Florencio Zaragoza Dörwald Lead Optimization for Medicinal Chemists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
WADA Technical Letter – TL07 ANDARINE
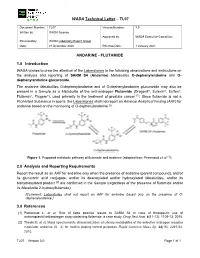
WADA Technical Letter – TL07 Document Number: TL07 Version Number: 3.0 Written by: WADA Science Approved by: WADA Executive Committee Reviewed by: WADA Laboratory Expert Group Date: 21 December 2020 Effective Date: 1 January 2021 ANDARINE - FLUTAMIDE 1.0 Introduction WADA wishes to draw the attention of the Laboratories to the following observations and instructions on the analysis and reporting of SARM S4 (Andarine) Metabolites O-dephenylandarine and O- dephenylandarine glucuronide. The andarine Metabolites O-dephenylandarine and of O-dephenylandarine glucuronide may also be present in a Sample as a Metabolite of the anti-androgen Flutamide (Drogenil®, Eulexin®, Euflex®, Flutamin®, Flugere®), used primarily in the treatment of prostate cancer [1]. Since flutamide is not a Prohibited Substance in sports, the Laboratories shall not report an Adverse Analytical Finding (AAF) for andarine based on the monitoring of O-dephenylandarine [2]. Figure 1. Proposed metabolic pathway of flutamide and andarine (adapted from Perrenoud et al. [1]). 2.0 Analysis and Reporting Requirements Report the result as an AAF for andarine only when the presence of andarine (parent compound), and/or its glucuronic acid conjugate, and/or its deacetylated and/or hydroxylated Metabolites, and/or its bishydroxylated product [2] are confirmed in the Sample (regardless of the presence of flutamide and/or its Metabolite 2-hydroxyflutamide); [Comment: Laboratories shall not report an AAF for andarine based only on the presence of O- dephenylandarine.] 3.0 References [1] Perrenoud L. et al. Risk of false positive results to SARM S4 in case of therapeutic use of antineoplastic/antiandrogen drug containing flutamide: a case study. -

(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
USOO9498481 B2 (12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao et al. (45) Date of Patent: *Nov. 22, 2016 (54) CYCLOPROPYL MODULATORS OF P2Y12 WO WO95/26325 10, 1995 RECEPTOR WO WO99/O5142 2, 1999 WO WOOO/34283 6, 2000 WO WO O1/92262 12/2001 (71) Applicant: Apharaceuticals. Inc., La WO WO O1/922.63 12/2001 olla, CA (US) WO WO 2011/O17108 2, 2011 (72) Inventors: Tadimeti Rao, San Diego, CA (US); Chengzhi Zhang, San Diego, CA (US) OTHER PUBLICATIONS Drugs of the Future 32(10), 845-853 (2007).* (73) Assignee: Auspex Pharmaceuticals, Inc., LaJolla, Tantry et al. in Expert Opin. Invest. Drugs (2007) 16(2):225-229.* CA (US) Wallentin et al. in the New England Journal of Medicine, 361 (11), 1045-1057 (2009).* (*) Notice: Subject to any disclaimer, the term of this Husted et al. in The European Heart Journal 27, 1038-1047 (2006).* patent is extended or adjusted under 35 Auspex in www.businesswire.com/news/home/20081023005201/ U.S.C. 154(b) by Od en/Auspex-Pharmaceuticals-Announces-Positive-Results-Clinical M YW- (b) by ayS. Study (published: Oct. 23, 2008).* This patent is Subject to a terminal dis- Concert In www.concertpharma. com/news/ claimer ConcertPresentsPreclinicalResultsNAMS.htm (published: Sep. 25. 2008).* Concert2 in Expert Rev. Anti Infect. Ther. 6(6), 782 (2008).* (21) Appl. No.: 14/977,056 Springthorpe et al. in Bioorganic & Medicinal Chemistry Letters 17. 6013-6018 (2007).* (22) Filed: Dec. 21, 2015 Leis et al. in Current Organic Chemistry 2, 131-144 (1998).* Angiolillo et al., Pharmacology of emerging novel platelet inhibi (65) Prior Publication Data tors, American Heart Journal, 2008, 156(2) Supp. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

