Welsh Ambulance Services NHS Trust Has
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Legal & Policy Briefing
LEGAL & POLICY BRIEFING Access to Healthcare for Migrants in Wales AUTHOR: JONATHAN PRICE PUBLISHED: February 2016 http://www.wrc.wales/migration-information LEGAL & POLICY BRIEFING: Access to Healthcare for Migrants in Wales TABLE OF CONTENTS Introduction .............................................................................................3 How this briefing is structured ..................................................................3 The NHS in Wales .....................................................................................3 Primary care .............................................................................................3 Secondary care .........................................................................................4 Immigration Health Surcharge ..................................................................8 Further resources ................................................................................... 10 Acknowledgments .................................................................................. 10 HTTP://WWW.WRC.WALES/MIGRATION-INFORMATION PAGE 2 LEGAL & POLICY BRIEFING: Access to Healthcare for Migrants in Wales Introduction This briefing provides a general overview of migrants’ entitlement to NHS healthcare services in Wales. A broad range of migrant groups are considered here, including mobile EU citizens, asylum seekers, refugees and third country nationals, including those with irregular immigration status. Information on access to both primary and secondary healthcare services -

Our Health, Our Health Service Green Paper
Number: WG25325 Welsh Government Green Paper Our Health, Our Health Service Date of issue: 6 July 2015 Action required: Responses by 20 November 2015 Digital ISBN 978 1 4734 3673 2 © Crown Copyright 2015 Overview Data protection This consultation is to promote discussion and How the views and information you give gather views to help inform the potential for us will be used future legislation in the Fifth Assembly with Any response you send us will be seen in full regards to improving quality and governance by Welsh Government staff dealing with the in the NHS in Wales. issues which this consultation is about. It may also be seen by other Welsh Government staff How to respond to help them plan future consultations. Please respond by answering the questions at The Welsh Government intends to publish a the back of this document and sending it to: summary of the responses to this document. We may also publish responses in full. [email protected] Normally, the name and address (or part of Or by post to: the address) of the person or organisation who sent the response are published with Matthew Tester the response. This helps to show that the Healthcare Quality Division consultation was carried out properly. If you Department of Health and Social Services do not want your name or address published, Welsh Government please tell us this in writing when you send Cathays Park your response. We will then blank them out. Cardiff CF10 3NQ Names or addresses we blank out might still get published later, though we do not think this would happen very often. -
Information for Candidates APPOINTMENT of NON
NHS Trust Non-executive Director Information for Candidates APPOINTMENT OF NON-EXECUTIVE DIRECTOR OF WELSH AMBULANCE SERVICES NHS TRUST NHS Trust Non-executive Director Diversity Statement The Welsh Government believes that public bodies should have board members who reflect Welsh society - people from all walks of life - to help them understand people's needs and make better decisions. This is why the Welsh Government is encouraging a wide and diverse range of individuals to apply for appointments to public bodies. Applications are particularly welcome from all under-represented groups including women, people under 30 years of age, members of ethnic minorities, disabled people, lesbian, gay, bisexual and trans people. Positive about Disability The Welsh Government operates a Positive about Disabled People scheme and welcome applications from people with disabilities. The scheme guarantees an interview to disabled people if they meet the minimum criteria for the post. The application form also enables you to detail any specific needs or equipment that you may need if invited to attend an interview. NHS Trust Non-executive Director Background and Context The Welsh Government’s vision for the NHS in Wales is “to create world-class health”. This vision is set out in Together for Health, and is based on providing more community services closer to home, alongside specialist centres of excellence, which give better results for patients. Who does what in the NHS in Wales? The Minister for Health and Social Services is responsible for all aspects of the NHS in Wales. Details of the Ministers responsibilities can be found here http://gov.wales/about/cabinet/cabinetm/markdrakeford The National Delivery Group, forms part of the Welsh Government’s Health and Social Services (HSSG) Group, and is responsible for overseeing the development and delivery of NHS services across Wales. -

