Assessing Internet-Based Information Used to Aid Patient Decision-Making for Pelvic Exenteration for Locally Advanced and Recurrent Rectal Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
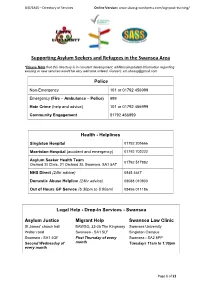
Supporting Asylum Seekers and Refugees in the Swansea Area
UiD/SASS – Directory of Services Online Version: www.sbassg.wordpress.com/signpost-training/ Supporting Asylum Seekers and Refugees in the Swansea Area *Please Note that this directory is in constant development, additional/updated information regarding existing or new services would be very welcome indeed. Contact: [email protected] Police Non-Emergency 101 or 01792 456999 Emergency (Fire – Ambulance – Police) 999 Hate Crime (help and advice) 101 or 01792 456999 Community Engagement 01792 456999 Health - Helplines Singleton Hospital 01792 205666 Morriston Hospital (accident and emergency) 01792 702222 Asylum Seeker Health Team 01792 517882 Orchard St Clinic, 21 Orchard St, Swansea. SA1 5AT NHS Direct (24hr advice) 0845 4647 Domestic Abuse Helpline (24hr advice) 08088 010800 Out of Hours GP Service (6:30pm to 8:00am) 08456 011186 Legal Help - Drop-In Services - Swansea Asylum Justice Migrant Help Swansea Law Clinic St James’ church hall BAWSO, 33-35 The Kingsway Swansea University Walter road Swansea - SA1 5LF Singleton Campus Swansea - SA1 4QF First Thursday of every Swansea - SA2 8PP Second Wednesday of month Tuesdays 11am to 1:30pm every month Page 1 of 21 UiD/SASS – Directory of Services Online Version: www.sbassg.wordpress.com/signpost-training/ Food Banks in Swansea Venue Address Day Time 646 Mumbles Rd. Mumbles - SA3 Red Cafe Monday 1pm to 3pm 4EA Ty Croeso 97 High Street. Clydach - SA6 5LN Tuesday 10am to 12pm St Stephen’s Gelli Street. Port Tennant - SA1 8NF Tuesday 2:30pm to 4pm Church City Church Dyfatty Street. City Centre - SA1 1QQ Wednesday 10am to 12pm Gorseinon Lime Street. Gorseinon - SA4 4EE Thursday 10am to 12pm Institute Lifepoint Fynone Road. -

Candidate Information Pack
Candidate Information Contents Section 1 – Welcome and Foreword 3 Section 2 – The NHS in Wales 5 Section 3 – Purpose, vision, aims and values 7 Section 4 – How we are structured and overview of services 9 Section 5 – Strategic change, challenges and planning 14 Section 6 – Working in partnership with Universities 18 Section 7 – A very special and unique place to live and work 25 Chairman’s Foreword Dear Candidate ABMU Health Board is ambitious - we aim to create a new model of a 21st century health economy, based on our core values of Caring for Each Other, Working Together and Always Improving. We want an Executive Director who shares our values and has ambition, drive and determination to help us create that. In Wales, NHS policy is the responsibility of the Welsh Government and health policy has diverged significantly from that operating in England where a market-driven system, increasingly based on competition, has developed. In Wales the emphasis is on collaboration not competition. Unlike in England, the seven Health Boards in Wales Andrew Davies, Chairman deliver an integrated service and are responsible for both commissioning and planning all levels of citizen-centred healthcare services, as well as delivering them. In practice, this means that ABMU Health Board is delivering - and developing - services which range from primary and community health care, mental health, and responsibility for public health, through to highly specialised tertiary services. We are doing this in close partnership with our local authority, third sector -
Pocketbook for You, in Any Print Style: Including Updated and Filtered Data, However You Want It
