Paper 1: Cwm Taf Morgannwg University Health Board , Item 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Cwm Taf Morgannwg University Health Board Job Description
CWM TAF MORGANNWG UNIVERSITY HEALTH BOARD JOB DESCRIPTION POST: Consultant Physician in Geriatric & General Medicine SALARY: £72,927 - £94,679 per annum DIRECTORATE: Medicine and A&E BASE: Royal Glamorgan Hospital The post holder will also be required to provide services at other hospital sites. Introduction This is a new post, which is being created to develop and improve the Geriatric Medicine services in Cwm Taf Morgannwg University Health Board. The post will be subject to the terms and conditions of service governing the appointment of Medical and Dental Staff in Wales, and to the Health Board's terms and conditions as appropriate. The candidate to be appointed will be required to be fully registered with the General Medical Council, to hold, or to be within 6 months of gaining, a Certificate of Completion of Training in both Geriatric Medicine and General Internal Medicine, and to be on the Specialist Register. The post holder will be joining a dynamic, forward looking and innovative Geriatric Medicine team. The post holder will be based at Royal Glamorgan Hospital in Llantrisant, where the Health Board has acute hospital beds covering a range of medical and surgical specialities. The post holder will be expected to help and develop Geriatric Medicine services provided by the Health Board at the Royal Glamorgan Hospital and in the community setting. A sub-speciality interest will be encouraged but there is flexibility to support personal development in this regard. Key to the development of services will be to develop clinical relationships with the colleagues in the Directorate and Local Health Board as well as strengthening working relationships with Primary Care colleagues in order to develop services locally. -
Information for Candidates APPOINTMENT of NON
NHS Trust Non-executive Director Information for Candidates APPOINTMENT OF NON-EXECUTIVE DIRECTOR OF WELSH AMBULANCE SERVICES NHS TRUST NHS Trust Non-executive Director Diversity Statement The Welsh Government believes that public bodies should have board members who reflect Welsh society - people from all walks of life - to help them understand people's needs and make better decisions. This is why the Welsh Government is encouraging a wide and diverse range of individuals to apply for appointments to public bodies. Applications are particularly welcome from all under-represented groups including women, people under 30 years of age, members of ethnic minorities, disabled people, lesbian, gay, bisexual and trans people. Positive about Disability The Welsh Government operates a Positive about Disabled People scheme and welcome applications from people with disabilities. The scheme guarantees an interview to disabled people if they meet the minimum criteria for the post. The application form also enables you to detail any specific needs or equipment that you may need if invited to attend an interview. NHS Trust Non-executive Director Background and Context The Welsh Government’s vision for the NHS in Wales is “to create world-class health”. This vision is set out in Together for Health, and is based on providing more community services closer to home, alongside specialist centres of excellence, which give better results for patients. Who does what in the NHS in Wales? The Minister for Health and Social Services is responsible for all aspects of the NHS in Wales. Details of the Ministers responsibilities can be found here http://gov.wales/about/cabinet/cabinetm/markdrakeford The National Delivery Group, forms part of the Welsh Government’s Health and Social Services (HSSG) Group, and is responsible for overseeing the development and delivery of NHS services across Wales. -
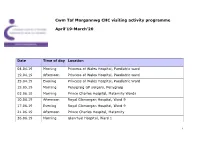
Cwm Taf Morgannwg CHC Visiting Activity Programme April'19-March'20
