The Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
Reproduction Methods
1336 Chapter 43 | Animal Reproduction and Development fertilization. Seahorses, like the one shown in Figure 43.1, provide an example of the latter. Following a mating dance, the female lays eggs in the male seahorse’s abdominal brood pouch where they are fertilized. The eggs hatch and the offspring develop in the pouch for several weeks. 43.1 | Reproduction Methods By the end of this section, you will be able to do the following: • Describe advantages and disadvantages of asexual and sexual reproduction • Discuss asexual reproduction methods • Discuss sexual reproduction methods Animals produce offspring through asexual and/or sexual reproduction. Both methods have advantages and disadvantages. Asexual reproduction produces offspring that are genetically identical to the parent because the offspring are all clones of the original parent. A single individual can produce offspring asexually and large numbers of offspring can be produced quickly. In a stable or predictable environment, asexual reproduction is an effective means of reproduction because all the offspring will be adapted to that environment. In an unstable or unpredictable environment asexually-reproducing species may be at a disadvantage because all the offspring are genetically identical and may not have the genetic variation to survive in new or different conditions. On the other hand, the rapid rates of asexual reproduction may allow for a speedy response to environmental changes if individuals have mutations. An additional advantage of asexual reproduction is that colonization of new habitats may be easier when an individual does not need to find a mate to reproduce. During sexual reproduction the genetic material of two individuals is combined to produce genetically diverse offspring that differ from their parents. -
Gametogenesis: Spermatogenesis & Oogenesis -Structure of Sperm and Egg Fertilization
Gametogenesis: Spermatogenesis & Oogenesis ‐Structure of Sperm and Egg Fertilization ‐ Definition, Mechanism Early development in Frog ‐ Cleavage, Blas tu la, GtlGastrula, DitiDerivatives of Germ layers Vikasana - CET 2012 y Human reproduction y Brief Account of Fertilization: Implantation, Placenta, Role of Gonadotropins and sex hormones , Menstrual cycle. y Fertility Control: Family Planning Methods- y Infertility Control: Meaning, Causes,Treatment y STD: AIDS , Syphilis and Gonorrhea Vikasana - CET 2012 1.Primary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 2.Secondary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 3.Centrioles of sperm control a) Movement of tail b) Hap lo id numb er of ch romosomes c) Help in fertilization d) None of the above. Vikasana - CET 2012 4.The Fertilization membrane is secreted because a) It checks the entry of more sperms after fertilization b) it checks the entry of antigens in ovum c))p it represents the left out tail of the sperm d) it represen tVikasanas the p - l CETasma 2012 mem brane of the sperm 5.Meiosis I occurs in a) Primary spermatocytes b) Secondary spermatocytes c) Both a and b d) Spermatogonia Vikasana - CET 2012 6.Meiosis II occurs in a) Secondary oocyte b))y Primary oocyte c) Spermatogonia d) Oogonia Vikasana - CET 2012 7.Axial filament of sperm is formed by a) Distal centriole b) Prox ima l centitrio le c) Mitochondria d) DNA Vikasana - CET 2012 8.Polar bodies are formed during a) oogenesis -

Anatomy of Male Reproductive System
Reproductive System Anatomy of Male Reproductive System Function: producing offspring Major Organs propagation of the species External Reproductive Organs !in terms of evolution penis and scrotum – the only reason all the other systems exist Internal Organs: only major system that doesn’t work continuously ! only activated at puberty these structures form continuous tube: unlike most other organisms on planet Testes ! mammals only reproduce sexually epididymus humans are dieocious vas deferens ! separate sexed (many animals are monoecious or ejaculatory duct hermaphrodites) urethra in penis th in 7 week of embryonic development genes are activated that trigger differentiation of gonads Accessory organs seminal vesicles prostate gland bulbourethral glands 1. Penis and Scrotum penis is transfer organ glans ! expanded head prepuce ! foreskin both have modified sebaceous glands that produce waxy secretion = smegma Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 1 Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 2 a. seminiferous tubules penis contains erectile tissues that surrounds (700’ of seminiferous tubules in testes) the urethra ! functions in spermatogenesis: ! fill with blood during sexual arousal formation and maturation of sperm cells corpus spongiosum (lower – surrounds urethra) passes along ventral side of penis and in cross section: encloses urethra seminiferous tubules appear roughly circular and contain germinal epithelium 2 coropora cavernosum (upper) (containing germ cells) and sustentacular on dorsal side (Sertoli) cells Sertoli cells protect germ cells and promote all contain numerous tiny blood sinuses their development = lacunae b. interstitial cells scrotum keeps testes at cooler temperature are scattered between the seminiferous tubules ! sperm can only be produced at several degrees below function in hormone secretion normal body temp !testosterone 2. -

