Severe Strongyloidiasis in Corticosteroid-Treated Patients: Case Series and Literature Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mantke, Peitz, Surgical Ultrasound -- Index
419 Index A esophageal 218 Anorchidism 376 gallbladder 165 Aorta 364–366 A-mode imaging 97 gastric 220 abdominal aneurysm (AAA) AAA (abdominal aortic aneurysm) metastasis 142 20–21, 364, 366 20–21, 364, 366 pancreatic 149, 225 dissection 364, 366 Abdominal wall Adenofibroma, breast 263 perforation 366 abscess 300–301 Adenoma pseudoaneurysm 364 diagnostic evaluation 297 adrenal 214 Aortic rupture 20 hematoma 73, 300, 305 colorectal 231, 232 Aplasia, muscular 272 rectus sheath 297–300 duodenal papilla 229, 231 Appendicitis 1–4 hernia 300, 302–304 gallbladder 165 consequences for surgical indications for sonography 297 hepatic 54, 58, 141 treatment 2 seroma 298, 300, 305 multiple 141 sonographic criteria 1 trauma 297–300 parathyroid 213 Archiving 418 Abortion, tubal 30 renal 241 Arteriosclerosis 346, 348 Abscess thyroid 202–203 carotid artery 335, 337, 338 abdominal wall 300–301 Adenomyomatosis 8, 164, 165 plaque 337, 338, 345, 367, 370 causes 301 Adrenal glands 214–216 Arteriovenous (AV) malformation amebic 138 adenoma 214 139, 293, 326–329 breast 264 carcinoma 214 Artery chest wall 173, 178 cyst 214 carotid 334–339 diverticular 120, 123 hematoma 214 aneurysm 338 drainage 85–88, 93 hemorrhage 214 arteriosclerosis 335 hepatic 6, 138, 398 hyperplasia 214 plaque characteristics inflammatory bowel disease limpoma/myelipoma 214 337, 338, 345 116, 119 metastases 214 bifurcation 334, 337 intramural 5 sonographic criteria 214 bulb 339 lung 183, 186, 190 tuberculosis 214 dissection 338, 339, 346 pancreatic 11 Advanced dynamic flow (ADF) sonographic -

Clinical Excellence Series Volume VI an Evidence-Based Approach to Infectious Disease
Clinical Excellence Series n Volume VI An Evidence-Based Approach To Infectious Disease Inside The Young Febrile Child: Evidence-Based Diagnostic And Therapeutic Strategies Pharyngitis In The ED: Diagnostic Challenges And Management Dilemmas HIV-Related Illnesses: The Challenge Of Emergency Department Management Antibiotics In The ED: How To Avoid The Common Mistake Of Treating Not Wisely, But Too Well Brought to you exclusively by the publisher of: An Evidence-Based Approach To Infectious Disease CEO: Robert Williford President & Publisher: Stephanie Ivy Associate Editor & CME Director: Jennifer Pai • Associate Editor: Dorothy Whisenhunt Director of Member Services: Liz Alvarez • Marketing & Customer Service Coordinator: Robin Williford Direct all questions to EB Medicine: 1-800-249-5770 • Fax: 1-770-500-1316 • Non-U.S. subscribers, call: 1-678-366-7933 EB Medicine • 5550 Triangle Pkwy Ste 150 • Norcross, GA 30092 E-mail: [email protected] • Web Site: www.ebmedicine.net The Emergency Medicine Practice Clinical Excellence Series, Volume Volume VI: An Evidence-Based Approach To Infectious Disease is published by EB Practice, LLC, d.b.a. EB Medicine, 5550 Triangle Pkwy Ste 150, Norcross, GA 30092. Opinions expressed are not necessarily those of this publication. Mention of products or services does not constitute endorsement. This publication is intended as a general guide and is intended to supplement, rather than substitute, professional judgment. It covers a highly technical and complex subject and should not be used for making specific medical decisions. The materials contained herein are not intended to establish policy, procedure, or standard of care. Emergency Medicine Practice, The Emergency Medicine Practice Clinical Excellence Series, and An Evidence-Based Approach To Infectious Disease are trademarks of EB Practice, LLC, d.b.a. -