Genetically Modified Baculoviruses for Pest
INSECT CONTROL BIOLOGICAL AND SYNTHETIC AGENTS This page intentionally left blank INSECT CONTROL BIOLOGICAL AND SYNTHETIC AGENTS EDITED BY LAWRENCE I. GILBERT SARJEET S. GILL Amsterdam • Boston • Heidelberg • London • New York • Oxford Paris • San Diego • San Francisco • Singapore • Sydney • Tokyo Academic Press is an imprint of Elsevier Academic Press, 32 Jamestown Road, London, NW1 7BU, UK 30 Corporate Drive, Suite 400, Burlington, MA 01803, USA 525 B Street, Suite 1800, San Diego, CA 92101-4495, USA ª 2010 Elsevier B.V. All rights reserved The chapters first appeared in Comprehensive Molecular Insect Science, edited by Lawrence I. Gilbert, Kostas Iatrou, and Sarjeet S. Gill (Elsevier, B.V. 2005). All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. Permissions may be sought directly from Elsevier’s Rights Department in Oxford, UK: phone (þ44) 1865 843830, fax (þ44) 1865 853333, e-mail [email protected]. Requests may also be completed on-line via the homepage (http://www.elsevier.com/locate/permissions). Library of Congress Cataloging-in-Publication Data Insect control : biological and synthetic agents / editors-in-chief: Lawrence I. Gilbert, Sarjeet S. Gill. – 1st ed. p. cm. Includes bibliographical references and index. ISBN 978-0-12-381449-4 (alk. paper) 1. Insect pests–Control. 2. Insecticides. I. Gilbert, Lawrence I. (Lawrence Irwin), 1929- II. Gill, Sarjeet S. SB931.I42 2010 632’.7–dc22 2010010547 A catalogue record for this book is available from the British Library ISBN 978-0-12-381449-4 Cover Images: (Top Left) Important pest insect targeted by neonicotinoid insecticides: Sweet-potato whitefly, Bemisia tabaci; (Top Right) Control (bottom) and tebufenozide intoxicated by ingestion (top) larvae of the white tussock moth, from Chapter 4; (Bottom) Mode of action of Cry1A toxins, from Addendum A7. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

A Randomized Double-Blind, Double-Dummy
pISSN 1598-2998, eISSN 2005-9256 Cancer Res Treat. 2014;46(1):19-26 http://dx.doi.org/10.4143/crt.2014.46.1.19 Original Article Open Access A Randomized Double-Blind, Double-Dummy, Multicenter Trial of Azasetron versus Ondansetron to Evaluate Efficacy and Safety in the Prevention of Delayed Nausea and Vomiting Induced by Chemotherapy Hee Yeon Lee, MD 1 Purpose Hoon-Kyo Kim, MD 1 This study was conducted to evaluate the efficacy and safety of azasetron compared Kyung Hee Lee, MD 2 to ondansetron in the prevention of delayed chemotherapy-induced nausea and Bong-Seog Kim, MD 3 vomiting. MD 4 Hong Suk Song, Materials and Methods MD 5 Sung Hyun Yang, This study was a multi-center, prospective, randomized, double-dummy, double-blind MD 6 Joon Hee Kim, and parallel-group trial involving 12 institutions in Korea between May 2005 and MD 7 Yeul Hong Kim, December 2005. A total of 265 patients with moderately and highly emetogenic MD 8 Jong Gwang Kim, chemotherapy were included and randomly assigned to either the azasetron or MD 9 Sang-We Kim, ondansetron group. All patients received azasetron (10 mg intravenously) and MD 10 Dong-Wan Kim, dexamethasone (20 mg intravenously) on day 1 and dexamethasone (4 mg orally every MD 11 Si-Young Kim, 12 hours) on days 2-4. The azasetron group received azasetron (10 mg orally) with MD 12 Hee Sook Park, placebo of ondansetron (orally every 12 hours), and the ondansetron group received Department of Internal Medicine, ondansetron (8 mg orally every 12 hours) with placebo of azasetron (orally) on days 1St. -

