Purinergic Signalling in Skin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Energy Healing
57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 61 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. CHAPTER 3 Energy Healing Our remedies oft in ourselves do lie. —WILLIAM SHAKESPEARE LEARNING OBJECTIVES 1. Describe the types of energy. 2. Explain the universal energy field (UEF). 3. Explain the human energy field (HEF). 4. Describe the seven auric layers. 5. Describe the seven chakras. 6. Define the concept of energy healing. 7. Describe various types of energy healing. INTRODUCTION For centuries, traditional healers worldwide have practiced methods of energy healing, viewing the body as a complex energy system with energy flowing through or over its surface (Rakel, 2007). Until recently, the Western world largely ignored the Eastern interpretation of humans as energy beings. However, times have changed dramatically and an exciting and promising new branch of academic inquiry and clinical research is opening in the area of energy healing (Oschman, 2000; Trivieri & Anderson, 2002). Scientists and energy therapists around the world have made discoveries that will forever alter our picture of human energetics. The National Institutes of Health (NIH) is conducting research in areas such as energy healing and prayer, and major U.S. academic institutions are conducting large clinical trials in these areas. Approaches in exploring the concepts of life force and healing energy that previously appeared to compete or conflict have now been found to support each other. Conner and Koithan (2006) note 61 57618_CH03_Pass2.QXD 10/30/08 1:19 PM Page 62 © Jones and Bartlett Publishers, LLC. NOT FOR SALE OR DISTRIBUTION. 62 CHAPTER 3 • ENERGY HEALING that “with increased recognition and federal funding for energetic healing, there is a growing body of research that supports the use of energetic healing interventions with patients” (p. -

Wound Classification
Wound Classification Presented by Dr. Karen Zulkowski, D.N.S., RN Montana State University Welcome! Thank you for joining this webinar about how to assess and measure a wound. 2 A Little About Myself… • Associate professor at Montana State University • Executive editor of the Journal of the World Council of Enterstomal Therapists (JWCET) and WCET International Ostomy Guidelines (2014) • Editorial board member of Ostomy Wound Management and Advances in Skin and Wound Care • Legal consultant • Former NPUAP board member 3 Today We Will Talk About • How to assess a wound • How to measure a wound Please make a note of your questions. Your Quality Improvement (QI) Specialists will follow up with you after this webinar to address them. 4 Assessing and Measuring Wounds • You completed a skin assessment and found a wound. • Now you need to determine what type of wound you found. • If it is a pressure ulcer, you need to determine the stage. 5 Assessing and Measuring Wounds This is important because— • Each type of wound has a different etiology. • Treatment may be very different. However— • Not all wounds are clear cut. • The cause may be multifactoral. 6 Types of Wounds • Vascular (arterial, venous, and mixed) • Neuropathic (diabetic) • Moisture-associated dermatitis • Skin tear • Pressure ulcer 7 Mixed Etiologies Many wounds have mixed etiologies. • There may be both venous and arterial insufficiency. • There may be diabetes and pressure characteristics. 8 Moisture-Associated Skin Damage • Also called perineal dermatitis, diaper rash, incontinence-associated dermatitis (often confused with pressure ulcers) • An inflammation of the skin in the perineal area, on and between the buttocks, into the skin folds, and down the inner thighs • Scaling of the skin with papule and vesicle formation: – These may open, with “weeping” of the skin, which exacerbates skin damage. -

P2Y Purinergic Receptors, Endothelial Dysfunction, and Cardiovascular Diseases
International Journal of Molecular Sciences Review P2Y Purinergic Receptors, Endothelial Dysfunction, and Cardiovascular Diseases Derek Strassheim 1, Alexander Verin 2, Robert Batori 2 , Hala Nijmeh 3, Nana Burns 1, Anita Kovacs-Kasa 2, Nagavedi S. Umapathy 4, Janavi Kotamarthi 5, Yash S. Gokhale 5, Vijaya Karoor 1, Kurt R. Stenmark 1,3 and Evgenia Gerasimovskaya 1,3,* 1 The Department of Medicine Cardiovascular and Pulmonary Research Laboratory, University of Colorado Denver, Aurora, CO 80045, USA; [email protected] (D.S.); [email protected] (N.B.); [email protected] (V.K.); [email protected] (K.R.S.) 2 Vascular Biology Center, Augusta University, Augusta, GA 30912, USA; [email protected] (A.V.); [email protected] (R.B.); [email protected] (A.K.-K.) 3 The Department of Pediatrics, Division of Critical Care Medicine, University of Colorado Denver, Aurora, CO 80045, USA; [email protected] 4 Center for Blood Disorders, Augusta University, Augusta, GA 30912, USA; [email protected] 5 The Department of BioMedical Engineering, University of Wisconsin, Madison, WI 53706, USA; [email protected] (J.K.); [email protected] (Y.S.G.) * Correspondence: [email protected]; Tel.: +1-303-724-5614 Received: 25 August 2020; Accepted: 15 September 2020; Published: 18 September 2020 Abstract: Purinergic G-protein-coupled receptors are ancient and the most abundant group of G-protein-coupled receptors (GPCRs). The wide distribution of purinergic receptors in the cardiovascular system, together with the expression of multiple receptor subtypes in endothelial cells (ECs) and other vascular cells demonstrates the physiological importance of the purinergic signaling system in the regulation of the cardiovascular system. -