Common Pediatric Pulmonary Issues
Common Pediatric Pulmonary Issues Chris Woleben MD, FAAP Associate Dean, Student Affairs VCU School of Medicine Assistant Professor, Emergency Medicine and Pediatrics Objectives • Learn common causes of upper and lower airway disease in the pediatric population • Learn basic management skills for common pediatric pulmonary problems Upper Airway Disease • Extrathoracic structures • Pharynx, larynx, trachea • Stridor • Externally audible sound produced by turbulent flow through narrowed airway • Signifies partial airway obstruction • May be acute or chronic Remember Physics? Poiseuille’s Law Acute Stridor • Febrile • Laryngotracheitis (croup) • Retropharyngeal abscess • Epiglottitis • Bacterial tracheitis • Afebrile • Foreign body • Caustic or thermal airway injury • Angioedema Croup - Epidemiology • Usually 6 to 36 months old • Males > Females (3:2) • Fall / Winter predilection • Common causes: • Parainfluenza • RSV • Adenovirus • Influenza Croup - Pathophysiology • Begins with URI symptoms and fever • Infection spreads from nasopharynx to larynx and trachea • Subglottic mucosal swelling and secretions lead to narrowed airway • Development of barky, “seal-like” cough with inspiratory stridor • Symptoms worse at night Croup - Management • Keep child as calm as possible, usually sitting in parent’s lap • Humidified saline via nebulizer • Steroids (Dexamethasone 0.6 mg/kg) • Oral and IM route both acceptable • Racemic Epinephrine • <10kg: 0.25 mg via nebulizer • >10kg: 0.5 mg via nebulizer Croup – Management • Must observe for 4 hours after -

Chronic Cough- Whoop It
3/3/2016 Chronic Cough- Whoop it Cassaundra Hefner PULMONARY ANATOMY DNP, FNP-BC FryeCare Lung Center Upper Airway Nasopharynx Oropharynx Laryngopharynx Lower Larynx Trachea Bronchi Bronchopulmonary segments Terminal bronchioles Acinus (alveolar regions) Upper and Lower Airway are lined with cilia which propel mucus and trapped bacteria toward the oropharynx Cough COUGH ACTION Protective reflex that keeps throat clear allowing for mucocilliary clearance of airway secretion Intrathoracic process of air from a vigorous cough through nearly closed vocal cords can approach 300mmHG, the velocities tear off mucus from the airway walls. The velocity can be up to 500mph 4 Cough/Sputum Defense mechanism to prevent aspiration- cough center stimulated- cough begins with deep inspiration to 50 % vital capacity- maximum expiratory flow increases coil - decreasing airway resistance- glottis opens wide and takes in large amount of air - glottis then rapidly closes - abdominal and intercostal muscles contract- increases intrapleural pressure - the glottis reopens- explosive release of air the tracheobronchial tree narrows rips the mucous off the walls = sputum 1 3/3/2016 Chronic Cough Defined (AACP, 2016) Effects of cough that prompts visit Talierco & Umur, 2014 Acute Sub-acute Chronic Fatigue 57% Cough Cough 3-8 Unexplained chronic less than weeks cough(UCC) Insomnia 45% 3 weeks Excessive perspiration 42% Cough lasting greater Incontinence 39% than 8 weeks in 15 yo or older MSK pain 45% Cough lasting greater Inguinal herniation than 4 weeks in Dysrhythmias those under the Headaches age of 15 Quality of life questionnaires are recommended for adolescents and children (CQLQ) Work loss Data Institute (NCG) (2016) Cough Referral to Pulmonology 80%-90% chronic cough Most common symptom for PCP visits in the U.S. -

Retropharyngeal Abscess: Diagnosis and Treatment Update
Infectious Disorders – Drug Targets, 2012, 12, 291-296 291 Retropharyngeal Abscess: Diagnosis and Treatment Update 1 2,3 Brian K. Reilly * and James S. Reilly 1Children’s National Medical Center, Washington, DC; USA; 2Chair, Department of Surgery, Nemours/Alfred I. duPont Hospital for Children, Wilmington, DE, USA; 3Professor of Otolaryngology and Pediatrics, Thomas Jefferson Univer- sity, Philadelphia, PA, USA Abstract: Retropharyngeal abscess is a deep neck space infection that may present in various subtle ways permitting po- tentially lethal complications to occur before appropriate diagnosis is made and expedient management undertaken. This article reviews in detail the pertinent anatomy, diagnostic pearls, and clinical recommendations to optimally manage these common infections in children. Keywords: Abscess, imaging, infection, neck, pediatric, retropharyngeal. OVERVIEW whether purulence is obtained intra-operatively [3]. Classic findings for abscess include large fluid with central A retropharyngeal abscess (RPA) is a deep neck space hypodensity, complete ring enhancement, and scalloping infection defined by its anatomical location within the deep Fig. (1). cervical tissue planes. RPA is located behind the pharyngeal mucosa and is contained anteriorly by the buccopharyngeal fascia (around the constrictor muscles) and laterally by the carotid sheath/parapharyngeal space. Superiorly, it may ex- tend to the skull base, and inferiorly, it can travel to the me- diastinum. This “potential” retropharyngeal space, which expands with infection, is occupied by a lymph-node basin [1] that serves as the common, final drainage pathway of the nasal cavity, paranasal sinuses, nasopharynx, oropharynx, hypopharynx, and larynx. Inadequately treated and virulent infections of these regions can cause suppuration of these nodes. Thus, retropharyngeal lymphadenitis with edema can progress to a cellulitis, which, if untreated, evolves to early abscess or phlegmon and then to abscess. -