Hello Since 1994, Media UK - www.mediauk.com - has contained a full media directory. We now contain media news from over 50 sources, RAJAR and playlist information, the industry's widest selection of radio jobs, and much more - and it's all free. From our directory, we're proud to be able to produce a new edition of the Radio Pocket Book. We've based this on the Radio Authority version that was available when we launched 17 years ago. We hope you find it useful. Enjoy this return of an old favourite: and set mediauk.com on your browser favourites list. James Cridland Managing Director Media UK First published in Great Britain in September 2011 Copyright © 1994-2011 Not At All Bad Ltd. All Rights Reserved. mediauk.com/terms This edition produced October 18, 2011 Set in Book Antiqua Printed on dead trees Published by Not At All Bad Ltd (t/a Media UK) Registered in England, No 6312072 Registered Office (not for correspondence): 96a Curtain Road, London EC2A 3AA 020 7100 1811 [email protected] @mediauk www.mediauk.com Foreword In 1975, when I was 13, I wrote to the IBA to ask for a copy of their latest publication grandly titled Transmitting stations: a Pocket Guide. The year before I had listened with excitement to the launch of our local commercial station, Liverpool's Radio City, and wanted to find out what other stations I might be able to pick up. In those days the Guide covered TV as well as radio, which could only manage to fill two pages – but then there were only 19 “ILR” stations. -

Swansea Via Singleton Hospital Service 43 (NAAO043)
Morriston Hospital - Swansea via Singleton Hospital Service 43 (NAAO043) Monday to Friday (Excluding Bank Holidays) (Inbound) Timetable valid from 12th April 2021 until further notice Days: SH SD Operator: NADT NADT NADT NADT NADT NADT NADT NADT NADT Morriston Hospital 0720 0720 0827 1027 1157 1327 1457 1627 1837 Llangyfelach (Clasemont Road) 0725 0725 0833 1033 1203 1333 1503 1633 1843 Clase (DVLA) 0728 0728 0836 1036 1206 1336 1506 1636 1846 Penlan Roundabout 0741 0741 0846 1046 1216 1346 1516 1646 1856 Blaen-y-Maes Roundabout 0747 0747 0852 1052 1222 1352 1522 1652 1902 Caereithen Cross 0758 0758 0856 1056 1226 1356 1526 1656 1906 Fforestfach Cross 0809 0809 0858 1058 1228 1358 1528 1658 1908 Gwynedd Avenue 0816 0816 0903 1103 1233 1403 1533 1703 1913 Mayhill Post Office 0821 0821 0908 1108 1238 1408 1538 1708 1918 Townhill (Graiglwyd Square) 0827 0827 0912 1112 1242 1412 1542 1712 1922 Gower College (Vivian Road) 0831 0831 0916 1116 1246 1416 1546 1716 1926 Sketty Cross (Dilwyn Road) 0835 0835 0919 1119 1249 1419 1549 1719 1929 Sketty Park (Hen Dderwen) | | 0924 1124 1254 | | | | Sketty Park (New Mill Road) | | 0926 1126 1256 | | | | Derwen Fawr (Saunders Way) | | 0929 1129 1259 | | | | Singleton Hospital 0840 0840 0934 1134 1304 1424 1554 1724 1934 University (Main Hall) 0841 0841 0937 1137 1307 1427 1557 1727 1937 University (Mumbles Road) 0843 0843 0938 1138 1308 1428 1558 1728 1938 Brynmill (Roundabout) 0845 0845 0941 1141 1311 1431 1601 1731 1941 Guildhall (Crown Court) 0848 0848 0944 1144 1314 1434 1604 1734 1944 Swansea City -
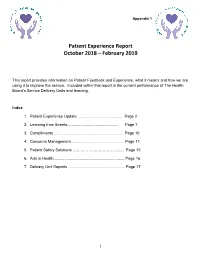
Summary Report for the Team
Appendix 1 Patient Experience Report October 2018 – February 2019 This report provides information on Patient Feedback and Experience, what it means and how we are using it to improve the service. Included within this report is the current performance of The Health Board’s Service Delivery Units and learning. Index 1. Patient Experience Update ........................................ Page 2 2. Learning from Events............................................... Page 7 3. Compliments ................................................................ Page 10 4. Concerns Management................................................. Page 11 5. Patient Safety Solutions ………………………………… Page 15 6. Arts in Health................................................................. Page 16 7. Delivery Unit Reports .................................................... Page 17 __________________________________________________________________________________________ 1 1. PATIENT EXPERIENCE 1.1 Inpatient Discharge Feedback Rates The Patient Experience Team continues to provide support and guidance to the Service Delivery Units (“SDU”) on increasing the number of surveys completed. The graph below indicates the discharge feedback rate benchmarked against the best performing Trusts for patient feedback returns in NHS England (35%). The Health Board’s aim is to increase the rate to 35%. October 2018 was 22.85%, November 2018 was 24.09%, December 2018 was 17.99%, January 2019 was 17.16% and February 2019 was 21.16%. __________________________________________________________________________________________ -

