Wound Care: the Basics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -

Energy Healing
57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 61 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. CHAPTER 3 Energy Healing Our remedies oft in ourselves do lie. —WILLIAM SHAKESPEARE LEARNING OBJECTIVES 1. Describe the types of energy. 2. Explain the universal energy field (UEF). 3. Explain the human energy field (HEF). 4. Describe the seven auric layers. 5. Describe the seven chakras. 6. Define the concept of energy healing. 7. Describe various types of energy healing. INTRODUCTION For centuries, traditional healers worldwide have practiced methods of energy healing, viewing the body as a complex energy system with energy flowing through or over its surface (Rakel, 2007). Until recently, the Western world largely ignored the Eastern interpretation of humans as energy beings. However, times have changed dramatically and an exciting and promising new branch of academic inquiry and clinical research is opening in the area of energy healing (Oschman, 2000; Trivieri & Anderson, 2002). Scientists and energy therapists around the world have made discoveries that will forever alter our picture of human energetics. The National Institutes of Health (NIH) is conducting research in areas such as energy healing and prayer, and major U.S. academic institutions are conducting large clinical trials in these areas. Approaches in exploring the concepts of life force and healing energy that previously appeared to compete or conflict have now been found to support each other. Conner and Koithan (2006) note 61 57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 62 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. 62 CHAPTER 3 • ENERGY HEALING that “with increased recognition and federal funding for energetic healing, there is a growing body of research that supports the use of energetic healing interventions with patients” (p. -

Purinergic Signalling in Skin
PURINERGIC SIGNALLING IN SKIN AINA VH GREIG MA FRCS Autonomic Neuroscience Institute Royal Free and University College School of Medicine Rowland Hill Street Hampstead London NW3 2PF in the Department of Anatomy and Developmental Biology University College London Gower Street London WCIE 6BT 2002 Thesis Submitted for the Degree of Doctor of Philosophy University of London ProQuest Number: U643205 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest. ProQuest U643205 Published by ProQuest LLC(2016). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. Microform Edition © ProQuest LLC. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 ABSTRACT Purinergic receptors, which bind ATP, are expressed on human cutaneous kératinocytes. Previous work in rat epidermis suggested functional roles of purinergic receptors in the regulation of proliferation, differentiation and apoptosis, for example P2X5 receptors were expressed on kératinocytes undergoing proliferation and differentiation, while P2X? receptors were associated with apoptosis. In this thesis, the aim was to investigate the expression of purinergic receptors in human normal and pathological skin, where the balance between these processes is changed. A study was made of the expression of purinergic receptor subtypes in human adult and fetal skin. -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

Gunshot Wounds
Gunshot Wounds Michael Sirkin, MD Chief, Orthopaedic Trauma Service Assistant Professor, New Jersey Medical School North Jersey Orthopaedic Institute Created March 2004; Reviewed March 2006, August 2010 Ballistics • Most bullets made of lead alloy – High specific gravity • Maximal mass • Less effect of air resistance • Bullet tips – Pointed – Round – Flat – Hollow Ballistics • Low velocity bullets – Made of low melting point lead alloys – If fired from high velocity they melt, 2° to friction • Deform • Change missile ballistics • High velocity bullets – Coated or jacketed with a harder metal – High temperature coating – Less deformity when fired Velocity • Energy = ½ mv2 • Energy increases by the square of the velocity and linearly with the mass • Velocity of missile is the most important factor determining amount of energy and subsequent tissue damage Kinetic Energy of High and Low Velocity Firearms Kinetic Energy of Shotgun Shells Wounding power • Low velocity, less severe – Less than 1000 ft/sec – Less than 230 grams • High velocity, very destructive – Greater than 2000 ft/sec – Weight less than 150 grams • Shotguns, very destructive at close range – About 1200 ft/sec – Weight up to 870 grams Factors that cause tissue damage • Crush and laceration • Secondary missiles • Cavitation • Shock wave Crush and Laceration • Principle mechanism in low velocity gunshot wounds • Material in path is crushed or lacerated • The kinetic energy is dissipated • Increased tissue damage with yaw or tumble – Increased profile – Increased rate of kinetic -

