Download the Hemophilia Dictionary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pictures of Central Venous Catheters
Pictures of Central Venous Catheters Below are examples of central venous catheters. This is not an all inclusive list of either type of catheter or type of access device. Tunneled Central Venous Catheters. Tunneled catheters are passed under the skin to a separate exit point. This helps stabilize them making them useful for long term therapy. They can have one or more lumens. Power Hickman® Multi-lumen Hickman® or Groshong® Tunneled Central Broviac® Long-Term Tunneled Central Venous Catheter Dialysis Catheters Venous Catheter © 2013 C. R. Bard, Inc. Used with permission. Bard, are trademarks and/or registered trademarks of C. R. Bard, Inc. Implanted Ports. Inplanted ports are also tunneled under the skin. The port itself is placed under the skin and accessed as needed. When not accessed, they only need an occasional flush but otherwise do not require care. They can be multilumen as well. They are also useful for long term therapy. ` Single lumen PowerPort® Vue Implantable Port Titanium Dome Port Dual lumen SlimPort® Dual-lumen RosenblattTM Implantable Port © 2013 C. R. Bard, Inc. Used with permission. Bard, are trademarks and/or registered trademarks of C. R. Bard, Inc. Non-tunneled Central Venous Catheters. Non-tunneled catheters are used for short term therapy and in emergent situations. MAHURKARTM Elite Dialysis Catheter Image provided courtesy of Covidien. MAHURKAR is a trademark of Sakharam D. Mahurkar, MD. © Covidien. All rights reserved. Peripherally Inserted Central Catheters. A “PICC” is inserted in a large peripheral vein, such as the cephalic or basilic vein, and then advanced until the tip rests in the distal superior vena cava or cavoatrial junction. -
Piccs, Ports and Lines: Clarifying the Options
Current Concepts in Vascular Therapies 2011 Mid-Atlantic Conference PICCs, Ports and Lines: Clarifying the Options Babatunde Almaroof, MD April 2, 2011 Objectives • State the indications for central venous access • Discuss types of central venous catheters • “Clarifying the options”/indications for each kind of catheter. Need for central vascular access • There is an increasing need for vascular access as medical care has become more complex. • Most inpatients are able to get their needs served by a peripheral i.v access • Sometimes however, a central access will be needed due to limitations of a peripheral access – Infiltration, extravasation, thrombosis – Infection and sclerosis • This makes central venous access, the preferred choice for long term use as they allow a higher flow and tolerate hyperosmolar solutions not tolerated by peripheral veins Indications for central venous access • TPN • Chemotherapy • Long term antibiotics – Osteomyelitis, endocarditis, fungal infections • Patients with difficult peripheral vein access • Hemodynamic monitoring • Temporary hemodialysis access • Plasmapheresis Historical Background • The first i.v infusion was performed using a cannula made from quill in 1657 • First successful human blood transfusion was performed in 1667 • Seldinger described his technique for catheter insertion in 1953 • Percutaneous placement of a subclavian vein catheter was reported in 1956 Sites of central venous access • Internal Jugular vein • Subclavian vein – Higher risk of pneumothorax • Femoral vein – Higher risk of -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

Infusaport Insertion in Patients with Haemophilia
Infusaport insertion in patients with haemophilia PURPOSE This guideline is designed to assist medical and nursing staff in the management of children with haemophilia having an infusaport inserted at the Royal Children’s Hospital. DEFINITIONS Infusaport or portacath is an implantable Central Venous Access Device. BACKGROUND Most children with severe haemophilia (<1% Factor VIII or IX) will require prophylactic intravenous clotting factor administration 2-3 times per week to prevent spontaneous bleeding. Accessing peripheral veins can be difficult and traumatic for children and in particular infants/toddlers where veins are often difficult to identify. A number of boys develop significant behavioural issues around treatment after traumatic experiences in their early years. Approximately 80% of children with severe haemophilia treated at the Royal Children’s Hospital will require an infusaport for venous access. Most families report that insertion of a “port” dramatically improves their quality of life in that venous access is no longer fearful and difficult and parents are able to administer clotting factor to their child at home for both prevention and treatment of bleeds. Ports are removed as soon as parents are able to administer clotting factor peripherally. In general ports are removed prior to commencement of primary school. PROCEDURE Once the need for a port has been identified and discussed with the family a referral is made. Mr Joe Crameri performs the majority of infusaport surgery in haemophilia patients at the Royal Children’s Hospital. Many families appreciate the opportunity to see a port (there is one in the haemophilia centre) and to speak with a family whose child is established on home prophylaxis via a port. -
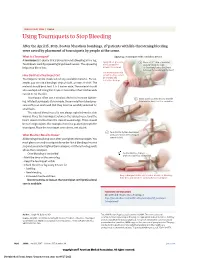
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -

Venous Access and Ports
Venous Access and Ports Helen Starosta Venous access and ports Peripheral IV access Arterio-Venous Fistula Central venous access Peripherally Inserted Central Catheter (PICC) Non Tunnelled Central Venous Catheter (CVC) Tunnelled (e.g. Hickman) Central Venous Access Device Implanted Central Venous Access Device e.g. Infusaport Jesse’s Story Charles’s Story Vein Training Why do we need venous access Treatment for bleeding disorders involves intravenous therapy Therefore reliable venous access is essential to make effective treatment possible The choices for IV access Peripheral IV access Arterio-Venous Fistula Central venous access Peripherally Inserted Central Catheter (PICC) Non Tunnelled Central Venous Catheter (CVC) Tunnelled (e.g. Hickman) Central Venous Access Device Implanted Central Venous Access Device e.g. Infusaport Peripheral Venous Access Butterfly & IV Short term (days) or intermittent therapy Short catheters generally placed in forearm, hand or scalp veins Arterio-Venous Fistula Can last many years Connects an artery directly to a vein → results in more blood flow to the vein → the vein grows larger and stronger Fistula takes a while after surgery to develop (as long as 24 months) Properly formed fistula is less likely than other kinds of vascular access to form clots or become infected Peripherally Inserted Central Catheters (PICC) Short term use (days to several weeks) Peripheral central venous catheter inserted at or above the antecubital space and the distal tip of the catheter is positioned -
ER Guide to Bleeding Disorders
Bleeding disorders ER guide to bleeding disorders 1 Table of contents 4 General Guidelines 4–5 national Hemophilia Foundation guidelines 5–10 Treatment options 10 HemopHilia a Name:__________________________________________________________________________________________________ 10–11 national Hemophilia Foundation guidelines Address:________________________________________________________________________________________________ 12 dosage chart Phone:__________________________________________________________________________________________________ 14–15 Treatment products 16 HemopHilia B In case of emergency, contact: ______________________________________________________________________________ 16 national Hemophilia Foundation guidelines Relation to patient:________________________________________________________________________________________ 17 dosage chart 18 Treatment products 19 HemopHilia a or B with inHiBiTors Diagnosis: Hemophilia A: Mild Moderate Severe 20 national Hemophilia Foundation guidelines Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 21 Treatment products Hemophilia B: Mild Moderate Severe 22–23 Von willeBrand disease Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 23–24 national Hemophilia Foundation guidelines von Willebrand disease: Type 1 Type 2 Type 3 Platelet type 25 Treatment products 27 Bibliography Preferred product:_________________________________________________________________________________________ Dose for life-threatening -
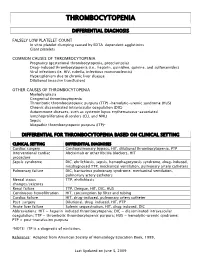
Thrombocytopenia.Pdf
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

