Spontaneous Hemopericardium Leading to Cardiac Tamponade in a Patient with Essential Thrombocythemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evidence of Atrial Functional Mitral Regurgitation Due to Atrial Fibrillation Reversal with Arrhythmia Control
Journal of the American College of Cardiology Vol. 58, No. 14, 2011 © 2011 by the American College of Cardiology Foundation ISSN 0735-1097/$36.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2011.06.032 Heart Rhythm Disorders Evidence of Atrial Functional Mitral Regurgitation Due to Atrial Fibrillation Reversal With Arrhythmia Control Zachary M. Gertz, MD,* Amresh Raina, MD,* Laszlo Saghy, MD,† Erica S. Zado, PA-C,* David J. Callans, MD,* Francis E. Marchlinski, MD,* Martin G. Keane, MD,* Frank E. Silvestry, MD* Philadelphia, Pennsylvania; and Szeged, Hungary Objectives The purpose of this study was to determine whether atrial fibrillation (AF) might cause significant mitral regurgi- tation (MR), and to see whether this MR improves with restoration of sinus rhythm. Background MR can be classified by leaflet pathology (organic/primary and functional/secondary) and by leaflet motion (nor- mal, excessive, restrictive). The existence of secondary, normal leaflet motion MR remains controversial. Methods We performed a retrospective cohort study. Patients undergoing first AF ablation at our institution (n ϭ 828) were screened. Included patients had echocardiograms at the time of ablation and at 1-year clinical follow-up. The MR cohort (n ϭ 53) had at least moderate MR. A reference cohort (n ϭ 53) was randomly selected from those patients (n ϭ 660) with mild or less MR. Baseline echocardiographic and clinical characteristics were compared, and the effect of restoration of sinus rhythm was assessed by follow-up echocardiograms. Results MR patients were older than controls and more often had persistent AF (62% vs. 23%, p Ͻ 0.0001). -

081999 Disseminated Intravascular Coagulation
The New England Journal of Medicine Current Concepts Systemic activation+ of coagulation DISSEMINATED INTRAVASCULAR COAGULATION Intravascular+ Depletion of platelets+ deposition of fibrin and coagulation factors MARCEL LEVI, M.D., AND HUGO TEN CATE, M.D. Thrombosis of small+ Bleeding and midsize vessels+ ISSEMINATED intravascular coagulation is and organ failure characterized by the widespread activation Dof coagulation, which results in the intravas- Figure 1. The Mechanism of Disseminated Intravascular Coag- cular formation of fibrin and ultimately thrombotic ulation. occlusion of small and midsize vessels.1-3 Intravascu- Systemic activation of coagulation leads to widespread intra- lar coagulation can also compromise the blood sup- vascular deposition of fibrin and depletion of platelets and co- agulation factors. As a result, thrombosis of small and midsize ply to organs and, in conjunction with hemodynam- vessels may occur, contributing to organ failure, and there may ic and metabolic derangements, may contribute to be severe bleeding. the failure of multiple organs. At the same time, the use and subsequent depletion of platelets and coag- ulation proteins resulting from the ongoing coagu- lation may induce severe bleeding (Fig. 1). Bleeding may be the presenting symptom in a patient with disseminated intravascular coagulation, a factor that can complicate decisions about treatment. TABLE 1. COMMON CLINICAL CONDITIONS ASSOCIATED WITH DISSEMINATED ASSOCIATED CLINICAL CONDITIONS INTRAVASCULAR COAGULATION. AND INCIDENCE Sepsis Infectious Disease Trauma Serious tissue injury Disseminated intravascular coagulation is an ac- Head injury Fat embolism quired disorder that occurs in a wide variety of clin- Cancer ical conditions, the most important of which are listed Myeloproliferative diseases in Table 1. -

What Everyone Should Know to Stop Bleeding After an Injury