Part I Biopharmaceuticals
1 Part I Biopharmaceuticals Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 3 1 Analogs and Antagonists of Male Sex Hormones Robert W. Brueggemeier The Ohio State University, Division of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, Columbus, Ohio 43210, USA 1Introduction6 2 Historical 6 3 Endogenous Male Sex Hormones 7 3.1 Occurrence and Physiological Roles 7 3.2 Biosynthesis 8 3.3 Absorption and Distribution 12 3.4 Metabolism 13 3.4.1 Reductive Metabolism 14 3.4.2 Oxidative Metabolism 17 3.5 Mechanism of Action 19 4 Synthetic Androgens 24 4.1 Current Drugs on the Market 24 4.2 Therapeutic Uses and Bioassays 25 4.3 Structure–Activity Relationships for Steroidal Androgens 26 4.3.1 Early Modifications 26 4.3.2 Methylated Derivatives 26 4.3.3 Ester Derivatives 27 4.3.4 Halo Derivatives 27 4.3.5 Other Androgen Derivatives 28 4.3.6 Summary of Structure–Activity Relationships of Steroidal Androgens 28 4.4 Nonsteroidal Androgens, Selective Androgen Receptor Modulators (SARMs) 30 4.5 Absorption, Distribution, and Metabolism 31 4.6 Toxicities 32 Translational Medicine: Molecular Pharmacology and Drug Discovery First Edition. Edited by Robert A. Meyers. © 2018 Wiley-VCH Verlag GmbH & Co. KGaA. Published 2018 by Wiley-VCH Verlag GmbH & Co. KGaA. 4 Analogs and Antagonists of Male Sex Hormones 5 Anabolic Agents 32 5.1 Current Drugs on the Market 32 5.2 Therapeutic Uses and Bioassays -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

Stems for Nonproprietary Drug Names
USAN STEM LIST STEM DEFINITION EXAMPLES -abine (see -arabine, -citabine) -ac anti-inflammatory agents (acetic acid derivatives) bromfenac dexpemedolac -acetam (see -racetam) -adol or analgesics (mixed opiate receptor agonists/ tazadolene -adol- antagonists) spiradolene levonantradol -adox antibacterials (quinoline dioxide derivatives) carbadox -afenone antiarrhythmics (propafenone derivatives) alprafenone diprafenonex -afil PDE5 inhibitors tadalafil -aj- antiarrhythmics (ajmaline derivatives) lorajmine -aldrate antacid aluminum salts magaldrate -algron alpha1 - and alpha2 - adrenoreceptor agonists dabuzalgron -alol combined alpha and beta blockers labetalol medroxalol -amidis antimyloidotics tafamidis -amivir (see -vir) -ampa ionotropic non-NMDA glutamate receptors (AMPA and/or KA receptors) subgroup: -ampanel antagonists becampanel -ampator modulators forampator -anib angiogenesis inhibitors pegaptanib cediranib 1 subgroup: -siranib siRNA bevasiranib -andr- androgens nandrolone -anserin serotonin 5-HT2 receptor antagonists altanserin tropanserin adatanserin -antel anthelmintics (undefined group) carbantel subgroup: -quantel 2-deoxoparaherquamide A derivatives derquantel -antrone antineoplastics; anthraquinone derivatives pixantrone -apsel P-selectin antagonists torapsel -arabine antineoplastics (arabinofuranosyl derivatives) fazarabine fludarabine aril-, -aril, -aril- antiviral (arildone derivatives) pleconaril arildone fosarilate -arit antirheumatics (lobenzarit type) lobenzarit clobuzarit -arol anticoagulants (dicumarol type) dicumarol -