Cwm Taf Morgannwg CHC visiting activity programme April’19-March’20 Date Time of day Location 04.04.19 Morning Princess of Wales Hospital, Paediatric ward 19.04.19 Afternoon Princess of Wales Hospital, Paediatric ward 25.04.19 Evening Princess of Wales Hospital, Paediatric Ward 15.05.19 Morning Penygraig GP surgery, Penygraig 03.06.19 Morning Prince Charles Hospital, Maternity Wards 10.06.19 Afternoon Royal Glamorgan Hospital, Ward 9 17.06.19 Evening Royal Glamorgan Hospital, Ward 9 21.06.19 Afternoon Prince Charles Hospital, Maternity 26.06.19 Morning Glanrhyd Hospital, Ward 1 1 Date Time of day Location 27.06.19 Afternoon Glanrhyd Hospital, Ward 1 03.07.19 Morning Ysbyty Cwm Rhondda, Ward A1 04.07.19 Afternoon Prince Charles Hospital, Maternity Wards 11.07.19 Morning Royal Glamorgan Hospital, Ward 6 16.07.19 Afternoon Princess of Wales Hospital, Acute Medical Assessment Unit 22.07.19 Morning Princess of Wales Hospital, Acute Medical Assessment Unit 22.07.19 Evening Royal Glamorgan Hospital, Ward 6 24.07.19 Afternoon Ysbyty Cwm Rhondda, Ward A1 05.08.19 Afternoon Prince Charles Hospital, Ward 4 07.08.19 Morning Royal Glamorgan Hospital, Ward 14 14.08.19 Morning Prince Charles Hospital, Ward 4 14.08.19 Afternoon Royal Glamorgan Hospital, Ward 14 19.08.19 Evening Royal Glamorgan Hospital, Ward 14 21.08.19 Evening Prince Charles Hospital, Ward 4 18.09.19 Afternoon Prince Charles Hospital, Maternity Unit 19.09.19 Morning Royal Glamorgan Hospital, Maternity Unit 2 Date Time of day Location 04.12.19 Afternoon Ysbyty Cwm Rhondda, Ward D4 09.12.19 -

Hospital Name Country Location
Hospital Name Country Location 1 Tameside Hospital NHS Foundation Trust England Ashton-under-Lyne 2 Barnsley Hospital NHS Foundation Trust England Barnsley 3 Royal National Hospital for Rheumatic Diseases England Bath 4 Royal United Hospitals Bath NHS Foundation Trust England Bath 5 Bedford Hospital NHS Trust England Bedford 6 South Central Ambulance Service NHS Foundation Trust England Bicester 7 Wirral Community NHS Trust England Birkenhead 8 Birmingham Children's Hospital NHS Foundation Trust England Birmingham 9 Heart Of England NHS Foundation Trust England Birmingham 10 Sandwell and West Birmingham Hospitals NHS Trust England Birmingham 11 University Hospital Birmingham NHS Foundation Trust England Birmingham 12 Birmingham and Solihull Mental Health NHS Foundation Trust England Birmingham 13 Birmingham Community Healthcare NHS Foundation Trust England Birmingham 14 Birmingham Women's NHS Foundation Trust England Birmingham 15 The Royal Orthopaedic Hospital NHS Foundation Trust England Birmingham 16 Blackpool Teaching Hospitals NHS Foundation Trust England Blackpool 17 Bolton NHS Foundation Trust England Bolton 18 The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust England Bournmouth 19 Poole Hospital NHS Foundation Trust England Bournmouth 20 Bradford Teaching Hospitals NHS Foundation Trust England Bradford 21 Bradford District NHS Foundation Trust England Bradford 22 South East Coast Ambulance Service NHS Foundation Trust England Bridgwater 23 Sussex Community NHS Foundation Trust England Brighton 24 Brighton and -
The Future of Stroke Care in Wales Report of the Inquiry Into the Implementation of the Welsh Government’S Stroke Delivery Plan
Cross Party Group on Stroke The Future of Stroke Care in Wales Report of the inquiry into the implementation of the Welsh Government’s Stroke Delivery Plan March 2020 The Cross Party Contents Group on Stroke The following Assembly Members are members of the Cross Party Group Foreword 4 on Stroke: • Dr Dai Lloyd AM (Chair) Executive summary 6 • Neil Hamilton AM • Huw Irranca-Davies AM Background 8 • Adam Price AM • Nick Ramsay AM About the inquiry 9 The Cross Party Group on Stroke is facilitated by the Stroke Association, Preventing stroke 11 which compiled this report. The Cross Party Group on Stroke would like Fast and effective acute care 18 to thank all those individuals and organisations who took part in the inquiry, particularly those who gave Life after stroke 28 either oral or written evidence. A full list of those who provided evidence can be The stroke workforce 37 found in Appendix Two. The Cross Party Group on Stroke The future of the Stroke Delivery Plan 43 can be contacted on [email protected] Appendix one: Full list of recommendations 48 Appendix two: Organisations who provided evidence 50 Foreword My fellow members and I are pleased to present the final report of the Cross A new, strengthened model of delivery and accountability accompanied by the Party Group’s inquiry into the implementation of the Welsh Government’s Stroke highest quality hyperacute stroke units would enable the other challenges set out in Delivery Plan. this report to be overcome, such as attracting the best possible staff to deliver vital rehabilitation and game-changing treatment such as thrombectomy. -