What Everyone Should Know to Stop Bleeding After an Injury THE HARTFORD CONSENSUS The Joint Committee to Increase Survival from Active Shooter and Intentional Mass Casualty Events was convened by the American College of Surgeons in response to the growing number and severity of these events. The committee met in Hartford Connecticut and has produced a number of documents with rec- ommendations. The documents represent the consensus opinion of a multi-dis- ciplinary committee involving medical groups, the military, the National Security Council, Homeland Security, the FBI, law enforcement, fire rescue, and EMS. These recommendations have become known as the Hartford Consensus. The overarching principle of the Hartford Consensus is that no one should die from uncontrolled bleeding. The Hartford Consensus recommends that all citizens learn to stop bleeding. Further information about the Hartford Consensus and bleeding control can be found on the website: Bleedingcontrol.org 2 SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury Authors: Peter T. Pons, MD, FACEP Lenworth Jacobs, MD, MPH, FACS Acknowledgements: The authors acknowledge the contributions of Michael Cohen and James “Brooks” Hart, CMI to the design of this manual. Some images adapted from Adam Wehrle, EMT-P and NAEMT. © 2017 American College of Surgeons CONTENTS SECTION 1 3 ■ Introduction ■ Primary Principles of Trauma Care Response ■ The ABCs of Bleeding SECTION 2 5 ■ Ensure Your Own Safety SECTION 3 6 ■ A – Alert – call 9-1-1 SECTION 4 7 ■ B – Bleeding – find the bleeding injury SECTION 5 9 ■ C – Compress – apply pressure to stop the bleeding by: ■ Covering the wound with a clean cloth and applying pressure by pushing directly on it with both hands, OR ■Using a tourniquet, OR ■ Packing (stuff) the wound with gauze or a clean cloth and then applying pressure with both hands SECTION 6 13 ■ Summary 2 SECTION 1: INTRODUCTION Welcome to the Stop the Bleed: Bleeding Control for the Injured information booklet. -

Clinical Manifestation and Survival of Patients with I Diopathic Bilateral
ORIGINAL ARTICLE Clinical Manifestation and Survival of Patients with Mizuhiro Arima, TatsujiI diopathicKanoh, Shinya BilateralOkazaki, YoshitakaAtrialIwama,DilatationAkira Yamasaki and Sigeru Matsuda Westudied the histories of eight patients who lacked clear evidence of cardiac abnormalities other than marked bilateral atrial dilatation and atrial fibrillation, which have rarely been dis- cussed in the literature. From the time of their first visit to our hospital, the patients' chest radio- graphs and electrocardiograms showed markedly enlarged cardiac silhouettes and atrial fibrilla- tion, respectively. Each patient's echocardiogram showed a marked bilateral atrial dilatation with almost normal wall motion of both ventricles. In one patient, inflammatory change was demonstrated by cardiac catheterization and endomyocardial biopsy from the right ventricle. Seven of our eight cases were elderly women.Over a long period after the diagnosis of cardiome- galy or arrhythmia, diuretics or digitalis offered good results in the treatment of edema and congestion in these patients. In view of the clinical courses included in the present study, we conclude that this disorder has a good prognosis. (Internal Medicine 38: 112-118, 1999) Key words: cardiomegaly, atrial fibrillation, elder women,good prognosis Introduction echocardiography. The severity of mitral and tricuspid regur- gitation was globally assessed by dividing into three equal parts Idiopathic enlargement of the right atrium was discussed by the distance from the valve orifice. The regurgitant jet was de- Bailey in 1955(1). This disorder may be an unusual congenital tected on color Doppler recording in the four-chamber view malformation. A review of the international literature disclosed and classified into one of the three regions (-: none, +: mild, that although several cases have been discussed since Bailey's ++:moderate, +++: severe). -
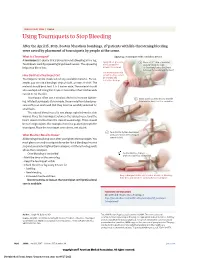
Using Tourniquets to Stop Bleeding
JAMA PATIENT PAGE | Trauma Using Tourniquets to Stop Bleeding After the April 15, 2013, Boston Marathon bombings, 27 patients with life-threatening bleeding were saved by placement of tourniquets by people at the scene. What Is a Tourniquet? Applying a tourniquet with a windlass device A tourniquet is a device that is placed around a bleeding arm or leg. Apply direct pressure 1 Place a 2-3” strip of material Tourniquets work by squeezing large blood vessels. The squeezing to the wound for about 2” from the edge helps stop blood loss. at least 15 minutes. of the wound over a long bone between the wound and the heart. Use a tourniquet only How Do I Put a Tourniquet On? when bleeding cannot be stopped and Tourniquets can be made out of any available material. For ex- is life