Chest Pain and Cardiac Dysrhythmias
Chest Pain and Cardiac Dysrhythmias Questions 1. A 59-year-old man presents to the emergency department (ED) com- plaining of new onset chest pain that radiates to his left arm. He has a his- tory of hypertension, hypercholesterolemia, and a 20-pack-year smoking history. His electrocardiogram (ECG) is remarkable for T-wave inversions in the lateral leads. Which of the following is the most appropriate next step in management? a. Give the patient two nitroglycerin tablets sublingually and observe if his chest pain resolves. b. Place the patient on a cardiac monitor, administer oxygen, and give aspirin. c. Call the cardiac catheterization laboratory for immediate percutaneous inter- vention (PCI). d. Order a chest x-ray; administer aspirin, clopidogrel, and heparin. e. Start a β-blocker immediately. 2. A 36-year-old woman presents to the ED with sudden onset of left- sided chest pain and mild shortness of breath that began the night before. She was able to fall asleep without difficulty but woke up in the morning with persistent pain that is worsened upon taking a deep breath. She walked up the stairs at home and became very short of breath, which made her come to the ED. Two weeks ago, she took a 7-hour flight from Europe and since then has left-sided calf pain and swelling. What is the most com- mon ECG finding for this patient’s presentation? a. S1Q3T3 pattern b. Atrial fibrillation c. Right-axis deviation d. Right-atrial enlargement e. Tachycardia or nonspecific ST-T–wave changes 1 2 Emergency Medicine 3. -

Don't Overlook Unexpected, but Risky, Diagnoses
® NOVEMBER 2020 VOLUME 15, NUMBER 2 THE JOURNAL OF URGENT CARE MEDICINE ® www.jucm.com The Official Publication of the UCA and CUCM CLINICAL cme ALSO IN THIS ISSUE 19 Original Research Probably Strep Informed Decisions Are Safer ‘ ’ Is Decisions in Patients with Sinusitis cme 29 Case Report Potentially Dangerous— When a Disease ‘of Childhood’ Threatens the Life of an Adult Patient 35 Clinical Don’t Overlook Unexpected, Better to Risk Patient Outrage Than Antibiotic Resistance When Treating but Risky, Diagnoses Otitis Media cme Health Law and Compliance The COVID-19 Vaccine Could Save Lives—and Your Business. But What If Employees Refuse to Get It? Ad_FullPage_Sized.indd 1 10/21/20 3:13 PM URGENT PERSPECTIVES Finding Urgent Care (and the Value of Recognizing a Specialty) n GUY MELROSE, MB, ChB arrived in New Zealand 11 years ago, a doctor without direc- Ition and certainly with no inkling of urgent care. I was one of those doctors who had always hoped to find their ultimate career path whilst at university. Alas, whilst I was able to remove some options (here’s looking at you Ob/Gyn),no single spe- cialty sufficiently inspired me to follow that rabbit hole through to its conclusion. So, my medical career began with an eclectic mix of jobs and travel, mainly focused around the emergency department. Maintaining this level of generalism seemed sensible, until such time as a specialty found me. As a young person, the ED was an exciting and flexible option. Yet in the back of my mind, I always assumed the career that would suit my broad interest in medicine whilst also addressing my growing need for a work-life balance would be general practice (or family practice, as it’s known in the U.S.). -