NHS Wales Decarbonisation Strategic Delivery Plan
NHS Wales Decarbonisation Strategic Delivery Plan 2021-2030 (including Technical Appendices) Published March 2021 NHS Wales Decarbonisation Strategic Delivery Plan Who we are Established in 2001, the Carbon Trust works with businesses, governments and institutions around the world, helping them contribute to, and benefit from, a more sustainable future through carbon reduction, resource efficiency strategies, and commercialising low carbon businesses, systems and technologies. The Carbon Trust: • works with corporates and governments, helping them to align their strategies with climate science and meet the goals of the Paris Agreement; • provides expert advice and assurance, giving investors and financial institutions the confidence that green finance will have genuinely green outcomes; and • supports the development of low carbon technologies and solutions, building the foundations for the energy system of the future. Headquartered in London, the Carbon Trust has a global team of over 200 staff, representing over 30 nationalities, based across five continents. 1 NHS Wales Decarbonisation Strategic Delivery Plan The Carbon Trust’s mission is to accelerate the move to a sustainable, low carbon economy. It is a world leading expert on carbon reduction and clean technology. As a not-for-dividend group, it advises governments and leading companies around the world, reinvesting profits into its low carbon mission. The NHS Wales Shared Services Partnership (NWSSP) is an independent organisation, owned and directed by NHS Wales. NWSSP supports -

Hospitals in Wales Thank You for Your Request Which I Re
Ein cyf/Our ref: ATISN 12891 22 January 2019 Dear , ATISN 12891 – Hospitals in Wales Thank you for your request which I received on 14 January 2019. You asked for the following information: A list of Welsh Hospitals per trust. The information you requested is attached in annex A. If you are dissatisfied with the Welsh Government’s handling of your request, you can ask for an internal review within 40 working days of the date of this response. Requests for an internal review should be addressed to the Welsh Government’s Freedom of Information Officer at: Information Rights Unit, Welsh Government, Cathays Park, Cardiff, CF10 3NQ or Email: [email protected] Please remember to quote the ATISN reference number above. You also have the right to complain to the Information Commissioner. However, please note the Commissioner will not normally investigate a complaint until it has been through our own internal review process. The Information Commissioner can be contacted at: Grŵp Iechyd a Gwasanaethau Cymdeithasol Health and Social Services Group E-bost E-mail: Parc Cathays Cathays Park [email protected] Caerdydd Cardiff CF10 3NQ Rydym yn croesawu derbyn gohebiaeth yn Gymraeg. Byddwn yn ateb gohebiaeth a dderbynnir yn Gymraeg yn Gymraeg ac ni fydd gohebu yn Gymraeg yn arwain at oedi. We welcome receiving correspondence in Welsh. Any correspondence received in Welsh will be answered in Welsh and corresponding in Welsh will not lead to a delay in responding. Information Commissioner’s Office, Wycliffe House, Water Lane, Wilmslow, Cheshire, SK9 5AF The request you sent me contains personal information about you – for example, your name and address. -

Carers A-Z Guide Cwm Taf Carers A-Z Guide