Physicians on the Front Line the Medical Workforce in Wales in 2016
Physicians on the front line The medical workforce in Wales in 2016 Phys_frontline_A4_ENG.indd 1 26/10/2016 16:12 Foreword At a glance The Royal College of Physicians (RCP) > The health sector employs an estimated president, Professor Jane Dacre, recently 129,000 workers. This equates to 8% of jobs warned that today’s NHS is ‘underdoctored, in Wales.4 1 underfunded and overstretched’. These > The NHS Wales workforce accounts for 62% observations apply as much to Wales as to of health boards’ expenditure, or almost the rest of the UK. For the Welsh NHS to £3 billion a year.5 achieve its full potential to serve the people > The medical workforce makes up 8.5% of of Wales, it requires adequate resources and the total NHS workforce in Wales. a committed, fully operational and integrated healthcare workforce, allied with good morale > The NHS in Wales spends around £350 and professional satisfaction. million to support approximately 15,000 students and trainees undertaking health- Wales suffers from recruitment and retention related education programmes.6 issues among the medical workforce, at > A third of core medical training (CMT) places both senior and junior levels. The issues were unfilled in Wales in 2016.7 underpinning these problems are varied and complex, and include geography, negative > Only 30% of Welsh medical school perceptions and a lack of inducements to undergraduates are Welsh domiciled. This encourage doctors to follow a career in compares with 85% in Northern Ireland, 8 Wales. The RCP in Wales believes that there 80% in England and 55% in Scotland. are many initiatives that we could and should > Only 39.5% of trainee physicians in Wales adopt to overcome these issues. -
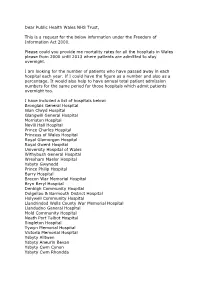
Dear Public Health Wales NHS Trust, This Is a Request for the Below
Dear Public Health Wales NHS Trust, This is a request for the below information under the Freedom of Information Act 2000. Please could you provide me mortality rates for all the hospitals in Wales please from 2000 until 2013 where patients are admitted to stay overnight. I am looking for the number of patients who have passed away in each hospital each year. If I could have the figure as a number and also as a percentage. It would also help to have annual total patient admission numbers for the same period for those hospitals which admit patients overnight too. I have included a list of hospitals below: Bronglais General Hospital Glan Clwyd Hospital Glangwili General Hospital Morriston Hospital Nevill Hall Hospital Prince Charles Hospital Princess of Wales Hospital Royal Glamorgan Hospital Royal Gwent Hospital University Hospital of Wales Withybush General Hospital Wrexham Maelor Hospital Ysbyty Gwynedd Prince Philip Hospital Barry Hospital Brecon War Memorial Hospital Bryn Beryl Hospital Denbigh Community Hospital Dolgellau & Barmouth District Hospital Holywell Community Hospital Llandrindod Wells County War Memorial Hospital Llandudno General Hospital Mold Community Hospital Neath Port Talbot Hospital Singleton Hospital Tywyn Memorial Hospital Victoria Memorial Hospital Ysbyty Alltwen Ysbyty Aneurin Bevan Ysbyty Cwm Cynon Ysbyty Cwm Rhondda Ysbyty Penrhos Stanley Ysbyty Ystrad Fawr Ystradgynlais Community Hospital Pontypridd & District Cottage Hospital (Y Bwthyn) St. Woolos Hospital CHC Local Committee Carmarthenshire Local Committee -

50 Years of the NHS in Wales.Pdf