Andrea Kline Tilford Phd, CPNP‐AC/PC, FCCM
Acute Care Pediatric Nurse Practitioner Review Course 2020 Andrea Kline Tilford PhD, CPNP‐AC/PC, FCCM C.S. Mott Children’s Hospital Ann Arbor, Michigan ©202 0 Disclosures • I have no financial relationships to disclose • I will not discuss investigational drug use ©202 0 Objectives • Discuss general principles of pediatric respiratory physiology • Discuss the presentation and evaluation of common pediatric respiratory diseases • Identify appropriate management strategies for common pediatric respiratory diseases ©202 0 Basic Anatomy • Upper Airway • Supraglottic (nose, nasopharynx, epiglottis) • Glottis (vocal cords, subglottic area, cervical trachea) • Humidifies inhaled gases • Warms inhaled gas • Site of most resistance to airflow • Conducting airways (dead space) • Lower airways • Thoracic trachea, bronchi, bronchioles and alveoli (gas exchange) ©202 0 Anatomical Considerations in Children • Pediatrics • Small mouth • Large tongue • In relation to mandible • Floppy epiglottis (infants) • Large occiput • Infants are obligate nose breathers (until ~ 6 months of age) • Cricoid ring narrowest portion of airway in infants and young children ©202 0 Bronchus • Bifurcates into right and left bronchus • RIGHT side generally more straight and more likely to be site of aspiration www.med.umich.edu ©202 0 Alveoli • Continue to multiply until ~ 8 years of age Covered in capillaries Site of gas exchange oac.med.jhmi.edu ©202 0 Basic Physiology • Goal of respiration = Oxygen in and carbon dioxide out • Oxygen ʻinʼ • For cell use • Carbon dioxide ʻoutʼ • Produced by cells ©202 0 Gas Exchange • Inhalation • Active; requires contraction of several muscles (e.g. diaphragm, intercostals) • Exhalation • Passive • Relaxation of intercostals and diaphragm, return of rib cage, diaphragm, and sternum to resting position, increases pressure in lungs and air is exhaled **PEARL: Some conditions, such as status asthmaticus, interfere with passive exhalation. -

Mehlmanmedical Hy Pulmonary
MEHLMANMEDICAL HY PULMONARY MEHLMANMEDICAL.COM HY Pulmonary - 58F + 6-month Hx of shortness of breath and non-productive cough + 2-year Hx of worsening dysphagia + 20-yr Hx of hands turning white when exposed to cold; what lung condition is this patient most at risk of developing? à answer = pulmonary hypertension à pulmonary fibrosis common in CREST syndrome (scleroderma; limited systemic sclerosis) à pulmonary fibrosis seen in both diffuse and limited types of systemic sclerosis; the latter is sans the renal phenomena) à can lead to cor pulmonale, which is right-heart failure secondary to a pathology of lung etiology (i.e., the left heart must not be causative). - What will the USMLE frequently say in the Q if they’re hinting at pulmonary hypertension? à HY vignette descriptors are loud S2 or P2 (pulmonic valve slams shut when the distal pressure is high); dilation of proximal pulmonary arteries; increased pulmonary vascular markings (congestion + increased hydrostatic pressure). - When is “pulmonary hypertension” important as the answer? à notably in Eisenmenger syndrome and cor pulmonale. o Regarding Eisenmenger: the reversal of the L to R shunt across the VSD such that it’s R to L requires the tunica media of the pulmonary arterioles to hypertrophy secondary to chronic increased preload à proximal backup of hydrostatic pressure à increased afterload on the right heart à now the right heart starts to significantly hypertrophy à shunt across the VSD reverses R to L. This is important, as RVH is not the most upstream cause of Eisenmenger; the pulmonary hypertension is. o Regarding cor pulmonale: as mentioned above, cor pulmonale is right heart failure secondary to a pathology of pulmonary etiology (e.g., COPD, cystic fibrosis [CF], fibrosis, etc.); however it must be noted that the most common cause of right heart failure is left heart failure; so for cor pulmonale to be the diagnosis, the left heart must not be the etiology of the right heart failure; the lungs must be the etiology. -

2019 In-Service Review: Visual Stimuli
1/11/2019 1. A CDC laboratory worker presents with malaise, fever, and a painless arm lesion. What is the most appropriate treatment? 2019 In-service Review: A. Doxycycline Visual Stimuli B. Cephalexin C. Penicillin Brett R. Todd, MD, FACEP D. Surgical debridement Assistant Professor of Emergency Medicine E. Dapsone Oakland University William Beaumont School of Medicine 1 2 1 2 A. Doxycycline Anthrax • Bacillus anthracis • Inhalational – initial flu-like, later severe distress, mediastinitis, wide mediastinum on CXR • Cutaneous – painless vesicle then ulcer with black eschar • GI • Bioterrorism agent 3 4 3 4 2. A 26 y.o. homeless man presents to the ED complaining of fever, foul breath, and oral pain. What is the diagnosis? A. Dental caries B. Acute necrotizing ulcerative gingivitis C. Ludwig’s angina D. Periapical abscess E. Malingering 5 6 5 6 1 1/11/2019 3. A 24 y.o. man is thrown from his B. Acute Necrotizing Ulcerative Gingivitis motorcycle at high speed. He is hypertensive • Trench mouth on arrival. What is the most appropriate • Immunosuppressed, HIV, treatment based on the portable chest x-ray Etoh, Stress • Fever, pain, bleeding, halitosis shown? • Grayish pseudomembrane • Polymicrobial, Fusobacterium, A. Needle thoracostomy Treponema B. Pericardiocentesis • PCN + Flagyl, or Clinda, or C. ED Thoracotomy Augmentin • Chlorhexidine rinses D. Esmolol E. Tube thoracostomy 7 8 7 8 D. Esmolol Traumatic rupture of aorta • Wide mediastinum, enlarged aortic knob, tracheal deviation, apical cap • Treat like aortic dissection – Beta-blocker, vasodialators • Goal: HR < 60 - 80, SBP < 120 • Medical management for intimal tear • Surgery for intramural hematoma, pseudoaneurysm, or free rupture 9 10 9 10 4. -