Cwm Taf Carers A-Z Guide Welcome from Cwm Taf Carers Champions Carers play a vital role in the provision of care, making an enormous contribution to supporting their loved ones in the community. They spend a great deal of their own valuable time and energy caring for vulnerable people and we are committed to ensuring that they are supported in this endeavour. We hope that this A-Z Guide, produced jointly by Merthyr Tydfil and Rhondda Cynon Taf Councils and Cwm Taf University Health Board in a response to the Carers Strategies (Wales) Measure, will help to achieve better outcomes for all by providing a central resource of up to date information about support services that are targeted to meet the needs of carers and other residents living in the Cwm Taf area. Councillor Bill Smith Carers Champion - Merthyr Tydfil CBC Councillor Mike Forey Carers Champion - Rhondda Cynon Taf CBC Independent Board Member Maria Thomas Carers Champion - Cwm Taf Local Health Board Cwm Taf Carers A-Z Guide Introduction This is the second edition of the Cwm Taf Carers Guide. It was originally formed by merging information from Merthyr and RCT’s Carers guides and has been produced to provide you with the information you may need to get the support necessary to help you to meet your caring responsibilities effectively. The useful contacts are listed alphabetically under the following headings to help you to find the specific information you require as easily as possible. We hope that the publication proves to be useful and helps you to better understand the services available locally and how to access them. -
Course Manual O P E N
DOCTORSDOCTORS ACADEMY ACADissemin ating DEMYMedical Knowl edge an d Skills Globally Disseminating Medical Knowledge and Skills Globally 6th Laparoscopic Colorectal Surgery Course & Master Class Dates: 7th and 8th May 2014 Venue: Prince Charles Hospital, Merthyr Tydfil, Wales Course Manual O P E N This course is accredited by the Royal College of Surgeons of Edinburgh. Attendance in this course entitles the delegate to receive 12 CPD points. Doctors Academy Publications Laparoscopic Colorectal Surgery Course & Master Class Prince Charles Hospital, Merthyr Tydfil, Wales Contents Welcome letter 3 Faculty & Orga nise r list 4 Faculty Profiles 5 About the Hospital 6 Course Programme 7 Selected Reading Material and Relevant Publications Steps for Laparoscopic Anterior Resection of Rectum 10 Steps for Laparoscopic Right hemicolectomy 11 The Merthyr Coaching Tool for Laparoscopic Colorectal Surgery 12 Preceptorship Programme 16 Laparoscopic Colorectal Surgery Training and Research - PC H contrib utions 17 Publications 18 Notes 22 Course dinner 24 Acknowledgement 25 Course Manual www.doctorsacademy.org Doctors Academy Publications Laparoscopic Colorectal Surgery Course & Master Class 33 Prince Charles Hospital, Merthyr Tydfil, Wales Welcome Dear Delegate, I am pleased to welcome you to the 6th Laparoscopic Colorectal Course & Masterclass at Prince Charles Hospital in Merthyr Tydfil. The course, started in 2010, is aimed at surgical trainees as well as consultants wishing to gain expertise in this field and has been very popular and very well received in previous years. Consequent upon its success, the course is now run biannually. The course is accredited by the Royal College of Surgeons of Edinburgh and the college awards 12 CPD points for attendance. -
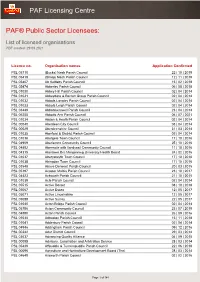
List of Licensed Organisations PDF Created: 29 09 2021
PAF Licensing Centre PAF® Public Sector Licensees: List of licensed organisations PDF created: 29 09 2021 Licence no. Organisation names Application Confirmed PSL 05710 (Bucks) Nash Parish Council 22 | 10 | 2019 PSL 05419 (Shrop) Nash Parish Council 12 | 11 | 2019 PSL 05407 Ab Kettleby Parish Council 15 | 02 | 2018 PSL 05474 Abberley Parish Council 06 | 08 | 2018 PSL 01030 Abbey Hill Parish Council 02 | 04 | 2014 PSL 01031 Abbeydore & Bacton Group Parish Council 02 | 04 | 2014 PSL 01032 Abbots Langley Parish Council 02 | 04 | 2014 PSL 01033 Abbots Leigh Parish Council 02 | 04 | 2014 PSL 03449 Abbotskerswell Parish Council 23 | 04 | 2014 PSL 06255 Abbotts Ann Parish Council 06 | 07 | 2021 PSL 01034 Abdon & Heath Parish Council 02 | 04 | 2014 PSL 00040 Aberdeen City Council 03 | 04 | 2014 PSL 00029 Aberdeenshire Council 31 | 03 | 2014 PSL 01035 Aberford & District Parish Council 02 | 04 | 2014 PSL 01036 Abergele Town Council 17 | 10 | 2016 PSL 04909 Aberlemno Community Council 25 | 10 | 2016 PSL 04892 Abermule with llandyssil Community Council 11 | 10 | 2016 PSL 04315 Abertawe Bro Morgannwg University Health Board 24 | 02 | 2016 PSL 01037 Aberystwyth Town Council 17 | 10 | 2016 PSL 01038 Abingdon Town Council 17 | 10 | 2016 PSL 03548 Above Derwent Parish Council 20 | 03 | 2015 PSL 05197 Acaster Malbis Parish Council 23 | 10 | 2017 PSL 04423 Ackworth Parish Council 21 | 10 | 2015 PSL 01039 Acle Parish Council 02 | 04 | 2014 PSL 05515 Active Dorset 08 | 10 | 2018 PSL 05067 Active Essex 12 | 05 | 2017 PSL 05071 Active Lincolnshire 12 | 05 -