Hypoxia Modulates Platelet Purinergic Signalling Pathways
Published online: 2019-12-13 THIEME Cellular Haemostasis and Platelets 253 Hypoxia Modulates Platelet Purinergic Signalling Pathways Gordon G. Paterson1,2 Jason M. Young1,2 Joseph A. Willson3 Christopher J. Graham1,2 Rebecca C. Dru1,2 Eleanor W. Lee1,2 Greig S. Torpey1,2 Sarah R. Walmsley3 Melissa V. Chan4 Timothy D. Warner4 John Kenneth Baillie1,5,6 Alfred Arthur Roger Thompson1,7 1 APEX (Altitude Physiology Expeditions), Edinburgh, United Kingdom Address for correspondence Alfred Arthur Roger Thompson, BSc, MB 2 Edinburgh Medical School, University of Edinburgh, Edinburgh, ChB,MRCP,PhD,DepartmentofInfection,Immunityand United Kingdom Cardiovascular Disease, University of Sheffield, M127a, Royal 3 University of Edinburgh Centre for Inflammation Research, The Hallamshire Hospital, Beech Hill Road, Sheffield S10 2RX, Queen’s Medical Research Institute, University of Edinburgh, United Kingdom (e-mail: R.Thompson@sheffield.ac.uk). Edinburgh, United Kingdom 4 Centre for Immunobiology, Blizard Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, London, United Kingdom 5 Division of Genetics and Genomics, The Roslin Institute, University of Edinburgh, Edinburgh, United Kingdom 6 Department of Anaesthesia, Critical Care and Pain Medicine, Royal Infirmary of Edinburgh, NHS Lothian, Edinburgh, United Kingdom 7 Department of Infection, Immunity and Cardiovascular Disease, University of Sheffield, Sheffield, United Kingdom Thromb Haemost 2020;120:253–261. Abstract Background Hypoxia resulting from ascent to high-altitude or pathological states at sea level is known to increase platelet reactivity. Previous work from our group has suggested that this may be adenosine diphosphate (ADP)-specific. Given the clinical importance of drugs targeting ADP pathways, research into the impact of hypoxia on platelet ADP pathways is highly important. -