threatening. ample, you can use a bandage, strip of cloth, or even a t-shirt. The material should be at least 2 to 3 inches wide. The material should also overlap itself. Using thin straps or material less than 2 inches wide can rip or cut the skin. Tourniquets often use a windlass device to increase tighten- 2 Insert a stick or other strong, straight ing. Inflated tourniquets (for example, those made from blood pres- item into the knot to act as a windlass. sure cuffs) can work well. But they must be carefully watched for small leaks. The injured blood vessel is not always right below the skin wound. Place the tourniquet between the injured vessel and the heart, about 2 inches from the closest wound edge. -
ER Guide to Bleeding Disorders
Bleeding disorders ER guide to bleeding disorders 1 Table of contents 4 General Guidelines 4–5 national Hemophilia Foundation guidelines 5–10 Treatment options 10 HemopHilia a Name:__________________________________________________________________________________________________ 10–11 national Hemophilia Foundation guidelines Address:________________________________________________________________________________________________ 12 dosage chart Phone:__________________________________________________________________________________________________ 14–15 Treatment products 16 HemopHilia B In case of emergency, contact: ______________________________________________________________________________ 16 national Hemophilia Foundation guidelines Relation to patient:________________________________________________________________________________________ 17 dosage chart 18 Treatment products 19 HemopHilia a or B with inHiBiTors Diagnosis: Hemophilia A: Mild Moderate Severe 20 national Hemophilia Foundation guidelines Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 21 Treatment products Hemophilia B: Mild Moderate Severe 22–23 Von willeBrand disease Inhibitors Inhibitors Bethesda units (if known) ____________________________________ 23–24 national Hemophilia Foundation guidelines von Willebrand disease: Type 1 Type 2 Type 3 Platelet type 25 Treatment products 27 Bibliography Preferred product:_________________________________________________________________________________________ Dose for life-threatening -
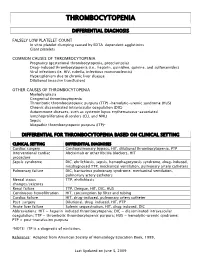
Thrombocytopenia.Pdf
THROMBOCYTOPENIA DIFFERENTIAL DIAGNOSIS FALSELY LOW PLATELET COUNT In vitro platelet clumping caused by EDTA-dependent agglutinins Giant platelets COMMON CAUSES OF THROMBOCYTOPENIA Pregnancy (gestational thrombocytopenia, preeclampsia) Drug-induced thrombocytopenia (i.e., heparin, quinidine, quinine, and sulfonamides) Viral infections (ie. HIV, rubella, infectious mononucleosis) Hypersplenism due to chronic liver disease Dilutional (massive transfusion) OTHER CAUSES OF THROMBOCYTOPENIA Myelodysplasia Congenital thrombocytopenia Thrombotic thrombocytopenic purpura (TTP) -hemolytic-uremic syndrome (HUS) Chronic disseminated intravascular coagulation (DIC) Autoimmune diseases, such as systemic lupus erythematosus-associated lymphoproliferative disorders (CLL and NHL) Sepsis Idiopathic thrombocytopenic purpura (ITP)* DIFFERENTIAL FOR THROMBOCYTOPENIA BASED ON CLINICAL SETTING CLINICAL SETTING DIFFERENTIAL DIAGNOSES Cardiac surgery Cardiopulmonary bypass, HIT, dilutional thrombocytopenia, PTP Interventional cardiac Abciximab or other IIb/IIIa blockers, HIT procedure Sepsis syndrome DIC, ehrlichiosis, sepsis, hemophagocytosis syndrome, drug-induced, misdiagnosed TTP, mechanical ventilation, pulmonary artery catheters Pulmonary failure DIC, hantavirus pulmonary syndrome, mechanical ventilation, pulmonary artery catheters Mental status TTP, ehrlichiosis changes/seizures Renal failure TTP, Dengue, HIT, DIC, HUS Continuous hemofiltration HIT, consumption by filter and tubing Cardiac failure HIT, drug-induced, pulmonary artery catheter Post-surgery -

Rheumatic Mitral Valve Stenosis: Diagnosis and Treatment Options