CONTENTS Preface ........ .......... .. ............... .......... ... ... ... ..... " ... ................... ..... .. 5 Acknowledgements ........... 6 Chapter 1 Introduction .................. .. ................. ...... .................... 7 Chapter 2 Pre 1948: The legacy of the Past ........................ ... .. ..... 9-35 THE HISTORICAL PERSPECTIVE Voluntary Hospitals ..... .. ................ ....... .. 10 Municipal Hospitals .. 11 11 .,' Mr Delme Griffiths and Welsh Health Esrares, 1998 Poor Law Institutions ................... Isolation Hospitals: the spectre of epidemics ................... ... ...... 13 From Lunatic Asylums to Mental Hospitals .......... ........... ..... .. 14 THE GENESIS OF HOSPITALS IN WALES Firsr Published 1998 by Welsh Health Esrares A Tradition of Care ............... ................. ................. ........ ... .... 16 Voluntary Hospitals Take the Lead .... ........................... ... ... ... 16 All Rights Reserved. No parr of this publicarion may be reproduced, srored in a Municipal Hospitals Follow On ....... .. .... ... ........ .... .. ........... .... 19 retrieval sysrem, or transmirred, in any fonn or by any means, electronic, General Acute Hospitals .. .......... ........ ............. .... .... .. ... ....... 19 mechanical, phorocopying, recording or otherwise without the prior pennission of Infectious Diseases Hospitals .............. .................. ..... ......... 24 Mental Health Hospitals . .... ..... .................... .... ....... ... 27 the copyright owner. The Role of -

01639 648363 [email protected] Dear
Cadeirydd/Chair: Emma Woollett Prif Weithredwr/Chief Executive: Tracy Myhill gofalu am ein gilydd, cydweithio, gwella bob amser caring for each other, working together, always improving Rydym yn croesawu gohebiaeth yn y Gymraeg ac yn y Saesneg. We welcome correspondence in Welsh or English. 01639 648363 Dyddiad/Date: 20th November 2020 Ein Cyf / Our Ref: 20-J-062 [email protected] [redacted] Corporate Services [redacted] [redacted] [redacted] Headquarters 1 Talbot Gateway Baglan Port Talbot, SA12 7BR Dear [redacted], I refer to your Freedom of Information Act Request acknowledged by ourselves on 3rd November 2020. Your request sought information relating to inflammatory bowel disease. 1. The name of the named Consultant Gastroenterology lead for Inflammatory Bowel Disease Singleton Hospital – Dr Sophie Henson [email protected] Morriston & Neath Port Talbot Hospitals - Dr Mithun Nagari [email protected] 2. If no named Consultant Gastroenterology lead for Inflammatory Bowel Disease could you please supply the name of the Consultant who is the clinical lead for Gastroenterology Not applicable 3. Does your Health Board have an Inflammatory Bowel Disease clinical nurse specialist? Singleton Hospital - Louise Caie [email protected] Morriston Hospital - Sarra Wilcox [email protected] Lisa Hicks [email protected] Pencadlys BIP Bae Abertawe, Un Porthfa Talbot, Port Talbot, SA12 7BR / Swansea Bay UHB Headquarters, One Talbot Gateway, Port Talbot, SA12 7BR Bwrdd Iechyd Prifysgol Bae Abertawe yw enw gweithredu Bwrdd Iechyd Lleol Prifysgol Bae Abertawe Swansea Bay University Health Board is the operational name of Swansea Bay University Local Health Board Neath Port Talbot Hospital - Russell Thomas [email protected] 4. -

Swansea City Bus Station
where to catch your bus at Swansea City Bus Station from 1st September 2019 Stand Service Destination A X10 Cardiff via McArthur Glen Designer Outlet & Cardiff Bay D 34 Neath via Landore Park & Ride, Morfa, Llansamlet & Skewen E 8 Swansea University Bay Campus via Fabian Way Park & Ride 7 Swansea Marina 38 Neath via Bay Campus, Jersey Marine, Skewen & Neath Abbey 84 Port Talbot via Elba Crescent, Baglan & Sandfields Estate F X5 Neath via Bay Campus & Briton Ferry X7 Glynneath via Bay Campus, Jersey Marine, Neath, Resolven & Tonna X8 Banwen via Bay Campus, Jersey Marine, Neath, Aberdulais & Crynant 6 Port Tennant via Sainsbury’s, St. Thomas & SA1 (Mondays to Fridays only) 44 Grenfell Park via Maritime Quarter, Sainsbury’s & SA1 G X1 Bridgend via Sainsbury’s, Bay Campus, Port Talbot, Margam & Pyle X3 Maesteg via