NHS Wales Decarbonisation Strategic Delivery Plan
NHS Wales Decarbonisation Strategic Delivery Plan 2021-2030 (including Technical Appendices) Published March 2021 NHS Wales Decarbonisation Strategic Delivery Plan Who we are Established in 2001, the Carbon Trust works with businesses, governments and institutions around the world, helping them contribute to, and benefit from, a more sustainable future through carbon reduction, resource efficiency strategies, and commercialising low carbon businesses, systems and technologies. The Carbon Trust: • works with corporates and governments, helping them to align their strategies with climate science and meet the goals of the Paris Agreement; • provides expert advice and assurance, giving investors and financial institutions the confidence that green finance will have genuinely green outcomes; and • supports the development of low carbon technologies and solutions, building the foundations for the energy system of the future. Headquartered in London, the Carbon Trust has a global team of over 200 staff, representing over 30 nationalities, based across five continents. 1 NHS Wales Decarbonisation Strategic Delivery Plan The Carbon Trust’s mission is to accelerate the move to a sustainable, low carbon economy. It is a world leading expert on carbon reduction and clean technology. As a not-for-dividend group, it advises governments and leading companies around the world, reinvesting profits into its low carbon mission. The NHS Wales Shared Services Partnership (NWSSP) is an independent organisation, owned and directed by NHS Wales. NWSSP supports -
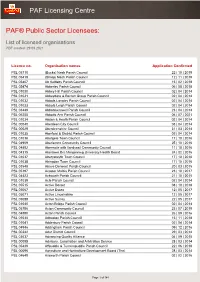
List of Licensed Organisations PDF Created: 29 09 2021
PAF Licensing Centre PAF® Public Sector Licensees: List of licensed organisations PDF created: 29 09 2021 Licence no. Organisation names Application Confirmed PSL 05710 (Bucks) Nash Parish Council 22 | 10 | 2019 PSL 05419 (Shrop) Nash Parish Council 12 | 11 | 2019 PSL 05407 Ab Kettleby Parish Council 15 | 02 | 2018 PSL 05474 Abberley Parish Council 06 | 08 | 2018 PSL 01030 Abbey Hill Parish Council 02 | 04 | 2014 PSL 01031 Abbeydore & Bacton Group Parish Council 02 | 04 | 2014 PSL 01032 Abbots Langley Parish Council 02 | 04 | 2014 PSL 01033 Abbots Leigh Parish Council 02 | 04 | 2014 PSL 03449 Abbotskerswell Parish Council 23 | 04 | 2014 PSL 06255 Abbotts Ann Parish Council 06 | 07 | 2021 PSL 01034 Abdon & Heath Parish Council 02 | 04 | 2014 PSL 00040 Aberdeen City Council 03 | 04 | 2014 PSL 00029 Aberdeenshire Council 31 | 03 | 2014 PSL 01035 Aberford & District Parish Council 02 | 04 | 2014 PSL 01036 Abergele Town Council 17 | 10 | 2016 PSL 04909 Aberlemno Community Council 25 | 10 | 2016 PSL 04892 Abermule with llandyssil Community Council 11 | 10 | 2016 PSL 04315 Abertawe Bro Morgannwg University Health Board 24 | 02 | 2016 PSL 01037 Aberystwyth Town Council 17 | 10 | 2016 PSL 01038 Abingdon Town Council 17 | 10 | 2016 PSL 03548 Above Derwent Parish Council 20 | 03 | 2015 PSL 05197 Acaster Malbis Parish Council 23 | 10 | 2017 PSL 04423 Ackworth Parish Council 21 | 10 | 2015 PSL 01039 Acle Parish Council 02 | 04 | 2014 PSL 05515 Active Dorset 08 | 10 | 2018 PSL 05067 Active Essex 12 | 05 | 2017 PSL 05071 Active Lincolnshire 12 | 05 -