Current Cardiology Reports (2019) 21: 14 https://doi.org/10.1007/s11886-019-1099-7 STRUCTURAL HEART DISEASE (RJ SIEGEL AND NC WUNDERLICH, SECTION EDITORS) Rheumatic Mitral Valve Stenosis: Diagnosis and Treatment Options Nina C. Wunderlich1 & Bharat Dalvi2 & Siew Yen Ho3 & Harald Küx1 & Robert J. Siegel4 Published online: 28 February 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review This review provides an update on rheumatic mitral stenosis. Acute rheumatic fever (RF), the sequela of group A β-hemolytic streptococcal infection, is the major etiology for mitral stenosis (MS). Recent Findings While the incidence of acute RF in the Western world had substantially declined over the past five decades, this trend is reversing due to immigration from non-industrialized countries where rheumatic heart disease (RHD) is higher. Pre- procedural evaluation for treatment of MS using a multimodality approach with 2D and 3D transthoracic and transesophageal echo, stress echo, cardiac CT scanning, and cardiac MRI as well as hemodynamic assessment by cardiac catheterization is discussed. The current methods of percutaneous mitral balloon commissurotomy (PMBC) and surgery are also discussed. New data on long-term follow-up after PMBC is also presented. Summary For severe rheumatic MS, medical therapy is ineffective and definitive therapy entails PMBC in patients with suitable morphological mitral valve (MV) characteristics, or surgery. As procedural outcomes depend heavily on appropriate case selection, definitive imaging and interpretation are crucial. It is also important to understand the indications as well as morpho- logical MV characteristics to identify the appropriate treatment with PMBC or surgery. -

Ten Patient Stories Illustrating the Extraordinarily Diverse Clinical Features of Patients with Thrombotic Thrombocytopenic Purpura and Severe ADAMTS13 Deficiency
Journal of Clinical Apheresis 27:302–311 (2012) Ten Patient Stories Illustrating the Extraordinarily Diverse Clinical Features of Patients With Thrombotic Thrombocytopenic Purpura and Severe ADAMTS13 Deficiency James N. George,* Qiaofang Chen, Cassie C. Deford, and Zayd Al-Nouri Department of Biostatistics and Epidemiology, College of Public Health, Department of Medicine, College of Medicine, The University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma Patients with thrombotic thrombocytopenic purpura (TTP) and severe ADAMTS13 deficiency are often consid- ered to have typical clinical features. However, our experience is that there is extraordinary diversity of the pre- senting features and the clinical courses of these patients. This diversity is illustrated by descriptions of 10 patients. The patients illustrate that ADAMTS13 activity may be normal initially but severely deficient in subse- quent episodes. Patients with established diagnoses of systemic infection as the cause of their clinical features may have undetectable ADAMTS13 activity. Patients may have a prolonged prodrome of mild symptoms with only microangiopathic hemolytic anemia and thrombocytopenia or they may have the sudden onset of critical ill- ness with multiple organ involvement. Patients may die rapidly or recover rapidly; they may require minimal treatment or extensive and prolonged treatment. Patients may have acute and severe neurologic abnormalities before microangiopathic hemolytic anemia and thrombocytopenia occur. Patients may have concurrent TTP and systemic lupus erythematosus. Patients may have hereditary ADAMTS13 deficiency as the etiology of their TTP rather than acquired autoimmune ADAMTS13 deficiency. These patients’ stories illustrate the clinical spectrum of TTP with ADAMTS13 deficiency and emphasize the difficulties of clinical diagnosis. J. Clin. -

Modern Management of Traumatic Hemothorax
rauma & f T T o re l a t a m n r e u n o t J Mahoozi, et al., J Trauma Treat 2016, 5:3 Journal of Trauma & Treatment DOI: 10.4172/2167-1222.1000326 ISSN: 2167-1222 Review Article Open Access Modern Management of Traumatic Hemothorax Hamid Reza Mahoozi, Jan Volmerig and Erich Hecker* Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany *Corresponding author: Erich Hecker, Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany, Tel: 0232349892212; Fax: 0232349892229; E-mail: [email protected] Rec date: Jun 28, 2016; Acc date: Aug 17, 2016; Pub date: Aug 19, 2016 Copyright: © 2016 Mahoozi HR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Hemothorax is defined as a bleeding into pleural cavity. Hemothorax is a frequent manifestation of blunt chest trauma. Some authors suggested a hematocrit value more than 50% for differentiation of a hemothorax from a sanguineous pleural effusion. Hemothorax is also often associated