Alzheimer and Purinergic Signaling: Just a Matter of Inflammation?
cells Review Alzheimer and Purinergic Signaling: Just a Matter of Inflammation? Stefania Merighi 1, Tino Emanuele Poloni 2, Anna Terrazzan 1, Eva Moretti 1, Stefania Gessi 1,* and Davide Ferrari 3,* 1 Department of Translational Medicine and for Romagna, University of Ferrara, 44100 Ferrara, Italy; [email protected] (S.M.); [email protected] (A.T.); [email protected] (E.M.) 2 Department of Neurology and Neuropathology, Golgi-Cenci Foundation & ASP Golgi-Redaelli, Abbiategrasso, 20081 Milan, Italy; [email protected] 3 Department of Life Science and Biotechnology, University of Ferrara, 44100 Ferrara, Italy * Correspondence: [email protected] (S.G.); [email protected] (D.F.) Abstract: Alzheimer’s disease (AD) is a widespread neurodegenerative pathology responsible for about 70% of all cases of dementia. Adenosine is an endogenous nucleoside that affects neurode- generation by activating four membrane G protein-coupled receptor subtypes, namely P1 receptors. One of them, the A2A subtype, is particularly expressed in the brain at the striatal and hippocampal levels and appears as the most promising target to counteract neurological damage and adenosine- dependent neuroinflammation. Extracellular nucleotides (ATP, ADP, UTP, UDP, etc.) are also released from the cell or are synthesized extracellularly. They activate P2X and P2Y membrane receptors, eliciting a variety of physiological but also pathological responses. Among the latter, the chronic inflammation underlying AD is mainly caused by the P2X7 receptor subtype. In this review we offer an overview of the scientific evidence linking P1 and P2 mediated purinergic signaling to AD devel- opment. We will also discuss potential strategies to exploit this knowledge for drug development. -
Wound Care: the Basics
Wound Care: The Basics Suzann Williams-Rosenthal, RN, MSN, WOC, GNP Norma Branham, RN, MSN, WOC, GNP University of Virginia May, 2010 What Type of Wound is it? How long has it been there? Acute-generally heal in a couple weeks, but can become chronic: Surgical Trauma Chronic -do not heal by normal repair process-takes weeks to months: Vascular-venous stasis, arterial ulcers Pressure ulcers Diabetic foot ulcers (neuropathic) Chronic Wounds Pressure Ulcer Staging Where is it? Where is it located? Use anatomical location-heel, ankle, sacrum, coccyx, etc. Measurements-in centimeters Length X Width X Depth • Length = greatest length (head to toe) • Width = greatest width (side to side) • Depth = measure by marking the depth with a Q- Tip and then hold to a ruler Wound Characteristics: Describe by percentage of each type of tissue: Granulation tissue: • red, cobblestone appearance (healing, filling in) Necrotic: • Slough-yellow, tan dead tissue (devitalized) • Eschar-black/brown necrotic tissue, can be hard or soft Evaluating additional tissue damage: Undermining Separation of tissue from the surface under the edge of the wound • Describe by clock face with patients head at 12 (“undermining is 1 cm from 12 to 4 o’clock”) Tunneling Channel that runs from the wound edge through to other tissue • “tunneling at 9 o’clock, measuring 3 cm long” Wound Drainage and Odor Exudate Fluid from wound • Document the amount, type and odor • Light, moderate, heavy • Drainage can be clear, sanguineous (bloody), serosanguineous (blood-tinged), -
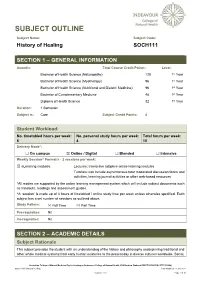
SOCH111 History of Healing Last Modified: 17-Jun-2021
SUBJECT OUTLINE Subject Name: Subject Code: History of Healing SOCH111 SECTION 1 – GENERAL INFORMATION Award/s: Total Course Credit Points: Level: Bachelor of Health Science (Naturopathy) 128 1st Year Bachelor of Health Science (Myotherapy) 96 1st Year Bachelor of Health Science (Nutritional and Dietetic Medicine) 96 1st Year Bachelor of Complementary Medicine 48 1st Year Diploma of Health Science 32 1st Year Duration: 1 Semester Subject is: Core Subject Credit Points: 4 Student Workload: No. timetabled hours per week: No. personal study hours per week: Total hours per week: 6 4 10 Delivery Mode*: ☐ On campus ☒ Online / Digital ☐ Blended ☐ Intensive Weekly Session^ Format/s - 2 sessions per week: ☒ eLearning modules: Lectures: Interactive adaptive online learning modules Tutorials: can include asynchronous tutor moderated discussion forum and activities, learning journal activities or other web-based resources *All modes are supported by the online learning management system which will include subject documents such as handouts, readings and assessment guides. ^A ‘session’ is made up of 3 hours of timetabled / online study time per week unless otherwise specified. Each subject has a set number of sessions as outlined above. Study Pattern: ☒ Full Time ☒ Part Time Pre-requisites: Nil Co-requisites: Nil SECTION 2 – ACADEMIC DETAILS Subject Rationale This subject provides the student with an understanding of the history and philosophy underpinning traditional and other whole medical systems from early human existence to the present day in diverse cultures worldwide. Social, Australian College of Natural Medicine Pty Ltd trading as Endeavour College of Natural Health, FIAFitnation (National CRICOS #00231G, RTO #31489) SOCH111 History of Healing Last modified: 17-Jun-2021 Version: 27.0 Page 1 of 10 cultural and political developments are considered in the evolution of healing and medicine, as well as the parallel developments in anatomy, physiology and other sciences. -