Bundle Public Board 29 March 2018
Bundle Public Board 29 March 2018 2.6 Report of the Chief Executive / Adroddiad y Prif Weithredwr Presenter: Steve Moore Report of the Chief Executive March 2018 App A - Register of Sealings March 2018 Board App B - Consultation Report March 2018 App C - Zero Based Review of HDdUHB 2.6 Report of the Chief Executive / Adroddiad y Prif Weithredwr 1 Report of the Chief Executive March 2018 CYFARFOD BWRDD PRIFYSGOL IECHYD UNIVERSITY HEALTH BOARD MEETING DYDDIAD Y CYFARFOD: 29 March 2018 DATE OF MEETING: TEITL YR ADRODDIAD: Chief Executive’s Report TITLE OF REPORT: CYFARWYDDWR ARWEINIOL: Steve Moore, Chief Executive LEAD DIRECTOR: SWYDDOG ADRODD: Sian-Marie James, Head of Corporate Office REPORTING OFFICER: Pwrpas yr Adroddiad (dewiswch fel yn addas) Purpose of the Report (select as appropriate) Ar Gyfer Penderfyniad/For Decision ADRODDIAD SCAA SBAR REPORT Sefyllfa / Situation The purpose of this Report is to: • Update the Board on relevant matters undertaken as Chief Executive of Hywel Dda University Health Board (the UHB) since the previous Board meeting held on 25 January 2018; and • Provide an overview of the current key issues, both at a local and national level, within NHS Wales. Cefndir / Background This Report provides the opportunity to present items to the Board to demonstrate areas of work that are being progressed and achievements that are being made, which may not be subject to prior consideration by a Committee of the Board, or may not be directly reported to the Board through Board reports. Asesiad / Assessment 1. Register of Sealings The UHB’s Common Seal has been applied to legal documents and a record of the sealing of these documents has been entered into the Register kept for this purpose. -

Integrated Medium Term Plan
1 CONTENTS Acronym Table 5 Message from the Chair and Chief Executive 8 Executive Summary 9 Part 1 Delivery of Our 2015/16 Plan 13 1.1 The New Clinical Response Model……………………………………............. 13 1.2 Quality and Operational Performance Trajectories…………………………... 15 1.3 2015/16 Strategic Change Portfolio …………………………………………… 18 1.4 Maturing Commissioning Arrangements and Increased Focus on Financial Strategy…………………………………………………………………………… 22 Part 2 Organisational and Strategic Context 24 This section, coupled with Part 1, serves as a high level diagnostic of the context within which we operate – it answers the “where are we now?” question. 2.1 Profile of the Trust……………………………………………………………….. 24 2.2 Our Demand & Activity………………………………………………………….. 32 2.3 The Five-Step Ambulance Care Pathway, Commissioning Quality & Delivery Framework, Understanding our Populations and Changes………. 33 2.4 National Policy Context………………………………………………………….. 37 2.5 Major Conditions, Older People and Frailty…………………………………… 42 2.6 Becoming a Listening and Learning Organisation………………………….... 43 2.7 NHS Wales Strategic Change Agenda………………………………………… 44 2.8 Service Change with Blue Light Partners……………………………………... 48 2.9 Ensuring Integration with Our Partners’ Three Year Plans………………….. 49 2.10 The Organisation and Prudent Healthcare……………………………………. 50 2.11 Treating People Fairly – Equality, Diversity & Human Rights………………. 51 2.12 Other Strategic Workforce and OD Drivers…………………………………… 54 Part 3 Creating Our Strategic Framework 57 This section sets the strategic framework for the organisation. It sets out our ambition and answers the “where do we want to go?” question. 3.1 Our Vision, Purpose and Behaviours………………………………………….. 57 3.2 Our Strategic Aims………………………………………………………………. 58 3.3 Our Priorities……………………………………………………………………… 59 3.4 Our Strategy Map………………………………………………………………… 63 3.5 Our Performance Ambitions………………………………………………........ -

