Physicians on the Front Line the Medical Workforce in Wales in 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessing Internet-Based Information Used to Aid Patient Decision-Making for Pelvic Exenteration for Locally Advanced and Recurrent Rectal Cancer
Assessing Internet-Based Information used to aid patient decision-making for pelvic exenteration for locally advanced and recurrent rectal cancer Anwen Williams ( [email protected] ) Abertawe Bro Morgannwg University Health Board https://orcid.org/0000-0002-8521-9989 Andrew Cunningham Abertawe Bro Morgannwg University Health Board Hayley Hutchings Swansea University Medical School Dean A Harris Abertawe Bro Morgannwg University Health Board Deena Harji Newcastle University Institute for Health and Society Martyn D Evans Abertawe Bro Morgannwg University Health Board Research article Keywords: Internet based information, Google, Patient Decision Aid, Pelvic Exenteration, Rectal Cancer, Locally Advanced Rectal Cancer, Locally Recurrent Rectal Cancer, DISCERN, IPDAS, Quality of Health Literature Posted Date: August 17th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-59146/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/15 Abstract Background: To establish what online decision aids are currently available for patients contemplating pelvic exenteration (PE) for locally advanced and recurrent rectal cancer (LARC and LRRC). Methodology: A grey literature review was carried out using the Google SearchTM engine undertaken using a predened search strategy (PROSPERO database CRD42019122933). Written health information was assessed using the DISCERN criteria and International Patient Decision Aids Standards (IPDAS) with readability content assessed using the Flesch-Kincaid score. Results: Google search yielded 27,782,200 results for the predened search criteria. 131 sources were screened resulting in the analysis of 6 sources. No sources were identied as a decision aid according to the IPDAS criteria. All sources were deemed acceptable quality of written health information, scoring a global score of 3. -

Legal & Policy Briefing
LEGAL & POLICY BRIEFING Access to Healthcare for Migrants in Wales AUTHOR: JONATHAN PRICE PUBLISHED: February 2016 http://www.wrc.wales/migration-information LEGAL & POLICY BRIEFING: Access to Healthcare for Migrants in Wales TABLE OF CONTENTS Introduction .............................................................................................3 How this briefing is structured ..................................................................3 The NHS in Wales .....................................................................................3 Primary care .............................................................................................3 Secondary care .........................................................................................4 Immigration Health Surcharge ..................................................................8 Further resources ................................................................................... 10 Acknowledgments .................................................................................. 10 HTTP://WWW.WRC.WALES/MIGRATION-INFORMATION PAGE 2 LEGAL & POLICY BRIEFING: Access to Healthcare for Migrants in Wales Introduction This briefing provides a general overview of migrants’ entitlement to NHS healthcare services in Wales. A broad range of migrant groups are considered here, including mobile EU citizens, asylum seekers, refugees and third country nationals, including those with irregular immigration status. Information on access to both primary and secondary healthcare services -
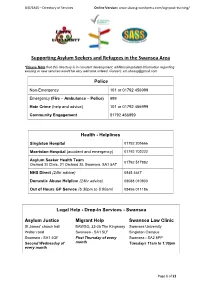
Supporting Asylum Seekers and Refugees in the Swansea Area
UiD/SASS – Directory of Services Online Version: www.sbassg.wordpress.com/signpost-training/ Supporting Asylum Seekers and Refugees in the Swansea Area *Please Note that this directory is in constant development, additional/updated information regarding existing or new services would be very welcome indeed. Contact: [email protected] Police Non-Emergency 101 or 01792 456999 Emergency (Fire – Ambulance – Police) 999 Hate Crime (help and advice) 101 or 01792 456999 Community Engagement 01792 456999 Health - Helplines Singleton Hospital 01792 205666 Morriston Hospital (accident and emergency) 01792 702222 Asylum Seeker Health Team 01792 517882 Orchard St Clinic, 21 Orchard St, Swansea. SA1 5AT NHS Direct (24hr advice) 0845 4647 Domestic Abuse Helpline (24hr advice) 08088 010800 Out of Hours GP Service (6:30pm to 8:00am) 08456 011186 Legal Help - Drop-In Services - Swansea Asylum Justice Migrant Help Swansea Law Clinic St James’ church hall BAWSO, 33-35 The Kingsway Swansea University Walter road Swansea - SA1 5LF Singleton Campus Swansea - SA1 4QF First Thursday of every Swansea - SA2 8PP Second Wednesday of month Tuesdays 11am to 1:30pm every month Page 1 of 21 UiD/SASS – Directory of Services Online Version: www.sbassg.wordpress.com/signpost-training/ Food Banks in Swansea Venue Address Day Time 646 Mumbles Rd. Mumbles - SA3 Red Cafe Monday 1pm to 3pm 4EA Ty Croeso 97 High Street. Clydach - SA6 5LN Tuesday 10am to 12pm St Stephen’s Gelli Street. Port Tennant - SA1 8NF Tuesday 2:30pm to 4pm Church City Church Dyfatty Street. City Centre - SA1 1QQ Wednesday 10am to 12pm Gorseinon Lime Street. Gorseinon - SA4 4EE Thursday 10am to 12pm Institute Lifepoint Fynone Road. -