The Reproductive System
27 The Reproductive System PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The reproductive system is designed to perpetuate the species • The male produces gametes called sperm cells • The female produces gametes called ova • The joining of a sperm cell and an ovum is fertilization • Fertilization results in the formation of a zygote © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • Overview of the Male Reproductive System • Testis • Epididymis • Ductus deferens • Ejaculatory duct • Spongy urethra (penile urethra) • Seminal gland • Prostate gland • Bulbo-urethral gland © 2012 Pearson Education, Inc. Figure 27.1 The Male Reproductive System, Part I Pubic symphysis Ureter Urinary bladder Prostatic urethra Seminal gland Membranous urethra Rectum Corpus cavernosum Prostate gland Corpus spongiosum Spongy urethra Ejaculatory duct Ductus deferens Penis Bulbo-urethral gland Epididymis Anus Testis External urethral orifice Scrotum Sigmoid colon (cut) Rectum Internal urethral orifice Rectus abdominis Prostatic urethra Urinary bladder Prostate gland Pubic symphysis Bristle within ejaculatory duct Membranous urethra Penis Spongy urethra Spongy urethra within corpus spongiosum Bulbospongiosus muscle Corpus cavernosum Ductus deferens Epididymis Scrotum Testis © 2012 Pearson Education, Inc. Anatomy of the Male Reproductive System • The Testes • Testes hang inside a pouch called the scrotum, which is on the outside of the body -

Creating an Artificial 3-Dimensional Ovarian Follicle Culture System
micromachines Article Creating an Artificial 3-Dimensional Ovarian Follicle Culture System Using a Microfluidic System Mae W. Healy 1,2, Shelley N. Dolitsky 1, Maria Villancio-Wolter 3, Meera Raghavan 3, Alexandra R. Tillman 3 , Nicole Y. Morgan 3, Alan H. DeCherney 1, Solji Park 1,*,† and Erin F. Wolff 1,4,† 1 Program in Reproductive and Adult Endocrinology, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (M.W.H.); [email protected] (S.N.D.); [email protected] (A.H.D.); [email protected] (E.F.W.) 2 Department of Obstetrics and Gynecology, Walter Reed National Military Medical Center, Bethesda, MD 20889, USA 3 Trans-NIH Shared Resource on Biomedical Engineering and Physical Science, National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, Bethesda, MD 20892, USA; [email protected] (M.V.-W.); [email protected] (M.R.); [email protected] (A.R.T.); [email protected] (N.Y.M.) 4 Pelex, Inc., McLean, VA 22101, USA * Correspondence: [email protected] † Solji Park and Erin F. Wolff are co-senior authors. Abstract: We hypothesized that the creation of a 3-dimensional ovarian follicle, with embedded gran- ulosa and theca cells, would better mimic the environment necessary to support early oocytes, both structurally and hormonally. Using a microfluidic system with controlled flow rates, 3-dimensional Citation: Healy, M.W.; Dolitsky, S.N.; two-layer (core and shell) capsules were created. The core consists of murine granulosa cells in Villancio-Wolter, M.; Raghavan, M.; 0.8 mg/mL collagen + 0.05% alginate, while the shell is composed of murine theca cells suspended Tillman, A.R.; Morgan, N.Y.; in 2% alginate. -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -

Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal
Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal intimately part of the endocrine responsibility of the ovary. Introduction If there are no gametes, then hormone production is drastically curtailed. Depletion of oocytes implies depletion of the major Oogenesis is an area that has long been of interest in medicine, hormones of the ovary. In the male this is not the case. as well as biology, economics, sociology, and public policy. Androgen production will proceed normally without a single Almost four centuries ago, the English physician William spermatozoa in the testes. Harvey (1578–1657) wrote ex ovo omnia —“all that is alive This chapter presents basic aspects of human ovarian comes from the egg.” follicle growth, oogenesis, and some of the regulatory mech- During a women’s reproductive life span only 300–400 of anisms involved [ 1 ] , as well as some of the basic structural the nearly 1–2 million oocytes present in her ovaries at birth morphology of the testes and the process of development to are ovulated. The process of oogenesis begins with migra- obtain mature spermatozoa. tory primordial germ cells (PGCs). It results in the produc- tion of meiotically competent oocytes containing the correct genetic material, proteins, mRNA transcripts, and organ- Structure of the Ovary elles that are necessary to create a viable embryo. This is a tightly controlled process involving not only ovarian para- The ovary, which contains the germ cells, is the main repro- crine factors but also signaling from gonadotropins secreted ductive organ in the female. -

Grade 12 Life Science Human Reproduction Notes
KNOWLEDGE AREA: Life Processes in Plants and Animals TOPIC 2.1: Reproduction in Vertebrates Human Reproduction Introduction Structure of Male Reproductive System Structure of Female Reproductive System Main Changes that occur during Puberty Gametogenesis Menstrual Cycle Fertilization and Embryonic Development Implantation and Development Gestation Role of Placenta There are 2 types of reproduction. These are… 1. Sexual and 2. Asexual reproduction We are studying reproduction in humans. Therefore we need to know what is sexual reproduction. Sexual reproduction is reproduction that occurs with the use of gametes. In humans fertilization occurs during sexual reproduction. This means a haploid sperm fuses with a haploid egg to form a diploid zygote. The zygote has 46 chromosomes or 23 pairs of chromosomes therefore it is called diploid. So how many chromosomes does the egg and sperm have? The sperm has 23 chromosomes The egg has 23 chromosomes The zygote then divides by mitosis to produce a large number of identical cells. All the cells have the same number of chromosomes and identical DNA. Some of these cells become differentiated. This means that the cells undergo physical and chemical changes to perform specialized function. Therefore these cells are adapted for their functions. This is how the body parts are formed. Therefore the zygote eventually develops into a fully formed adult. Sexual maturity occur between 11-15. It is known as puberty. During puberty meiosis occurs in the male and female reproductive organs to produce the gametes. Since the gametes are produced by meiosis, each gamete will have a haploid number of chromosomes and each egg or sperm will be genetically different from the other. -

Diagnostic Evaluation of the Infertile Female: a Committee Opinion
Diagnostic evaluation of the infertile female: a committee opinion Practice Committee of the American Society for Reproductive Medicine American Society for Reproductive Medicine, Birmingham, Alabama Diagnostic evaluation for infertility in women should be conducted in a systematic, expeditious, and cost-effective manner to identify all relevant factors with initial emphasis on the least invasive methods for detection of the most common causes of infertility. The purpose of this committee opinion is to provide a critical review of the current methods and procedures for the evaluation of the infertile female, and it replaces the document of the same name, last published in 2012 (Fertil Steril 2012;98:302–7). (Fertil SterilÒ 2015;103:e44–50. Ó2015 by American Society for Reproductive Medicine.) Key Words: Infertility, oocyte, ovarian reserve, unexplained, conception Use your smartphone to scan this QR code Earn online CME credit related to this document at www.asrm.org/elearn and connect to the discussion forum for Discuss: You can discuss this article with its authors and with other ASRM members at http:// this article now.* fertstertforum.com/asrmpraccom-diagnostic-evaluation-infertile-female/ * Download a free QR code scanner by searching for “QR scanner” in your smartphone’s app store or app marketplace. diagnostic evaluation for infer- of the male partner are described in a Pregnancy history (gravidity, parity, tility is indicated for women separate document (5). Women who pregnancy outcome, and associated A who fail to achieve a successful are planning to attempt pregnancy via complications) pregnancy after 12 months or more of insemination with sperm from a known Previous methods of contraception regular unprotected intercourse (1). -

