What Everyone Should Know to Stop Bleeding After an Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

First Aid 10/18/07 1:23 PM Page 1
FINAL CATALOGUE -First Aid 10/18/07 1:23 PM Page 1 Regulation FirstFirst Aid Aid Kits by SAFECROSS OCCUPATIONAL HEALTH AND SAFETY REGULATION FIRST AID KITS Regulation first aid kits meet regulations required by Federal, Provincial and Territorial jurisdictions. Regulations change on a continuing basis. Requirements vary from jurisdiction to jurisdiction and are ALBERTA FIRST AID KITS dependent on a number of factors including (but not limited to): • maximum number of employees at the work site (or per shift) http://www.gov.ab.ca/ • location of the place of employment/industry • type of industry and potential hazards • proximity or travel time to a medical facility FEDERAL REGULATION FIRST AID KITS Common federal employers include the following interprovincial and international industries: • Banks • Railways, highway and air transport No. 1 • Ferries, tunnels, bridges and canals FAP 50100 16 unit Plastic with gasket • Telephone and telegraph systems FAP 50103 16 unit Metal • Pipelines FAP 50109B Soft Pack # 16 • Radio and television broadcasting and cable systems • Shipping and shipping services No. 2 • Employment in the operation of ships, trains and aircraft FAP 50124 36 unit Plastic with gasket • Licensed grain elevators, and certain feed mills and feed warehouses, flour mills and grain seed clearing plants FAP 50127 36 unit Metal • Federal public service and persons employed by the public service and Crown corporations and agencies FAP 50133B Soft Pack # 24 • Indian reserves • Exploration and development of petroleum on lands subject to federal jurisdiction No. 3 FAP 50140 # 2 Plastic with gasket FAP 50139 # 2 Metal FAP 50142B Soft Pack Mini Trauma Bag FEDERAL FIRST AID KITS BRITISH COLUMBIA FIRST AID KITS Item required but not included in all kits: accident record book. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Gunshot Wounds
Gunshot Wounds Michael Sirkin, MD Chief, Orthopaedic Trauma Service Assistant Professor, New Jersey Medical School North Jersey Orthopaedic Institute Created March 2004; Reviewed March 2006, August 2010 Ballistics • Most bullets made of lead alloy – High specific gravity • Maximal mass • Less effect of air resistance • Bullet tips – Pointed – Round – Flat – Hollow Ballistics • Low velocity bullets – Made of low melting point lead alloys – If fired from high velocity they melt, 2° to friction • Deform • Change missile ballistics • High velocity bullets – Coated or jacketed with a harder metal – High temperature coating – Less deformity when fired Velocity • Energy = ½ mv2 • Energy increases by the square of the velocity and linearly with the mass • Velocity of missile is the most important factor determining amount of energy and subsequent tissue damage Kinetic Energy of High and Low Velocity Firearms Kinetic Energy of Shotgun Shells Wounding power • Low velocity, less severe – Less than 1000 ft/sec – Less than 230 grams • High velocity, very destructive – Greater than 2000 ft/sec – Weight less than 150 grams • Shotguns, very destructive at close range – About 1200 ft/sec – Weight up to 870 grams Factors that cause tissue damage • Crush and laceration • Secondary missiles • Cavitation • Shock wave Crush and Laceration • Principle mechanism in low velocity gunshot wounds • Material in path is crushed or lacerated • The kinetic energy is dissipated • Increased tissue damage with yaw or tumble – Increased profile – Increased rate of kinetic -