Integrated Medium Term Plan
1 CONTENTS Acronym Table 5 Message from the Chair and Chief Executive 8 Executive Summary 9 Part 1 Delivery of Our 2015/16 Plan 13 1.1 The New Clinical Response Model……………………………………............. 13 1.2 Quality and Operational Performance Trajectories…………………………... 15 1.3 2015/16 Strategic Change Portfolio …………………………………………… 18 1.4 Maturing Commissioning Arrangements and Increased Focus on Financial Strategy…………………………………………………………………………… 22 Part 2 Organisational and Strategic Context 24 This section, coupled with Part 1, serves as a high level diagnostic of the context within which we operate – it answers the “where are we now?” question. 2.1 Profile of the Trust……………………………………………………………….. 24 2.2 Our Demand & Activity………………………………………………………….. 32 2.3 The Five-Step Ambulance Care Pathway, Commissioning Quality & Delivery Framework, Understanding our Populations and Changes………. 33 2.4 National Policy Context………………………………………………………….. 37 2.5 Major Conditions, Older People and Frailty…………………………………… 42 2.6 Becoming a Listening and Learning Organisation………………………….... 43 2.7 NHS Wales Strategic Change Agenda………………………………………… 44 2.8 Service Change with Blue Light Partners……………………………………... 48 2.9 Ensuring Integration with Our Partners’ Three Year Plans………………….. 49 2.10 The Organisation and Prudent Healthcare……………………………………. 50 2.11 Treating People Fairly – Equality, Diversity & Human Rights………………. 51 2.12 Other Strategic Workforce and OD Drivers…………………………………… 54 Part 3 Creating Our Strategic Framework 57 This section sets the strategic framework for the organisation. It sets out our ambition and answers the “where do we want to go?” question. 3.1 Our Vision, Purpose and Behaviours………………………………………….. 57 3.2 Our Strategic Aims………………………………………………………………. 58 3.3 Our Priorities……………………………………………………………………… 59 3.4 Our Strategy Map………………………………………………………………… 63 3.5 Our Performance Ambitions………………………………………………........ -

{Department – Welsh}
Information Governance Team Vera Vallins Office Bronllys Hospital Bronllys Brecon Powys LD3 0LS Tel: 01874 712763 Fax: 01874 712756 Our ref: IG/FOI/19.R.233 23 September 2019 Sent via email to: [email protected] Dear Sir, Request under the Freedom of Information Act 2000 I write further to your request for information which was received on 29 August 2019 , to confirm, in accordance with S.1(1)(a) of the Freedom of Information Act 2000, that Powys Teaching Health Board (PTHB) holds part of the information that you require. For ease of reference your request is set out below and our response follows: Your Freedom of Information (FOI) Request: Who have you commissioned to provide any of the following orthotic devices which are vital to prevent damage and pain to the lower spine in long-term manual wheelchair users: 1. A measured spinal-restriction-brace, designed to stop long-term wheelchair users prevent stress induced damage and pain to their lumbar-sacrum region, where the spine joins the pelvis; 2. Power-assist motors such as: * Trike attachments * Pushers such as the Alber Smoov and Permobile Smart-drive * Joystick- and push-rim- controlled hub motors? 3. Please send me the minutes of the meetings discussing this essential support for wheelchair users, and a copy of the contract you commissioned. 4. If nothing has been commissioned, or if nothing has been considered for commissioning, what is the official protocol to get the consideration of such orthotic devices put onto the agenda? Is there a form members of the public can fill in? Pencadlys Headquarters Tŷ Glasbury, Ysbyty Bronllys, Glasbury House, Bronllys Hospital Aberhonddu, Powys LD3 0LU Brecon, Powys LD3 0LU Ffôn: 01874 711661 Tel: 01874 711661 Rydym yn croesawu gohebiaeth Gymraeg We welcome correspondence in Welsh Bwrdd Iechyd Addysgu Powys yw enw gweithredd Bwrdd Iechyd Lleol Powys Teaching Health Board is the operational name of Addysgu Powys Powys Teaching Local Health Board 5.