Medication Overdoses in the Emergency Department: Oral Hypoglycemic Agents, Atypical Antipsychotic Agents, Beta- Blockers, Calcium Channel Blockers, and Digoxin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

The Pharmacology of Amiodarone and Digoxin As Antiarrhythmic Agents
Part I Anaesthesia Refresher Course – 2017 University of Cape Town The Pharmacology of Amiodarone and Digoxin as Antiarrhythmic Agents Dr Adri Vorster UCT Department of Anaesthesia & Perioperative Medicine The heart contains pacemaker, conduction and contractile tissue. Cardiac arrhythmias are caused by either enhancement or depression of cardiac action potential generation by pacemaker cells, or by abnormal conduction of the action potential. The pharmacological treatment of arrhythmias aims to achieve restoration of a normal rhythm and rate. The resting membrane potential of myocytes is around -90 mV, with the inside of the membrane more negative than the outside. The main extracellular ions are Na+ and Cl−, with K+ the main intracellular ion. The cardiac action potential involves a change in voltage across the cell membrane of myocytes, caused by movement of charged ions across the membrane. This voltage change is triggered by pacemaker cells. The action potential is divided into 5 phases (figure 1). Phase 0: Rapid depolarisation Duration < 2ms Threshold potential must be reached (-70 mV) for propagation to occur Rapid positive charge achieved as a result of increased Na+ conductance through voltage-gated Na+ channels in the cell membrane Phase 1: Partial repolarisation Closure of Na+ channels K+ channels open and close, resulting in brief outflow of K+ and a more negative membrane potential Phase 2: Plateau Duration up to 150 ms Absolute refractory period – prevents further depolarisation and myocardial tetany Result of Ca++ influx -

Dabigatran Amoxicillin Clavulanate IV Treatment in the Community
BEST PRACTICE 38 SEPTEMBER 2011 Dabigatran Amoxicillin clavulanate bpac nz IV treatment in the community better medicin e Editor-in-chief We would like to acknowledge the following people for Professor Murray Tilyard their guidance and expertise in developing this edition: Professor Carl Burgess, Wellington Editor Dr Gerry Devlin, Hamilton Rebecca Harris Dr John Fink, Christchurch Dr Lisa Houghton, Dunedin Programme Development Dr Rosemary Ikram, Christchurch Mark Caswell Dr Sisira Jayathissa, Wellington Rachael Clarke Kate Laidlow, Rotorua Peter Ellison Dr Hywel Lloyd, GP Reviewer, Dunedin Julie Knight Associate Professor Stewart Mann, Wellington Noni Richards Dr Richard Medlicott, Wellington Dr AnneMarie Tangney Dr Alan Panting, Nelson Dr Sharyn Willis Dr Helen Patterson, Dunedin Dave Woods David Rankin, Wellington Report Development Dr Ralph Stewart, Auckland Justine Broadley Dr Neil Whittaker, GP Reviewer, Nelson Tim Powell Dr Howard Wilson, Akaroa Design Michael Crawford Best Practice Journal (BPJ) ISSN 1177-5645 Web BPJ, Issue 38, September 2011 Gordon Smith BPJ is published and owned by bpacnz Ltd Management and Administration Level 8, 10 George Street, Dunedin, New Zealand. Jaala Baldwin Bpacnz Ltd is an independent organisation that promotes health Kaye Baldwin care interventions which meet patients’ needs and are evidence Tony Fraser based, cost effective and suitable for the New Zealand context. Kyla Letman We develop and distribute evidence based resources which describe, facilitate and help overcome the barriers to best Clinical Advisory Group practice. Clive Cannons nz Michele Cray Bpac Ltd is currently funded through contracts with PHARMAC and DHBNZ. Margaret Gibbs nz Dr Rosemary Ikram Bpac Ltd has five shareholders: Procare Health, South Link Health, General Practice NZ, the University of Otago and Pegasus Dr Cam Kyle Health. -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