Candidate Information Pack
Candidate Information Contents Section 1 – Welcome and Foreword 3 Section 2 – The NHS in Wales 5 Section 3 – Purpose, vision, aims and values 7 Section 4 – How we are structured and overview of services 9 Section 5 – Strategic change, challenges and planning 14 Section 6 – Working in partnership with Universities 18 Section 7 – A very special and unique place to live and work 25 Chairman’s Foreword Dear Candidate ABMU Health Board is ambitious - we aim to create a new model of a 21st century health economy, based on our core values of Caring for Each Other, Working Together and Always Improving. We want an Executive Director who shares our values and has ambition, drive and determination to help us create that. In Wales, NHS policy is the responsibility of the Welsh Government and health policy has diverged significantly from that operating in England where a market-driven system, increasingly based on competition, has developed. In Wales the emphasis is on collaboration not competition. Unlike in England, the seven Health Boards in Wales Andrew Davies, Chairman deliver an integrated service and are responsible for both commissioning and planning all levels of citizen-centred healthcare services, as well as delivering them. In practice, this means that ABMU Health Board is delivering - and developing - services which range from primary and community health care, mental health, and responsibility for public health, through to highly specialised tertiary services. We are doing this in close partnership with our local authority, third sector -

Our Health, Our Health Service Green Paper
Number: WG25325 Welsh Government Green Paper Our Health, Our Health Service Date of issue: 6 July 2015 Action required: Responses by 20 November 2015 Digital ISBN 978 1 4734 3673 2 © Crown Copyright 2015 Overview Data protection This consultation is to promote discussion and How the views and information you give gather views to help inform the potential for us will be used future legislation in the Fifth Assembly with Any response you send us will be seen in full regards to improving quality and governance by Welsh Government staff dealing with the in the NHS in Wales. issues which this consultation is about. It may also be seen by other Welsh Government staff How to respond to help them plan future consultations. Please respond by answering the questions at The Welsh Government intends to publish a the back of this document and sending it to: summary of the responses to this document. We may also publish responses in full. [email protected] Normally, the name and address (or part of Or by post to: the address) of the person or organisation who sent the response are published with Matthew Tester the response. This helps to show that the Healthcare Quality Division consultation was carried out properly. If you Department of Health and Social Services do not want your name or address published, Welsh Government please tell us this in writing when you send Cathays Park your response. We will then blank them out. Cardiff CF10 3NQ Names or addresses we blank out might still get published later, though we do not think this would happen very often. -
Pocketbook for You, in Any Print Style: Including Updated and Filtered Data, However You Want It
Hello Since 1994, Media UK - www.mediauk.com - has contained a full media directory. We now contain media news from over 50 sources, RAJAR and playlist information, the industry's widest selection of radio jobs, and much more - and it's all free. From our directory, we're proud to be able to produce a new edition of the Radio Pocket Book. We've based this on the Radio Authority version that was available when we launched 17 years ago. We hope you find it useful. Enjoy this return of an old favourite: and set mediauk.com on your browser favourites list. James Cridland Managing Director Media UK First published in Great Britain in September 2011 Copyright © 1994-2011 Not At All Bad Ltd. All Rights Reserved. mediauk.com/terms This edition produced October 18, 2011 Set in Book Antiqua Printed on dead trees Published by Not At All Bad Ltd (t/a Media UK) Registered in England, No 6312072 Registered Office (not for correspondence): 96a Curtain Road, London EC2A 3AA 020 7100 1811 [email protected] @mediauk www.mediauk.com Foreword In 1975, when I was 13, I wrote to the IBA to ask for a copy of their latest publication grandly titled Transmitting stations: a Pocket Guide. The year before I had listened with excitement to the launch of our local commercial station, Liverpool's Radio City, and wanted to find out what other stations I might be able to pick up. In those days the Guide covered TV as well as radio, which could only manage to fill two pages – but then there were only 19 “ILR” stations. -

Bundle Public Board 29 March 2018
Bundle Public Board 29 March 2018 2.6 Report of the Chief Executive / Adroddiad y Prif Weithredwr Presenter: Steve Moore Report of the Chief Executive March 2018 App A - Register of Sealings March 2018 Board App B - Consultation Report March 2018 App C - Zero Based Review of HDdUHB 2.6 Report of the Chief Executive / Adroddiad y Prif Weithredwr 1 Report of the Chief Executive March 2018 CYFARFOD BWRDD PRIFYSGOL IECHYD UNIVERSITY HEALTH BOARD MEETING DYDDIAD Y CYFARFOD: 29 March 2018 DATE OF MEETING: TEITL YR ADRODDIAD: Chief Executive’s Report TITLE OF REPORT: CYFARWYDDWR ARWEINIOL: Steve Moore, Chief Executive LEAD DIRECTOR: SWYDDOG ADRODD: Sian-Marie James, Head of Corporate Office REPORTING OFFICER: Pwrpas yr Adroddiad (dewiswch fel yn addas) Purpose of the Report (select as appropriate) Ar Gyfer Penderfyniad/For Decision ADRODDIAD SCAA SBAR REPORT Sefyllfa / Situation The purpose of this Report is to: • Update the Board on relevant matters undertaken as Chief Executive of Hywel Dda University Health Board (the UHB) since the previous Board meeting held on 25 January 2018; and • Provide an overview of the current key issues, both at a local and national level, within NHS Wales. Cefndir / Background This Report provides the opportunity to present items to the Board to demonstrate areas of work that are being progressed and achievements that are being made, which may not be subject to prior consideration by a Committee of the Board, or may not be directly reported to the Board through Board reports. Asesiad / Assessment 1. Register of Sealings The UHB’s Common Seal has been applied to legal documents and a record of the sealing of these documents has been entered into the Register kept for this purpose. -

Swansea Via Singleton Hospital Service 43 (NAAO043)
Morriston Hospital - Swansea via Singleton Hospital Service 43 (NAAO043) Monday to Friday (Excluding Bank Holidays) (Inbound) Timetable valid from 12th April 2021 until further notice Days: SH SD Operator: NADT NADT NADT NADT NADT NADT NADT NADT NADT Morriston Hospital 0720 0720 0827 1027 1157 1327 1457 1627 1837 Llangyfelach (Clasemont Road) 0725 0725 0833 1033 1203 1333 1503 1633 1843 Clase (DVLA) 0728 0728 0836 1036 1206 1336 1506 1636 1846 Penlan Roundabout 0741 0741 0846 1046 1216 1346 1516 1646 1856 Blaen-y-Maes Roundabout 0747 0747 0852 1052 1222 1352 1522 1652 1902 Caereithen Cross 0758 0758 0856 1056 1226 1356 1526 1656 1906 Fforestfach Cross 0809 0809 0858 1058 1228 1358 1528 1658 1908 Gwynedd Avenue 0816 0816 0903 1103 1233 1403 1533 1703 1913 Mayhill Post Office 0821 0821 0908 1108 1238 1408 1538 1708 1918 Townhill (Graiglwyd Square) 0827 0827 0912 1112 1242 1412 1542 1712 1922 Gower College (Vivian Road) 0831 0831 0916 1116 1246 1416 1546 1716 1926 Sketty Cross (Dilwyn Road) 0835 0835 0919 1119 1249 1419 1549 1719 1929 Sketty Park (Hen Dderwen) | | 0924 1124 1254 | | | | Sketty Park (New Mill Road) | | 0926 1126 1256 | | | | Derwen Fawr (Saunders Way) | | 0929 1129 1259 | | | | Singleton Hospital 0840 0840 0934 1134 1304 1424 1554 1724 1934 University (Main Hall) 0841 0841 0937 1137 1307 1427 1557 1727 1937 University (Mumbles Road) 0843 0843 0938 1138 1308 1428 1558 1728 1938 Brynmill (Roundabout) 0845 0845 0941 1141 1311 1431 1601 1731 1941 Guildhall (Crown Court) 0848 0848 0944 1144 1314 1434 1604 1734 1944 Swansea City -