Chapter 1 Traumatic and Nontraumatic Emergencies of the Brain, Head, and Neck Glenn D
Chapter 1 Traumatic and Nontraumatic Emergencies of the Brain, Head, and Neck Glenn D. Barest, Asim Z. Mian, Rohini N. Nadgir, and Osamu Sakai Imagine you are asked to create a list of the disorders of to study the other volumes in the Requisites series (es- the brain, head, and neck that one might commonly expect pecially Neuroradiology, Musculoskeletal Imaging, and to encounter at an emergency department (ED) and de- Pediatric Radiology), which cover this material in great scribe the typical imaging features. At first, this challenge detail. In this attempt at condensing so much material seems straightforward enough. However, upon beginning into one useful volume, important topics inevitably have the task, it soon becomes clear that almost every disorder been neglected. We hope that this volume can serve as within the realm of neuroradiology/head and neck radi- a starting point for further study and become a valuable ology might at one time or another present as an acute reference to on-call radiologists, emergency department emergency. Inclusion of certain diagnoses such as stroke, physicians, and residents of both specialties. fractures, and epiglottitis is a must. Other diagnoses, such as oligodendroglioma or perhaps a slowly growing le- INTRACRANIAL HEMORRHAGE AND sion, might seem less clear-cut. Ultimately, it is important TRAUMATIC BRAIN INJURY to realize that a wide variety of processes will result in an alteration in mental status leading to an ED visit, with Whether in the setting of head trauma, spontaneous de- imaging playing a key role in diagnosis and appropriate velopment of headache, or alteration of mental status, the management. -
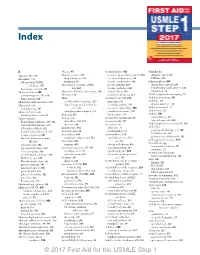
First-Aid-Step-1-2017-Index.Pdf
Index A Abscess, 451 Acetaminophen, 455 Achlorhydria Abacavir, 197, 199 Absence seizures, 487 vs aspirin for pediatric patients, 455 stomach cancer, 362 Abciximab, 118 drug therapy for, 514 free radical injury and, 210 VIPomas, 356 Glycoprotein IIb/IIIa treatment, 661 hepatic necrosis from, 240 Achondroplasia, 435 inhibitors, 415 Absolute risk reduction (ARR), for osteoarthritis, 439 chromosome disorder, 60 thrombogenesis and, 393 248, 669 tension headaches, 488 endochondral ossification in, 434 Abdominal aorta, 348 Absorption disorders and anemia, 396 toxicity effects, 455 inheritance, 56 217 atherosclerosis in, 292, 668 AB toxin, 128 toxicity treatment for, 239 AChR (acetylcholine receptor), 561 bifurcation of, 629 Abuse Acetazolamide, 243, 575 Acid-base physiology, Acidemia, 561 Abdominal aortic aneurysm, 292 confidentiality exceptions, 255 glaucoma, 521 diuretic effect on, 576 Abdominal colic dependent personality disorder metabolic acidosis, 561 Acidic amino acids, 77 lead poisoning, 397 and, 535 in nephron physiology, 555 Acid maltase, 82 Abdominal distension intimate partner violence, 257 pseudotumor cerebri, 491 Acidosis, 561 duodenal atresia and, 344 Acalculia, 481 site of action, 574 contractility in, 273 Abdominal pain Acamprosate Acetoacetate metabolism, 86 hyperkalemia with, 560 Budd-Chiari syndrome, 375, 652 alcoholism, 541, 661 Acetone breath, 337 Acid phosphatase in neutrophils, 386 cilostazol/dipyridamole, 415 diarrhea, 240 Acetylation, 41 Acid reflux Clostridium difficile, 652 Acanthocytes, 394 chromatin, 32 esophageal