Central Venous Lines in Haemophilia. Ljung, Rolf
Central venous lines in haemophilia. Ljung, Rolf Published in: Haemophilia DOI: 10.1046/j.1365-2516.9.s1.7.x 2003 Link to publication Citation for published version (APA): Ljung, R. (2003). Central venous lines in haemophilia. Haemophilia, 9(Suppl 1), 88-92. https://doi.org/10.1046/j.1365-2516.9.s1.7.x Total number of authors: 1 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. LUND UNIVERSITY PO Box 117 221 00 Lund +46 46-222 00 00 Haemophilia (2003), 9, (Suppl. 1), 88–93 Central venous lines in haemophilia R. LJUNG Departments of Paediatrics and Coagulation Disorders, Lund University, University Hospital, Malmoo,€ Sweden Summary. Infections and technical problems are the been seen in some but not in others. -

Ten Patient Stories Illustrating the Extraordinarily Diverse Clinical Features of Patients with Thrombotic Thrombocytopenic Purpura and Severe ADAMTS13 Deficiency
Journal of Clinical Apheresis 27:302–311 (2012) Ten Patient Stories Illustrating the Extraordinarily Diverse Clinical Features of Patients With Thrombotic Thrombocytopenic Purpura and Severe ADAMTS13 Deficiency James N. George,* Qiaofang Chen, Cassie C. Deford, and Zayd Al-Nouri Department of Biostatistics and Epidemiology, College of Public Health, Department of Medicine, College of Medicine, The University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma Patients with thrombotic thrombocytopenic purpura (TTP) and severe ADAMTS13 deficiency are often consid- ered to have typical clinical features. However, our experience is that there is extraordinary diversity of the pre- senting features and the clinical courses of these patients. This diversity is illustrated by descriptions of 10 patients. The patients illustrate that ADAMTS13 activity may be normal initially but severely deficient in subse- quent episodes. Patients with established diagnoses of systemic infection as the cause of their clinical features may have undetectable ADAMTS13 activity. Patients may have a prolonged prodrome of mild symptoms with only microangiopathic hemolytic anemia and thrombocytopenia or they may have the sudden onset of critical ill- ness with multiple organ involvement. Patients may die rapidly or recover rapidly; they may require minimal treatment or extensive and prolonged treatment. Patients may have acute and severe neurologic abnormalities before microangiopathic hemolytic anemia and thrombocytopenia occur. Patients may have concurrent TTP and systemic lupus erythematosus. Patients may have hereditary ADAMTS13 deficiency as the etiology of their TTP rather than acquired autoimmune ADAMTS13 deficiency. These patients’ stories illustrate the clinical spectrum of TTP with ADAMTS13 deficiency and emphasize the difficulties of clinical diagnosis. J. Clin. -

Modern Management of Traumatic Hemothorax
rauma & f T T o re l a t a m n r e u n o t J Mahoozi, et al., J Trauma Treat 2016, 5:3 Journal of Trauma & Treatment DOI: 10.4172/2167-1222.1000326 ISSN: 2167-1222 Review Article Open Access Modern Management of Traumatic Hemothorax Hamid Reza Mahoozi, Jan Volmerig and Erich Hecker* Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany *Corresponding author: Erich Hecker, Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany, Tel: 0232349892212; Fax: 0232349892229; E-mail: [email protected] Rec date: Jun 28, 2016; Acc date: Aug 17, 2016; Pub date: Aug 19, 2016 Copyright: © 2016 Mahoozi HR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Hemothorax is defined as a bleeding into pleural cavity. Hemothorax is a frequent manifestation of blunt chest trauma. Some authors suggested a hematocrit value more than 50% for differentiation of a hemothorax from a sanguineous pleural effusion. Hemothorax is also often associated with penetrating chest injury or chest wall blunt chest wall trauma with skeletal injury. Much less common, it may be related to pleural diseases, induced iatrogenic or develop spontaneously. In the vast majority of blunt and penetrating trauma cases, hemothoraces can be managed by relatively simple means in the course of care. Keywords: Traumatic hemothorax; Internal chest wall; Cardiac Hemodynamic response injury; Clinical manifestation; Blunt chest-wall injuries; Blunt As above mentioned the hemodynamic response is a multifactorial intrathoracic injuries; Penetrating thoracic trauma response and depends on severity of hemothorax according to its classification.