Sainsbury’s, Bay Campus, Port Talbot & Bryn 31 Morriston Hospital via Sainsbury’s, Bonymaen, Trallwn, Birchgrove & Llansamlet H 32 Birchgrove via Sainsbury’s, Bonymaen & Trallwn 33 Frederick Place via Sainsbury’s, Bonymaen & Trallwn J 36 Morriston via Rail Station, Manselton, Brynhyfryd, Treboeth, Clase & DVLA K 4 Morriston Hospital via Rail Station, Liberty Stadium, Plasmarl & Morriston 25 Blaen-y-Maes via Rail Station, Manselton, First Cymru Depot & Caereithin Cross L 30 Rhyd-y-Felin via Rail Station, Morfa, Bonymaen & Trallwn M 28 Penplas via Rail Station, Cwmbwrla, Penlan, Heol Cadifor & First Cymru Depot 110 Llanelli via Rail Station, Garden Village, Gorseinon, Loughor & Bynea N 111 Llanelli via Rail Station, Garden Village, -

4A Bus Time Schedule & Line Route
4A bus time schedule & line map Singleton Hospital - Morriston Hospital via Civic 4A Centre, Liberty Stadium, Morriston Cross & View In Website Mode Llanllienwen Close The 4A bus line (Singleton Hospital - Morriston Hospital via Civic Centre, Liberty Stadium, Morriston Cross & Llanllienwen Close) has 3 routes. For regular weekdays, their operation hours are: (1) Morriston Hospital: 7:36 PM - 10:50 PM (2) Singleton: 8:59 AM - 5:59 PM (3) Swansea: 8:33 PM - 10:03 PM Use the Moovit App to ƒnd the closest 4A bus station near you and ƒnd out when is the next 4A bus arriving. Direction: Morriston Hospital 4A bus Time Schedule 47 stops Morriston Hospital Route Timetable: VIEW LINE SCHEDULE Sunday 9:26 AM - 10:50 PM Monday 7:36 PM - 10:50 PM Hospital, Singleton Tuesday 7:36 PM - 10:50 PM Swansea University Campus, Singleton Wednesday 7:36 PM - 10:50 PM Swansea University, Singleton Thursday 7:36 PM - 10:50 PM Brynmill Lane, Singleton Friday 7:36 PM - 10:50 PM Recreation Ground, Brynmill Saturday 7:36 PM - 10:50 PM Cricket Ground, St Helen's The Slip, Guildhall 4A bus Info Civic Centre Level Access 3, Swansea Direction: Morriston Hospital Stops: 47 Trip Duration: 54 min Civic Centre 1, Swansea Line Summary: Hospital, Singleton, Swansea Dunvant Place, Swansea University Campus, Singleton, Swansea University, Singleton, Brynmill Lane, Singleton, Recreation Bus Station M, Swansea Ground, Brynmill, Cricket Ground, St Helen's, The Slip, Guildhall, Civic Centre Level Access 3, Swansea, Civic The Kingsway, Swansea Centre 1, Swansea, Bus Station M, Swansea, -

Abertawe Bro Morgannwg University Health Board, Morriston Hospital and Singleton Hospital
Hospital Inspection (Unannounced) Abertawe Bro Morgannwg University Health Board, Morriston Hospital and Singleton Hospital 9 and 10 September 2015 This publication and other HIW information can be provided in alternative formats or languages on request. There will be a short delay as alternative languages and formats are produced when requested to meet individual needs. Please contact us for assistance. Copies of all reports, when published, will be available on our website or by contacting us: In writing: Communications Manager Healthcare Inspectorate Wales Welsh Government Rhydycar Business Park Merthyr Tydfil CF48 1UZ Or via Phone: 0300 062 8163 Email: [email protected] Fax: 0300 062 8387 Website: www.hiw.org.uk Digital ISBN 978-1-4734-5233-6 © Crown copyright 2015 Contents 1. Introduction ........................................................................................................ 2 2. Methodology....................................................................................................... 3 3. Context ............................................................................................................... 6 4. Summary ............................................................................................................ 7 5. Findings ............................................................................................................. 9 Quality of the Patient Experience ...................................................................... 9 Delivery of Safe and Effective Care ................................................................