Caffeine Has a Dual Influence on NMDA Receptor–Mediated Glutamatergic Transmission at the Hippocampus
Purinergic Signalling https://doi.org/10.1007/s11302-020-09724-z ORIGINAL ARTICLE Caffeine has a dual influence on NMDA receptor–mediated glutamatergic transmission at the hippocampus Robertta S. Martins1,2 & Diogo M. Rombo1,3 & Joana Gonçalves-Ribeiro1,3 & Carlos Meneses4 & Vladimir P. P. Borges-Martins2 & Joaquim A. Ribeiro1,3 & Sandra H. Vaz1,3 & Regina C. C. Kubrusly2 & Ana M. Sebastião1,3 Received: 19 June 2020 /Accepted: 20 August 2020 # Springer Nature B.V. 2020 Abstract Caffeine, a stimulant largely consumed around the world, is a non-selective adenosine receptor antagonist, and therefore caffeine actions at synapses usually, but not always, mirror those of adenosine. Importantly, different adenosine receptors with opposing regulatory actions co-exist at synapses. Through both inhibitory and excitatory high-affinity receptors (A1RandA2R, respec- tively), adenosine affects NMDA receptor (NMDAR) function at the hippocampus, but surprisingly, there is a lack of knowledge on the effects of caffeine upon this ionotropic glutamatergic receptor deeply involved in both positive (plasticity) and negative (excitotoxicity) synaptic actions. We thus aimed to elucidate the effects of caffeine upon NMDAR-mediated excitatory post- synaptic currents (NMDAR-EPSCs), and its implications upon neuronal Ca2+ homeostasis. We found that caffeine (30–200 μM) facilitates NMDAR-EPSCs on pyramidal CA1 neurons from Balbc/ByJ male mice, an action mimicked, as well as occluded, by 1,3-dipropyl-cyclopentylxantine (DPCPX, 50 nM), thus likely mediated by blockade of inhibitory A1Rs. This action of caffeine cannot be attributed to a pre-synaptic facilitation of transmission because caffeine even increased paired-pulse facilitation of NMDA-EPSCs, indicative of an inhibition of neurotransmitter release. -

Collagen in Wound Healing
bioengineering Review Collagen in Wound Healing Shomita S. Mathew-Steiner, Sashwati Roy and Chandan K. Sen * Indiana Center for Regenerative Medicine and Engineering, School of Medicine, Indiana University, Indianapolis, IN 46202, USA; [email protected] (S.S.M.-S.); [email protected] (S.R.) * Correspondence: [email protected]; Tel.: +1-317-278-2735 Abstract: Normal wound healing progresses through inflammatory, proliferative and remodeling phases in response to tissue injury. Collagen, a key component of the extracellular matrix, plays critical roles in the regulation of the phases of wound healing either in its native, fibrillar conformation or as soluble components in the wound milieu. Impairments in any of these phases stall the wound in a chronic, non-healing state that typically requires some form of intervention to guide the process back to completion. Key factors in the hostile environment of a chronic wound are persistent inflammation, increased destruction of ECM components caused by elevated metalloproteinases and other enzymes and improper activation of soluble mediators of the wound healing process. Collagen, being central in the regulation of several of these processes, has been utilized as an adjunct wound therapy to promote healing. In this work the significance of collagen in different biological processes relevant to wound healing are reviewed and a summary of the current literature on the use of collagen-based products in wound care is provided. Keywords: extracellular matrix; collagen; signaling; inflammation; wound healing; collagen dressings; engineered collagen Citation: Mathew-Steiner, S.S.; Roy, S.; Sen, C.K. Collagen in Wound 1. Introduction Healing. Bioengineering 2021, 8, 63. Sophisticated regulation by a number of key factors including the environment of the https://doi.org/10.3390/ wound which is rich in extracellular matrix (ECM) drives the process of wound healing [1,2]. -