First Aid Cpr Aed
FIRST AID CPR AED Copyright: Bushue HR, Inc. 2018 First Aid Copyright: Bushue HR, Inc. 2018 Outline First Aid First Aid Situations First Aid Kit Training Copyright: Bushue HR, Inc. 2018 First Aid Facts More than 1.25 million Americans have a first or recurrent heart attack every year. 70% of the deaths from heart attack occur before the victim reaches the hospital. rd Stroke is the 3 leading cause of death in the U.S. There are 800,000 strokes each year in the United States. The human body contains an average of 10 pints of blood. Loss of two pints may result in shock, loss of five to six pints usually results in death. Shock is a life-threatening condition that occurs when the body’s organs and tissues do not receive enough oxygenated blood. The most common cause of shock is severe bleeding. There are 700,000 work-related eye injuries each year in the United States, 90% of which are preventable with proper safety eyewear. There are about 4,500 fire and burn deaths per year, roughly 20,000 more are injured from fires and burns. 1,500 people die from excessive heat each year in the U.S. Heat related emergencies are usually preventable. Copyright: Bushue HR, Inc. 2018 First Aid First aid is emergency care that is provided for injury or sudden illness before emergency medical treatment is available. A workplace first aid provider is: Trained in the delivery of initial medical emergency procedures. Expected to use a limited amount of equipment to perform a primary assessment. -

Equiping the Right Boat First Aid
Building a First Aid Kit for your Boat By Jeannie Zortman, LPSC GMM Presentation 2018 Have you ever wondered what you would do if you had a serious injury or medical condition where you couldn’t call 911? Are you prepared to handle a major incident on board your boat? Have you done everything possible to prevent any such unfortunate foreseeable event? Building a personalized first aid kit for your boat is something you can do this month and should be checked each season before heading out to the lake. Bandages get wet or dry out. Medicines expire, tools get robbed for mechanical issues, etc, etc. Building your own kit has many advantages. First, by building it yourself, you know what is there, and hopefully have put it in a place you will remember and can access easily when you need it. Secondly, you will have the tools and materials needed for the types of illnesses and injuries you are most likely to have to handle yourself on your boat with its unique capabilities. Remember! Treatment is exponentially more painful, more expensive, risky, and resource intensive than prevention, preparation, and training. So let’s get started! Let’s start with prevention! Take a CPR/first aid class! Wear your life jacket! Get adequate sleep! Hydrate! Bring cold, wind, and sun protection, and plan nutritious snacks (limes) Check the weather! Be prepared for the worst conditions for your area. Get to know your crew! Tell them if you have any special conditions. Exchange emergency contact information. Don’t assume! Bring a light source! And ONE MORE TIME! Make a commitment to signing up for a First Aid/CPR class, Wilderness First Responder Course, or a Safety at Sea Course. -

Pressure Ulcer Staging Cards and Skin Inspection Opportunities.Indd
Pressure Ulcer Staging Pressure Ulcer Staging Suspected Deep Tissue Injury (sDTI): Purple or maroon localized area of discolored Suspected Deep Tissue Injury (sDTI): Purple or maroon localized area of discolored intact skin or blood-fi lled blister due to damage of underlying soft tissue from pressure intact skin or blood-fi lled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, fi rm, mushy, boggy, and/or shear. The area may be preceded by tissue that is painful, fi rm, mushy, boggy, warmer or cooler as compared to adjacent tissue. warmer or cooler as compared to adjacent tissue. Stage 1: Intact skin with non- Stage 1: Intact skin with non- blanchable redness of a localized blanchable redness of a localized area usually over a bony prominence. area usually over a bony prominence. Darkly pigmented skin may not have Darkly pigmented skin may not have visible blanching; its color may differ visible blanching; its color may differ from surrounding area. from surrounding area. Stage 2: Partial thickness loss of Stage 2: Partial thickness loss of dermis presenting as a shallow open dermis presenting as a shallow open ulcer with a red pink wound bed, ulcer with a red pink wound bed, without slough. May also present as without slough. May also present as an intact or open/ruptured serum- an intact or open/ruptured serum- fi lled blister. fi lled blister. Stage 3: Full thickness tissue loss. Stage 3: Full thickness tissue loss. Subcutaneous fat may be visible but Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. -