Formulary (List of Covered Drugs)
3ODQ<HDU 202 Formulary (List of Covered Drugs) PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THE FOLLOWING PLAN: $0 Cost Share AI/AN HMO Minimum Coverage HMO Silver 70 HMO Active Choice PPO Silver Opal 25 Gold HMO Silver 70 OFF Exchange HMO Amber 50 HMO Silver Opal 50 Silver HMO Silver 73 HMO Bronze 60 HDHP HMO Platinum 90 HMO Silver 87 HMO Bronze 60 HMO Ruby 10 Platinum HMO Silver 94 HMO Gold 80 HMO Ruby 20 Platinum HMO Jade 15 HMO Ruby 40 Platinum HMO This formulary was last updated on8//20. This formulary is VXEMHFWto change and all previous versions of the formulary no longer apply. For more recent information or other questions, please contact Chinese Community Health Plan Member Services at 1-888-775-7888 or, for TTY users, 1-877-681-8898, seven days a week from 8:00 a.m. to 8:00 p.m., or visit www.cchphealthplan.com/family-member -,-ϭ -,-ϭ"&* !#" + 5 5 ),-$+" %(%'.')/"+#" %&/"+ -%/"$)% "%&/"+ *& )&! %&/"+ 0 $(#" '"+ %&/"+ *& %&/"+ %&/"+ +)(2" &-%(.' %&/"+ +)(2" .1&-%(.' %&/"+ )&! .1&-%(.' !" .1&-%(.' dŚŝƐĨŽƌŵƵůĂƌLJǁĂƐůĂƐƚƵƉĚĂƚĞĚ8ͬϭͬϮϬϮϭ͘dŚŝƐĨŽƌŵƵůĂƌLJŝƐƐƵďũĞĐƚƚŽ ĐŚĂŶŐĞĂŶĚĂůůƉƌĞǀŝŽƵƐǀĞƌƐŝŽŶƐŽĨƚŚĞĨŽƌŵƵůĂƌLJŶŽůŽŶŐĞƌĂƉƉůLJ͘&ŽƌŵŽƌĞ ƌĞĐĞŶƚŝŶĨŽƌŵĂƚŝŽŶŽƌŽƚŚĞƌƋƵĞƐƚŝŽŶƐ͕ƉůĞĂƐĞĐŽŶƚĂĐƚŚŝŶĞƐĞŽŵŵƵŶŝƚLJ ,ĞĂůƚŚWůĂŶDĞŵďĞƌ^ĞƌǀŝĐĞƐĂƚϭͲϴϴϴͲϳϳϱͲϳϴϴϴŽƌ͕ĨŽƌddzƵƐĞƌƐ͕ ϭͲϴϳϳͲϲϴϭͲϴϴϵϴ͕ƐĞǀĞŶĚĂLJƐĂǁĞĞŬĨƌŽŵϴ͗ϬϬĂ͘ŵ͘ƚŽϴ͗ϬϬƉ͘ŵ͕͘ŽƌǀŝƐŝƚ ǁǁǁ͘ĐĐŚƉŚĞĂůƚŚƉůĂŶ͘ĐŽŵͬĨĂŵŝůLJͲŵĞŵďĞƌ !! %+)&,+ &%+&+&)$,#)0),# *+666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I % + &%*6666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666I -

Development and Validation of a LC-MS/MS Method for Detection and Quantification of 18 Antidepressants in Whole Blood
City University of New York (CUNY) CUNY Academic Works Student Theses John Jay College of Criminal Justice Spring 6-2019 Development and validation of a LC-MS/MS method for detection and quantification of 18 antidepressants in whole blood Linda Kim CUNY John Jay College, [email protected] How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/jj_etds/106 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Development and validation of a LC-MS/MS method for detection and quantification of 18 antidepressants in whole blood A Thesis Presented in Partial Fulfillment of the Requirements for the Degree of Master of Science in Forensic Science, John Jay College of Criminal Justice, City University of New York Linda Kim May 2019 Development and validation of a LC-MS/MS method for detection and quantification of 18 antidepressants in whole blood Linda Kim This Thesis has been presented to and accepted by the Office of Graduate Studies, John Jay College of Criminal Justice in Partial Fulfillment of the Requirements for the Degree of Master of Science in Forensic Science. Thesis Committee Thesis Advisor: Marta Concheiro-Guisan Second Reader: Shu-Yuan Cheng External Reader: Damon Borg i Acknowledgement I would like to thank Dr. Stripp for providing his laboratory for my research, and Dr. Borg and everyone in Cordant Laboratory for their guidance and support. I would like to thank Dr. Concheiro-Guisan for her time, patience, and information, and for making it possible to successfully complete this thesis.