Glossary of Health and Care Terms
Glossary of health and care terms May 2021 This glossary provides a summary of organisations and general terms used within the health and care sector in Wales. The glossary provides some of the most common words and phrases used. 0 - 9 Acute Medical Unit (AMU) 111 An AMU is the first point of entry for patients referred to hospital as The NHS Wales 111 service is a free- emergencies by their GP and those to-call, non-emergency medical requiring admission from the helpline, available 24 hours a day, to Emergency Department. be used for health information, advice and access to urgent care. The service is currently operational in the Aneurin Add to Your Life Bevan University Health Board (UHB), Cwm Taf Morgannwg UHB, Hywel Dda ‘Add to Your Life’ is an online health- UHB, Powys Teaching Health Board check, which provides assessment (THB) and Swansea Bay UHB areas. It and community-based support to is anticipated that 111 will be rolled out enable over 50s in Wales to assess across Wales by the end of 2021. and improve their own health. A Additional Learning Needs and Education Tribunal Act 2018 A Regional Collaboration for Health (ALNET) (ARCH) The ALNET Act 2018 establishes a ARCH is a regional partnership made statutory framework for supporting up of Swansea University, Swansea children and young people with Bay UHB and Hywel Dda UHB. The additional learning needs (ALN) from ARCH partners work to improve the birth; whilst they are in school; and, if health, wealth and wellbeing of the they are over compulsory school age, people of South West Wales. -

{Department – Welsh}
Information Governance Team Vera Vallins Office Bronllys Hospital Bronllys Brecon Powys LD3 0LS Tel: 01874 712763 Fax: 01874 712756 Our ref: IG/FOI/19.R.233 23 September 2019 Sent via email to: [email protected] Dear Sir, Request under the Freedom of Information Act 2000 I write further to your request for information which was received on 29 August 2019 , to confirm, in accordance with S.1(1)(a) of the Freedom of Information Act 2000, that Powys Teaching Health Board (PTHB) holds part of the information that you require. For ease of reference your request is set out below and our response follows: Your Freedom of Information (FOI) Request: Who have you commissioned to provide any of the following orthotic devices which are vital to prevent damage and pain to the lower spine in long-term manual wheelchair users: 1. A measured spinal-restriction-brace, designed to stop long-term wheelchair users prevent stress induced damage and pain to their lumbar-sacrum region, where the spine joins the pelvis; 2. Power-assist motors such as: * Trike attachments * Pushers such as the Alber Smoov and Permobile Smart-drive * Joystick- and push-rim- controlled hub motors? 3. Please send me the minutes of the meetings discussing this essential support for wheelchair users, and a copy of the contract you commissioned. 4. If nothing has been commissioned, or if nothing has been considered for commissioning, what is the official protocol to get the consideration of such orthotic devices put onto the agenda? Is there a form members of the public can fill in? Pencadlys Headquarters Tŷ Glasbury, Ysbyty Bronllys, Glasbury House, Bronllys Hospital Aberhonddu, Powys LD3 0LU Brecon, Powys LD3 0LU Ffôn: 01874 711661 Tel: 01874 711661 Rydym yn croesawu gohebiaeth Gymraeg We welcome correspondence in Welsh Bwrdd Iechyd Addysgu Powys yw enw gweithredd Bwrdd Iechyd Lleol Powys Teaching Health Board is the operational name of Addysgu Powys Powys Teaching Local Health Board 5. -

(Public Pack)Agenda Document for Petitions Committee, 02/03/2021 09
------------------------ Public Document Pack ------------------------ Agenda - Petitions Committee Meeting Venue: For further information contact: Video Conferencing Via Zoom Graeme Francis - Committee Clerk Meeting date: 2 March 2021 Kayleigh Imperato – Deputy Clerk Meeting time: 09.00 0300 200 6373 [email protected] ------ In accordance with Standing Order 34.19, the Chair has determined that the public are excluded from the Committee's meeting in order to protect public health. This meeting will be broadcast live on www.senedd.tv 1 Introduction, apologies, substitutions and declarations of interest (Pages 1 - 43) 2 New Covid 19 petitions 2.1 P-05-1118 Allow parents of under 1 year old to form a support bubble in new Tier 4 Covid restrictions (Pages 44 - 47) 2.2 P-05-1123 Raise the priority of non-NHS public facing key workers in the roll out of the Covid-19 vaccine (Pages 48 - 51) 2.3 P-05-1124 Allow two individuals from two different households to meet for exercise in alert level 4 (Pages 52 - 53) 2.4 P-05-1127 Reduce the fee limit for all Welsh universities due to COVID-19 requirement of distanced learning (Pages 54 - 57) 2.5 P-05-1128 Cancel externally set ‘assessments’ in 2021 for AS and A levels and only use teacher assessed grades (Pages 58 - 62) 2.6 P-05-1135 Targeted funding for residential outdoor education centres, now unable to operate for 12 months (Pages 63 - 70) 2.7 P-05-1136 Allow Welsh residents to travel for fishing the same as our counterparts in England (Pages 71 - 75) 2.8 P-05-1139 Extend stamp duty relief -

Bundle Quality, Safety and Experience Committee 17 December 2019
Bundle Quality, Safety and Experience Committee 17 December 2019 Agenda attachments 00 - Agenda Dec 2019 - v3.docx 1 STANDING ITEMS 1.1 Welcome and Introductions Susan Elsmore 1.2 Apologies for Absence Susan Elsmore 1.3 Declarations of Interest Susan Elsmore 1.4 Minutes of the Committee Meeting held on 17 September 2019 and 15 October 2019 Susan Elsmore 1.4 - QSE Public Mins 17.09.19 NF Final.docx 1.4.1 - QSE Mins 15.10.19 v2 - AF.NF Final.docx 1.5 Action Log - 17 September 2019 and 15 October 2019 Susan Elsmore 1.5 Action Log Sep 2019.docx 1.6 Chair's Action taken since last meeting Susan Elsmore 1.7 Clinical Board Assurance Report: Clinical Diagnostics and Therapeutics Clinical Board Aled Roberts 1.7 - CD&T Board Assurance Report.pdf 2 PATIENT STORY 3 ITEMS FOR REVIEW AND ASSURANCE 3.1 Healthcare Standards Self-Assessment Plan and Progress Update Carol Evans 3.1 -Health and Care standards Dec 2019_v 4 FINAL.docx 3.1.1 - Appendix 1 - ISN 2019 003 - Resuscitation trolley checks.pdf 3.1.2 - Appendix 2 H&CS_Dec_2019 v3 FINAL.docx 3.2 Point of Care Testing Stuart Walker 3.2 - QSE POCT SBAR 171219 (002) Final.docx 3.3 Update on Stroke Rehabilitation and Model Workforce Verbal - Fiona Jenkins 3.4 Local Clinical Audit Plan Update Stuart Walker 3.4 - Clinical Audit Plan Update -18.12.18.docx 3.4.1 - Local Clinial Audit appendix 1.xlsx 3.5 Cancer Peer Review Stuart Walker 3.6 - Peer Review report for QSE Dec 19.docx 3.6 Internal Inspections Ruth Walker 3.6 - Internal Inspections QSE.docx 3.7 Patient Notification Exercises in Cardiff and Vale -

Integrated Medium Term Plan Summary 2017-18
Welsh Ambulance Services NHS Trust Integrated Medium Term Plan Summary 2017-2018 Published: MARCH 2017 www.ambulance.wales.nhs.uk www.facebook.com/welshambulanceservice @WelshAmbulance 0 1- INTRODUCTION Welcome to the summary document of our Integrated Medium Term Plan (IMTP). We are conscious that our IMTP is a lengthy, technical document that many may not have the time to read. This summary is our way of trying to make such an important document more reader friendly. The IMTP document is a requirement of Welsh Government for all Health Boards and Trusts in NHS Wales and it sets out our direction for the next three years stating our priorities, challenges and main risks. Throughout the main plan we commit ourselves to 48 actions which can be viewed in more detail in the main IMTP. We believe our IMTP is vital for us in WAST, regardless of it being a necessity for Welsh Government, to ensure there is a clear plan in place for the organisation. In a message from the Chair and Chief Executive they have stated how reshaping an ambulance service is a long term process and therefore a need to focus on our services and how we deliver them especially as the type of patients we are seeing are changing within our ageing population. This can only be achievable with support from our partners and ensuring our teams have the right skills. We hope you find this summary a useful insight into the Trust and the work we are continuing to do to improve the quality of care we deliver to our patients.