with penetrating chest injury or chest wall blunt chest wall trauma with skeletal injury. Much less common, it may be related to pleural diseases, induced iatrogenic or develop spontaneously. In the vast majority of blunt and penetrating trauma cases, hemothoraces can be managed by relatively simple means in the course of care. Keywords: Traumatic hemothorax; Internal chest wall; Cardiac Hemodynamic response injury; Clinical manifestation; Blunt chest-wall injuries; Blunt As above mentioned the hemodynamic response is a multifactorial intrathoracic injuries; Penetrating thoracic trauma response and depends on severity of hemothorax according to its classification. -

Atrial Infarction
Cardiovascular and Metabolic Science Review Vol. 31 No. 1 January-March 2020 Atrial infarction: a literature review Infarto atrial: revisión de la literatura Laura Duque-González,* María José Orrego-Garay,‡ Laura Lopera-Mejía,§ Mauricio Duque-Ramírez|| Keywords: Infarction, atrium, ABSTRACT RESUMEN atrial fibrillation, embolism and Atrial infarction is an often-missed entity that has been El infarto atrial es una entidad frecuentemente olvidada, thrombosis. described in association with ventricular infarction ha sido descrita en asociación con el infarto ventricular or as an isolated disease, which is mainly caused by o de manera aislada y es causado principalmente Palabras clave: atherosclerosis. The electrocardiographic diagnostic por aterosclerosis. Los criterios diagnósticos Infarto, aurícula, criteria were proposed more than fifty years ago and electrocardiográficos fueron propuestos hace más de 50 fibrilación auricular, have not yet been validated. The diagnosis is based on años y aún no han sido validados. El diagnóstico se basa en embolia y trombosis. elevations and depressions of the PTa segment and changes el hallazgo de elevación o depresión del segmento PTa y de in the P wave morphology. However, supraventricular alteraciones en la morfología de la onda P; sin embargo, arrhythmias such as atrial fibrillation are the most common las arritmias supraventriculares como la fibrilación atrial finding and often predominate in the clinical presentation. son las más comunes y con frecuencia predominan en el Early recognition and treatment may prevent serious cuadro clínico. Un rápido reconocimiento y tratamiento complications such as mural thrombosis or atrial rupture. pueden ayudar a prevenir complicaciones graves como la Further studies need to be carried out in order to establish trombosis mural o la ruptura auricular. -

Pathophysiology of Atrial Fibrillation. Systemic Review
PRACA POGLĄDOWA/RevieW papeR Folia Cardiologica 2020 tom 15, nr 5, strony 349–354 DOI: 10.5603/FC.2020.0050 Copyright © 2020 Via Medica ISSN 2353–7752 Pathophysiology of atrial fibrillation. Systemic review Patofizjologia migotania przedsionków. Przegląd systemowy Andrzej Wysokiński, Sebastian Sawonik●iD , Katarzyna Wysokińska Department of Cardiology, Medical University of Lublin, Lublin, Poland Abstract Atrial fibrillation (AF) is an arrhythmia in which chaotic electrical signals are generated in the atria. AF can be classified as first episode AF, paroxysmal AF, persistent AF, long-standing persistent AF and permanent AF. Hence, AF is one of the biggest problems of contemporary health care (due to severe complications like thromboembolic disease and huge expenses associated with the treatment). The pathophysiology of the AF includes a triggered activity in the myocardium and also left atrial enlargement (LAE), and remodelling of the atria that may result in an interatrial block (IAB). IAB is prolonged conduction between the atria and is diagnosed in electrocardiography (ECG) when P-wave duration ≥ 110 ms. Other ECG changes coexisting with IAB, LAE and also remodelling of the atria are attributed to P-wave dispersion ≥ 40 ms, and a P-wave terminal force in V1 ≤ –0.04 mm/s. Remodelling of the atria leads to structural, cellular and hormonal changes. At the cellular scale — mitochondrial size and count are enlarged. A neurohormonal imbalance is also related to arrhythmia. An increased level of atrial natriuretic peptide, B-type natriuretic peptide, angiotensin II, transforming growth factor-β1 are observed in the case of cellular and ion channels changes. Atrial fibrillation is a significant problem posed to modern health care.