Oogenesis and Egg Quality in Finfish: Yolk Formation and Other Factors
fishes Review Oogenesis and Egg Quality in Finfish: Yolk Formation and Other Factors Influencing Female Fertility Benjamin J. Reading 1,2,*, Linnea K. Andersen 1, Yong-Woon Ryu 3, Yuji Mushirobira 4, Takashi Todo 4 and Naoshi Hiramatsu 4 1 Department of Applied Ecology, North Carolina State University, Raleigh, NC 27695, USA; [email protected] 2 Pamlico Aquaculture Field Laboratory, North Carolina State University, Aurora, NC 27806, USA 3 National Institute of Fisheries Science, Gijang, Busan 46083, Korea; [email protected] 4 Faculty of Fisheries Sciences, Hokkaido University, Minato, Hakodate, Hokkaido 041-8611, Japan; [email protected] (Y.M.); todo@fish.hokudai.ac.jp (T.T.); naoshi@fish.hokudai.ac.jp (N.H.) * Correspondence: [email protected]; Tel.: +1-919-515-3830 Received: 28 August 2018; Accepted: 16 November 2018; Published: 21 November 2018 Abstract: Egg quality in fishes has been a topic of research in aquaculture and fisheries for decades as it represents an important life history trait and is critical for captive propagation and successful recruitment. A major factor influencing egg quality is proper yolk formation, as most fishes are oviparous and the developing offspring are entirely dependent on stored egg yolk for nutritional sustenance. These maternally derived nutrients consist of proteins, carbohydrates, lipids, vitamins, minerals, and ions that are transported from the liver to the ovary by lipoprotein particles including vitellogenins. The yolk composition may be influenced by broodstock diet, husbandry, and other intrinsic and extrinsic conditions. In addition, a number of other maternal factors that may influence egg quality also are stored in eggs, such as gene transcripts, that direct early embryonic development. -
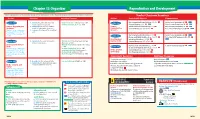
Chapter 38: Reproduction and Development Computer Test Bank Cryopreservation
Chapter 38 Organizer Reproduction and Development Refer to pages 4T-5T of the Teacher Guide for an explanation of the National Science Education Standards correlations. Teacher Classroom Resources Activities/FeaturesObjectivesSection MastersSection TransparenciesReproducible Reinforcement and Study Guide, pp. 167-168 L2 Section Focus Transparency 93 L1 ELL Section 38.1 1. Identify the parts of the male and Inside Story: Sex Cell Production, p. 1033 Section 38.1 female reproductive systems. Problem-Solving Lab 38-1, p. 1035 Concept Mapping, p. 38 L3 ELL Basic Concepts Transparency 74 L2 ELL Human Reproductive 2. Summarize the negative feedback Human Critical Thinking/Problem Solving, p. 38 L3 Basic Concepts Transparency 75 L2 ELL Systems control of reproductive hormones. Reproductive Content Mastery, pp. 185-186, 188 L1 Reteaching Skills Transparency 55 L1P ELL National Science Education 3. Sequence the stages of the menstrual Systems P P cycle. Standards UCP.1-3, UCP.5; P C.1, C.5; F.1 (2 sessions, 11/ P 2 Reinforcement and Study Guide, p. 169 L2 P Section Focus Transparency 94 L1 ELLP blocks) Section 38.2 P LS BioLab and MiniLab Worksheets, pp. 169-170 L2 Reteaching Skills Transparency 56a,P 56b L1 LS P LS Development Laboratory Manual, pp. 277-284 L2 ELL P Before Birth LS Section 38.2 4. Summarize the events during each MiniLab 38-1: Examining Sperm and Egg Content Mastery, pp. 185,LS 187-188 L1 LS P LS trimester of pregnancy. Attraction, p. 1038 LS Development Before MiniLab 38-2: Making a Graph of Fetal Size, P LS P Reinforcement and Study Guide, p.