Pressure Ulcer Staging Cards and Skin Inspection Opportunities.Indd
Pressure Ulcer Staging Pressure Ulcer Staging Suspected Deep Tissue Injury (sDTI): Purple or maroon localized area of discolored Suspected Deep Tissue Injury (sDTI): Purple or maroon localized area of discolored intact skin or blood-fi lled blister due to damage of underlying soft tissue from pressure intact skin or blood-fi lled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, fi rm, mushy, boggy, and/or shear. The area may be preceded by tissue that is painful, fi rm, mushy, boggy, warmer or cooler as compared to adjacent tissue. warmer or cooler as compared to adjacent tissue. Stage 1: Intact skin with non- Stage 1: Intact skin with non- blanchable redness of a localized blanchable redness of a localized area usually over a bony prominence. area usually over a bony prominence. Darkly pigmented skin may not have Darkly pigmented skin may not have visible blanching; its color may differ visible blanching; its color may differ from surrounding area. from surrounding area. Stage 2: Partial thickness loss of Stage 2: Partial thickness loss of dermis presenting as a shallow open dermis presenting as a shallow open ulcer with a red pink wound bed, ulcer with a red pink wound bed, without slough. May also present as without slough. May also present as an intact or open/ruptured serum- an intact or open/ruptured serum- fi lled blister. fi lled blister. Stage 3: Full thickness tissue loss. Stage 3: Full thickness tissue loss. Subcutaneous fat may be visible but Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. -

Penetrating Injury to the Head: Case Reviews K Regunath, S Awang*, S B Siti, M R Premananda, W M Tan, R H Haron**
CASE REPORT Penetrating Injury to the Head: Case Reviews K Regunath, S Awang*, S B Siti, M R Premananda, W M Tan, R H Haron** *Department of Neurosciences, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan, **Department of Neurosurgery, Hospital Kuala Lumpur the right frontal lobe to a depth of approximately 2.5cm. SUMMARY (Figure 1: A & B) There was no obvious intracranial Penetrating injury to the head is considered a form of severe haemorrhage along the track of injury. The patient was taken traumatic brain injury. Although uncommon, most to the operating theatre and was put under general neurosurgical centres would have experienced treating anaesthesia. The nail was cut proximal to the entry wound patients with such an injury. Despite the presence of well and the piece of wood removed. The entry wound was found written guidelines for managing these cases, surgical to be contaminated with hair and debris. The nail was also treatment requires an individualized approach tailored to rusty. A bicoronal skin incision was fashioned centred on the the situation at hand. We describe a collection of three cases entry wound. A bifrontal craniotomy was fashioned and the of non-missile penetrating head injury which were managed bone flap removed sparing a small island of bone around the in two main Neurosurgical centres within Malaysia and the nail (Figure 1: C&D). Bilateral “U” shaped dural incisions unique management approaches for each of these cases. were made with the base to the midline. The nail was found to have penetrated with dura about 0.5cm from the edge of KEY WORDS: Penetrating head injury, nail related injury, atypical penetrating the sagittal sinus. -

VII. Wound and Fracture Healing
Journal of Rehabilitation Research and Development Rehabilitation R & D Progress Reports 1986 VII. Wound and Fracture Healing VII . Wound and Fracture Healing Electrical Stimulation for Augmentation of Wound Healing Scott R. Crowgey, M.D., and Steven M. Sharpe Veterans Administration Research and Development, Decatur, GA 30033 Sponsor: VA Rehabilitation Research and Development Service Purpose—This project will attempt to identify ing that could be influenced by electrical stimu- aspects of the wound healing process that may lation. Efforts will then be directed toward de- be augmented by the exogenous influence of veloping mathematical models of the possible electromagnetic fields. A theoretical analysis of electrical interaction of electromagnetic fields the possible effects of electromagnetic fields on with cells and cell structures to determine how wound healing will include analyses of the these interactions could be optimized to im- interaction of electromagnetic fields with cellu- prove wound healing. It is anticipated that the lar structures and of the deposition of heat in literature will not contain all the information damaged tissue via exogenously applied energy necessary to develop these models . Any gaps in fields. This analysis will then be used as a basis necessary information and data will be filled, if for developing a plan for future investigations practical, using tissue phantom modeling mate- into the potential application of electrical stim- rials, blood, and possibly even primitive tissue ulation for the augmentation of wound healing. culture exposed to a variety of known electro- The initial research will involve a review of magnetic environments, using easily construct- the literature to identify aspects of wound heal- ed exposure chambers. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -
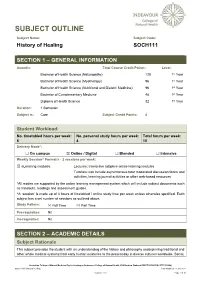
SOCH111 History of Healing Last Modified: 17-Jun-2021
SUBJECT OUTLINE Subject Name: Subject Code: History of Healing SOCH111 SECTION 1 – GENERAL INFORMATION Award/s: Total Course Credit Points: Level: Bachelor of Health Science (Naturopathy) 128 1st Year Bachelor of Health Science (Myotherapy) 96 1st Year Bachelor of Health Science (Nutritional and Dietetic Medicine) 96 1st Year Bachelor of Complementary Medicine 48 1st Year Diploma of Health Science 32 1st Year Duration: 1 Semester Subject is: Core Subject Credit Points: 4 Student Workload: No. timetabled hours per week: No. personal study hours per week: Total hours per week: 6 4 10 Delivery Mode*: ☐ On campus ☒ Online / Digital ☐ Blended ☐ Intensive Weekly Session^ Format/s - 2 sessions per week: ☒ eLearning modules: Lectures: Interactive adaptive online learning modules Tutorials: can include asynchronous tutor moderated discussion forum and activities, learning journal activities or other web-based resources *All modes are supported by the online learning management system which will include subject documents such as handouts, readings and assessment guides. ^A ‘session’ is made up of 3 hours of timetabled / online study time per week unless otherwise specified. Each subject has a set number of sessions as outlined above. Study Pattern: ☒ Full Time ☒ Part Time Pre-requisites: Nil Co-requisites: Nil SECTION 2 – ACADEMIC DETAILS Subject Rationale This subject provides the student with an understanding of the history and philosophy underpinning traditional and other whole medical systems from early human existence to the present day in diverse cultures worldwide. Social, Australian College of Natural Medicine Pty Ltd trading as Endeavour College of Natural Health, FIAFitnation (National CRICOS #00231G, RTO #31489) SOCH111 History of Healing Last modified: 17-Jun-2021 Version: 27.0 Page 1 of 10 cultural and political developments are considered in the evolution of healing and medicine, as well as the parallel developments in anatomy, physiology and other sciences. -