Glossary of Health and Care Terms
Glossary of health and care terms May 2021 This glossary provides a summary of organisations and general terms used within the health and care sector in Wales. The glossary provides some of the most common words and phrases used. 0 - 9 Acute Medical Unit (AMU) 111 An AMU is the first point of entry for patients referred to hospital as The NHS Wales 111 service is a free- emergencies by their GP and those to-call, non-emergency medical requiring admission from the helpline, available 24 hours a day, to Emergency Department. be used for health information, advice and access to urgent care. The service is currently operational in the Aneurin Add to Your Life Bevan University Health Board (UHB), Cwm Taf Morgannwg UHB, Hywel Dda ‘Add to Your Life’ is an online health- UHB, Powys Teaching Health Board check, which provides assessment (THB) and Swansea Bay UHB areas. It and community-based support to is anticipated that 111 will be rolled out enable over 50s in Wales to assess across Wales by the end of 2021. and improve their own health. A Additional Learning Needs and Education Tribunal Act 2018 A Regional Collaboration for Health (ALNET) (ARCH) The ALNET Act 2018 establishes a ARCH is a regional partnership made statutory framework for supporting up of Swansea University, Swansea children and young people with Bay UHB and Hywel Dda UHB. The additional learning needs (ALN) from ARCH partners work to improve the birth; whilst they are in school; and, if health, wealth and wellbeing of the they are over compulsory school age, people of South West Wales. -
Summary Report for the Team
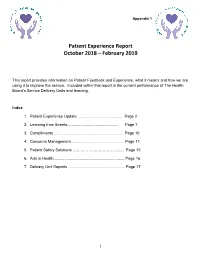
Appendix 1 Patient Experience Report October 2018 – February 2019 This report provides information on Patient Feedback and Experience, what it means and how we are using it to improve the service. Included within this report is the current performance of The Health Board’s Service Delivery Units and learning. Index 1. Patient Experience Update ........................................ Page 2 2. Learning from Events............................................... Page 7 3. Compliments ................................................................ Page 10 4. Concerns Management................................................. Page 11 5. Patient Safety Solutions ………………………………… Page 15 6. Arts in Health................................................................. Page 16 7. Delivery Unit Reports .................................................... Page 17 __________________________________________________________________________________________ 1 1. PATIENT EXPERIENCE 1.1 Inpatient Discharge Feedback Rates The Patient Experience Team continues to provide support and guidance to the Service Delivery Units (“SDU”) on increasing the number of surveys completed. The graph below indicates the discharge feedback rate benchmarked against the best performing Trusts for patient feedback returns in NHS England (35%). The Health Board’s aim is to increase the rate to 35%. October 2018 was 22.85%, November 2018 was 24.09%, December 2018 was 17.99%, January 2019 was 17.16% and February 2019 was 21.16%. __________________________________________________________________________________________ -

Audit Committee Ambulance Services in Wales Inquiry July 2009
Audit Committee Ambulance Services in Wales Inquiry July 2009 The National Assembly for Wales is the democratically elected body that represents the interests of Wales and its people, makes laws for Wales and holds the Welsh Government to account. An electronic copy of this report can be found on the National Assembly’s website www.assemblywales.org Further hard copies of this document can be obtained from: Audit Committee National Assembly for Wales Cardiff Bay CF99 1NA Tel: 029 2089 8617 Fax: 029 2089 8021 Email: [email protected] National Assembly for Wales Audit Committee Ambulance Services in Wales Inquiry July 2009 Ambulance Services in Wales Inquiry Contents Chair’s Foreword 4 Introduction 5 The eight minute standard 8 Rapid Response Vehicles 9 Transport of patients by other emergency services 11 Intelligent targets 12 Advanced Paramedic Practitioners 13 Handovers 15 Data terminals 16 Handover targets 17 Making best use of resources 18 Ambulance officers 19 Restocking 21 Sharing best practice 21 Addressing geographical variations 22 Staffing levels at emergency departments 23 The staff experience 24 WAST financial position 25 Re-organisation of the NHS 26 1 Annexes Audit Committee Record of Proceedings 21 January Annex 1 2009 Audit Committee Record of Proceedings 11 March Annex 2 2009 Audit Committee Record of Proceedings 30 April 2009 Annex 3 Audit Committee Record of Proceedings 4 June 2009 Annex 4 Audit Committee Record of Proceedings 18 June Annex 5 2009 AC(3) 08-09 (p1) Unison – Ambulance Services in Annex 6 Wales -

Review of Evidence of Inequalities in Access to Healthcare Services for Disabled People in Wales
Ymchwil gymdeithasol Social research Rhif/Number: 55/2015 Review of Evidence of Inequalities in Access to Healthcare Services for Disabled People in Wales Review of Evidence of Inequalities in Access to Healthcare Services for Disabled People in Wales Shaun Smith ESRC PhD Internship Scheme This research was produced as part of a four month-long PhD Internship with the Welsh Government, funded jointly by the Welsh Government and the Economic and Social Research Council (ESRC). The ESRC was not involved in the study’s design, collection of data, analysis or writing of the report. Views expressed in this report are those of the researcher and not necessarily those of the Welsh Government. For further information please contact: Joanne Coates Social Research and Information Division Knowledge and Analytical Services Welsh Government Cathays Park Cardiff, CF10 3NQ Tel/Ffôn: 02920 825540 Email/Ebost: [email protected] Welsh Government Social Research, 15 October 2015 ISBN: 978-1-4734-4870-4 © Crown Copyright 2015 All content is available under the Open Government Licence v3.0 , except where otherwise stated. http://www.nationalarchives.gov.uk/doc/open-government-licence/version/3/ Contents Acronyms ................................................................................................................... 5 Executive Summary ................................................................................................... 6 Introduction.......................................................................................................................