Regulation of Microglial Functions by Purinergic Mechanisms in the Healthy and Diseased CNS
cells Review Regulation of Microglial Functions by Purinergic Mechanisms in the Healthy and Diseased CNS Peter Illes 1,2,*, Patrizia Rubini 2, Henning Ulrich 3, Yafei Zhao 4 and Yong Tang 2,4 1 Rudolf Boehm Institute for Pharmacology and Toxicology, University of Leipzig, 04107 Leipzig, Germany 2 International Collaborative Centre on Big Science Plan for Purine Signalling, Chengdu University of Traditional Chinese Medicine, Chengdu 610075, China; [email protected] (P.R.); [email protected] (Y.T.) 3 Department of Biochemistry, Institute of Chemistry, University of São Paulo, São Paulo 748, Brazil; [email protected] 4 Acupuncture and Tuina School, Chengdu University of Traditional Chinese Medicine, Chengdu 610075, China; [email protected] * Correspondence: [email protected]; Tel.: +49-34-1972-46-14 Received: 17 March 2020; Accepted: 27 April 2020; Published: 29 April 2020 Abstract: Microglial cells, the resident macrophages of the central nervous system (CNS), exist in a process-bearing, ramified/surveying phenotype under resting conditions. Upon activation by cell-damaging factors, they get transformed into an amoeboid phenotype releasing various cell products including pro-inflammatory cytokines, chemokines, proteases, reactive oxygen/nitrogen species, and the excytotoxic ATP and glutamate. In addition, they engulf pathogenic bacteria or cell debris and phagocytose them. However, already resting/surveying microglia have a number of important physiological functions in the CNS; for example, they shield small disruptions of the blood–brain barrier by their processes, dynamically interact with synaptic structures, and clear surplus synapses during development. In neurodegenerative illnesses, they aggravate the original disease by a microglia-based compulsory neuroinflammatory reaction. -

Purinergic Receptors Brian F
Chapter 21 Purinergic receptors Brian F. King and Geoffrey Burnstock 21.1 Introduction The term purinergic receptor (or purinoceptor) was first introduced to describe classes of membrane receptors that, when activated by either neurally released ATP (P2 purinoceptor) or its breakdown product adenosine (P1 purinoceptor), mediated relaxation of gut smooth muscle (Burnstock 1972, 1978). P2 purinoceptors were further divided into five broad phenotypes (P2X, P2Y, P2Z, P2U, and P2T) according to pharmacological profile and tissue distribution (Burnstock and Kennedy 1985; Gordon 1986; O’Connor et al. 1991; Dubyak 1991). Thereafter, they were reorganized into families of metabotropic ATP receptors (P2Y, P2U, and P2T) and ionotropic ATP receptors (P2X and P2Z) (Dubyak and El-Moatassim 1993), later redefined as extended P2Y and P2X families (Abbracchio and Burnstock 1994). In the early 1990s, cDNAs were isolated for three heptahelical proteins—called P2Y1, P2Y2, and P2Y3—with structural similarities to the rhodopsin GPCR template. At first, these three GPCRs were believed to correspond to the P2Y, P2U, and P2T receptors. However, the com- plexity of the P2Y receptor family was underestimated. At least 15, possibly 16, heptahelical proteins have been associated with the P2Y receptor family (King et al. 2001, see Table 21.1). Multiple expression of P2Y receptors is considered the norm in all tissues (Ralevic and Burnstock 1998) and mixtures of P2 purinoceptors have been reported in central neurones (Chessell et al. 1997) and glia (King et al. 1996). The situation is compounded by P2Y protein dimerization to generate receptor assemblies with subtly distinct pharmacological proper- ties from their constituent components (Filippov et al. -

Products & Technology Wound Inflammation and the Role of A
Products & technology Wound inflammation and the role of a multifunctional polymeric dressing Temporary inflammation is a normal response in acute wound healing. However, in chronic wounds, the inflammatory phase is dysfunctional in nature. This results in delayed healing, and causes further problems such as increased pain, odour and Intro high levels of exudate production. It is important to choose a dressing that addresses all of these factors while meeting the patient’s needs. Multifunctional polymeric Authors: Keith F Cutting membrane dressings (e.g. PolyMem®, Ferris) can help to simplify this choice and Authors: Peter Vowden assist healthcare professionals in chronic wound care. The unique actions of xxxxx Cornelia Wiegand PolyMem® have been proven to reduce and prevent inflammation, swelling, bruising and pain to promote rapid healing, working in the deep tissues beneath the skin[1,2]. he mechanism of acute wound healing — the vascular and cellular stages. During is a well-described complex cellular vascular response, immediately on injury there is T interaction[3] that can be divided into an initial transient vasoconstriction that can be several integrated processes: haemostasis, measured in seconds. This is promptly followed inflammation, proliferation, epithelialisation by vasodilation under the influence of histamine and tissue remodeling. Inflammation is a key and nitric oxide (NO) that cause an inflow of blood. component of acute wound healing, clearing An increase in vascular permeability promotes damaged extracellular matrix, cells and debris leakage of serous fluid (protein-rich exudate) into from zones of tissue damage. This is normally a the extravascular compartment, which in turn time-limited orchestrated process. Successful increases the concentration of cells and clotting progression of the inflammatory phase allows factors.