Immune Thrombocytopenic Purpura in a Twin Girl Revealed by a Traumatic Injury in Parakou (North Benin)
Immune thrombocytopenic purpura in a twin girl revealed by a traumatic injury in parakou (North Benin) Adedemy JD 1*, Noudamadjo A 1, Kpanidja G 1, Agossou J 1, Agbeille Mohamed F 1, Dovonou CA 2 1 Mother and Child Department, Parakou Teaching Hospital, Republic of Benin, and Faculty of Medicine, University of Parakou West Africa 2 Department of Medicine, Parakou Teaching Hospital, and Faculty of Medicine, University of Parakou, West Africa Abstract Background: ITP seems to be rare but in tropical settings thrombocytopenia is often encountered among children. Objective: Authors through this case report are putting emphasy on the diagnosis and management of ITP in a 4 year old twin girl admitted in the pediatric emergency ward for hematuria and bleeding from various origins seen in the context of a domestic trauma. Results: The various clinical signs have been analyzed to confirm ITP through exclusion of other possible health conditions. The management of ITP depend on the severity of clinical signs and in some cases the situations can be life threatening. In this case report, Blood transfusion and corticosteroids were the main treatment tools. The hospital stay was about 47 days and an ambulatory follow up was conducted for almost 6 months. Conclusion: In the context of various bleeding disorders, hematuria and thrombocytopenia, autoimmune thrombocytopenia in a twin girl was revealed by a domestic trauma. Citation: Adedemy JD, Noudamadjo A, Kpanidja G, Agossou J, Agbeille MF, Dovonou CA (2019) Immune Thrombocytopenic Purpura in a twin girl revealed by a traumatic injury in Parakou (North Benin). Adv Pediatr Res 6:27. -
Suturing with U-Technique Versus Un
Official Title of the Study: Suturing with U-Technique versus Un- Reapproximated wound Edges during removal of Closed Thoracostomy-tube drain - A single centre Open-label randomized prospective trial (SUTURE TRIAL) NCT NUMBER: Not Yet Assigned DATE OF DOCUMENT: January 16, 2019 1 STUDY SUMMARY Title: Suturing with U-Technique versus Un-Reapproximated wound Edges during removal of Closed Thoracostomy-tube drain - A single centre Open-label randomized prospective trial (SUTURE TRIAL) Background: Closed thoracostomy tube drainage or chest tube insertion is one of the most commonly performed procedures in thoracic surgery. There are several published evidence-based guidelines on safe performance of a chest tube insertion. However, there is absence of prospective controlled trials or systematic reviews indicating the safest technique of closing the wound created at the time of chest tube insertion and that best guarantees good wound and overall outcomes, post-chest tube removal. The use of a horizontal mattress non-absorbable suture or U- suture which is placed at the time of chest tube insertion and used to create a purse-string wound re-approximation at the time of tube removal has been an age-long and time-honored practice in most thoracic surgical settings. It has been established by a recent study that an occlusive adhesive-absorbent dressing can also be safely used to occlude the wound at the time of chest tube removal with good wound and overall outcomes though the study focused on tubes inserted during thoracic surgical operations.