The Genetics of Adverse Drug Outcomes in Type 2 Diabetes: a Systematic Review
SYSTEMATIC REVIEW published: 14 June 2021 doi: 10.3389/fgene.2021.675053 The Genetics of Adverse Drug Outcomes in Type 2 Diabetes: A Systematic Review Assefa M. Baye 1, Teferi G. Fanta 1, Moneeza K. Siddiqui 2 and Adem Y. Dawed 2* 1 Department of Pharmacology and Clinical Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia, 2 Division of Population Health and Genomics, Ninewells Hospital and School of Medicine, University of Dundee, Dundee, United Kingdom Background: Adverse drug reactions (ADR) are a major clinical problem accounting for significant hospital admission rates, morbidity, mortality, and health care costs. One-third of people with diabetes experience at least one ADR. However, there is notable interindividual heterogeneity resulting in patient harm and unnecessary medical costs. Genomics is at the forefront of research to understand interindividual variability, and there are many genotype-drug response associations in diabetes with inconsistent findings. Here, we conducted a systematic review to comprehensively examine and synthesize the effect of genetic polymorphisms on the incidence of ADRs of oral glucose-lowering drugs in people with type 2 diabetes. Edited by: Celine Verstuyft, Methods: A literature search was made to identify articles that included specific Université Paris-Saclay, France results of research on genetic polymorphism and adverse effects associated with Reviewed by: oral glucose-lowering drugs. The electronic search was carried out on 3rd October Zhiguo Xie, 2020, through Cochrane Library, PubMed, and Web of Science using keywords and Central South University, China Vera Ribeiro, MeSH terms. University of Algarve, Portugal Result: Eighteen articles consisting of 10, 383 subjects were included in this review. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

Spectrum of Digoxin-Induced Ocular Toxicity: a Case Report and Literature Review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E
Renard et al. BMC Res Notes (2015) 8:368 DOI 10.1186/s13104-015-1367-6 CASE REPORT Open Access Spectrum of digoxin-induced ocular toxicity: a case report and literature review Delphine Renard1*, Eve Rubli2, Nathalie Voide3, François‑Xavier Borruat3 and Laura E. Rothuizen1 Abstract Background: Digoxin intoxication results in predominantly digestive, cardiac and neurological symptoms. This case is outstanding in that the intoxication occurred in a nonagenarian and induced severe, extensively documented visual symptoms as well as dysphagia and proprioceptive illusions. Moreover, it went undiagnosed for a whole month despite close medical follow-up, illustrating the difficulty in recognizing drug-induced effects in a polymorbid patient. Case presentation: Digoxin 0.25 mg qd for atrial fibrillation was prescribed to a 91-year-old woman with an esti‑ mated creatinine clearance of 18 ml/min. Over the following 2–3 weeks she developed nausea, vomiting and dyspha‑ gia, snowy and blurry vision, photopsia, dyschromatopsia, aggravated pre-existing formed visual hallucinations and proprioceptive illusions. She saw her family doctor twice and visited the eye clinic once until, 1 month after starting digoxin, she was admitted to the emergency room. Intoxication was confirmed by a serum digoxin level of 5.7 ng/ml (reference range 0.8–2 ng/ml). After stopping digoxin, general symptoms resolved in a few days, but visual complaints persisted. Examination by the ophthalmologist revealed decreased visual acuity in both eyes, 4/10 in the right eye (OD) and 5/10 in the left eye (OS), decreased color vision as demonstrated by a score of 1/13 in both eyes (OU) on Ishihara pseudoisochromatic plates, OS cataract, and dry age-related macular degeneration (ARMD). -

Sulfonylureas
Therapeutic Class Overview Sulfonylureas INTRODUCTION In the United States (US), diabetes mellitus affects more than 30 million people and is the 7th leading cause of death (Centers for Disease Control and Prevention [CDC] 2018). Type 2 diabetes mellitus (T2DM) is the most common form of diabetes and is characterized by elevated fasting and postprandial glucose concentrations (American Diabetes Association [ADA] 2019[a]). It is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications (ADA 2019[b]). ○ Complications of T2DM include hypertension, heart disease, stroke, vision loss, nephropathy, and neuropathy (ADA 2019[a]). In addition to dietary and lifestyle management, T2DM can be treated with insulin, one or more oral medications, or a combination of both. Many patients with T2DM will require combination therapy (Garber et al 2019). Classes of oral medications for the management of blood glucose levels in patients with T2DM focus on increasing insulin secretion, increasing insulin responsiveness, or both, decreasing the rate of carbohydrate absorption, decreasing the rate of hepatic glucose production, decreasing the rate of glucagon secretion, and blocking glucose reabsorption by the kidney (Garber et al 2019). Pharmacologic options for T2DM include sulfonylureas (SFUs), biguanides, thiazolidinediones (TZDs), meglitinides, alpha-glucosidase inhibitors, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) analogs, amylinomimetics, sodium-glucose cotransporter 2 (SGLT2) inhibitors, combination products, and insulin (Garber et al 2019). SFUs are the oldest of the oral antidiabetic medications, and all agents are available generically. The SFUs can be divided into 2 categories: first-generation and second-generation. -
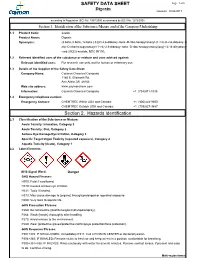
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented.