect the health of a developing foetus, although the mechanism for maternal smoking increases the risk of low birth weight and birth defects this is unclear. Caffeine may affect ovulation and corpus luteum functioning [23] and women who smoke reach menopause earlier than non-smokers through alterations to hormone levels [1] and has been shown to be associated [24]. Smoking can also damage sperm DNA. Heavy smoking (≥20 with elevated early follicular E2 levels in females [2]. Although some studies cigarettes per day) by fathers at the time of conception increases the have found a positive relationship between caffeine consumption and time child’s risk of childhood leukaemia and shortens reproductive lifespan to conception [3-6], study results are inconsistent and should be interpreted of daughters [25-26].