Penetrating Injury to the Head: Case Reviews K Regunath, S Awang*, S B Siti, M R Premananda, W M Tan, R H Haron**
CASE REPORT Penetrating Injury to the Head: Case Reviews K Regunath, S Awang*, S B Siti, M R Premananda, W M Tan, R H Haron** *Department of Neurosciences, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan, **Department of Neurosurgery, Hospital Kuala Lumpur the right frontal lobe to a depth of approximately 2.5cm. SUMMARY (Figure 1: A & B) There was no obvious intracranial Penetrating injury to the head is considered a form of severe haemorrhage along the track of injury. The patient was taken traumatic brain injury. Although uncommon, most to the operating theatre and was put under general neurosurgical centres would have experienced treating anaesthesia. The nail was cut proximal to the entry wound patients with such an injury. Despite the presence of well and the piece of wood removed. The entry wound was found written guidelines for managing these cases, surgical to be contaminated with hair and debris. The nail was also treatment requires an individualized approach tailored to rusty. A bicoronal skin incision was fashioned centred on the the situation at hand. We describe a collection of three cases entry wound. A bifrontal craniotomy was fashioned and the of non-missile penetrating head injury which were managed bone flap removed sparing a small island of bone around the in two main Neurosurgical centres within Malaysia and the nail (Figure 1: C&D). Bilateral “U” shaped dural incisions unique management approaches for each of these cases. were made with the base to the midline. The nail was found to have penetrated with dura about 0.5cm from the edge of KEY WORDS: Penetrating head injury, nail related injury, atypical penetrating the sagittal sinus. -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -
Wound Care: the Basics
Wound Care: The Basics Suzann Williams-Rosenthal, RN, MSN, WOC, GNP Norma Branham, RN, MSN, WOC, GNP University of Virginia May, 2010 What Type of Wound is it? How long has it been there? Acute-generally heal in a couple weeks, but can become chronic: Surgical Trauma Chronic -do not heal by normal repair process-takes weeks to months: Vascular-venous stasis, arterial ulcers Pressure ulcers Diabetic foot ulcers (neuropathic) Chronic Wounds Pressure Ulcer Staging Where is it? Where is it located? Use anatomical location-heel, ankle, sacrum, coccyx, etc. Measurements-in centimeters Length X Width X Depth • Length = greatest length (head to toe) • Width = greatest width (side to side) • Depth = measure by marking the depth with a Q- Tip and then hold to a ruler Wound Characteristics: Describe by percentage of each type of tissue: Granulation tissue: • red, cobblestone appearance (healing, filling in) Necrotic: • Slough-yellow, tan dead tissue (devitalized) • Eschar-black/brown necrotic tissue, can be hard or soft Evaluating additional tissue damage: Undermining Separation of tissue from the surface under the edge of the wound • Describe by clock face with patients head at 12 (“undermining is 1 cm from 12 to 4 o’clock”) Tunneling Channel that runs from the wound edge through to other tissue • “tunneling at 9 o’clock, measuring 3 cm long” Wound Drainage and Odor Exudate Fluid from wound • Document the amount, type and odor • Light, moderate, heavy • Drainage can be clear, sanguineous (bloody), serosanguineous (blood-tinged), -
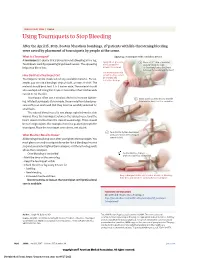
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -
ER Guide to Bleeding Disorders
Bleeding disorders ER guide to bleeding disorders 1 Table of contents 4 General Guidelines 4–5 national Hemophilia Foundation guidelines 5–10 Treatment options 10 HemopHilia a Name:__________________________________________________________________________________________________ 10–11 national Hemophilia Foundation guidelines Address:________________________________________________________________________________________________ 12 dosage chart Phone:__________________________________________________________________________________________________ 14–15 Treatment products 16 HemopHilia B In case of emergency, contact: ______________________________________________________________________________ 16 national Hemophilia Foundation guidelines Relation to patient:________________________________________________________________________________________ 17 dosage chart 18 Treatment products 19 HemopHilia a or B with inHiBiTors Diagnosis: Hemophilia A: Mild Moderate Severe 20 national Hemophilia Foundation guidelines Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 21 Treatment products Hemophilia B: Mild Moderate Severe 22–23 Von willeBrand disease Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 23–24 national Hemophilia Foundation guidelines von Willebrand disease: Type 1 Type 2 Type 3 Platelet type 25 Treatment products 27 Bibliography Preferred product:_________________________________________________________________________________________ Dose for life-threatening