Short-Term Efficacy and Safety of Repaglinide Versus Glimepiride As
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optum Essential Health Benefits Enhanced Formulary PDL January
PENICILLINS ketorolac tromethamineQL GENERIC mefenamic acid amoxicillin/clavulanate potassium nabumetone amoxicillin/clavulanate potassium ER naproxen January 2016 ampicillin naproxen sodium ampicillin sodium naproxen sodium CR ESSENTIAL HEALTH BENEFITS ampicillin-sulbactam naproxen sodium ER ENHANCED PREFERRED DRUG LIST nafcillin sodium naproxen DR The Optum Preferred Drug List is a guide identifying oxacillin sodium oxaprozin preferred brand-name medicines within select penicillin G potassium piroxicam therapeutic categories. The Preferred Drug List may piperacillin sodium/ tazobactam sulindac not include all drugs covered by your prescription sodium tolmetin sodium drug benefit. Generic medicines are available within many of the therapeutic categories listed, in addition piperacillin sodium/tazobactam Fenoprofen Calcium sodium to categories not listed, and should be considered Meclofenamate Sodium piperacillin/tazobactam as the first line of prescribing. Tolmetin Sodium Amoxicillin/Clavulanate Potassium LOW COST GENERIC PREFERRED For benefit coverage or restrictions please check indomethacin your benefit plan document(s). This listing is revised Augmentin meloxicam periodically as new drugs and new prescribing LOW COST GENERIC naproxen kit information becomes available. It is recommended amoxicillin that you bring this list of medications when you or a dicloxacillin sodium CARDIOVASCULAR covered family member sees a physician or other penicillin v potassium ACE-INHIBITORS healthcare provider. GENERIC QUINOLONES captopril ANTI-INFECTIVES -

The Genetics of Adverse Drug Outcomes in Type 2 Diabetes: a Systematic Review
SYSTEMATIC REVIEW published: 14 June 2021 doi: 10.3389/fgene.2021.675053 The Genetics of Adverse Drug Outcomes in Type 2 Diabetes: A Systematic Review Assefa M. Baye 1, Teferi G. Fanta 1, Moneeza K. Siddiqui 2 and Adem Y. Dawed 2* 1 Department of Pharmacology and Clinical Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia, 2 Division of Population Health and Genomics, Ninewells Hospital and School of Medicine, University of Dundee, Dundee, United Kingdom Background: Adverse drug reactions (ADR) are a major clinical problem accounting for significant hospital admission rates, morbidity, mortality, and health care costs. One-third of people with diabetes experience at least one ADR. However, there is notable interindividual heterogeneity resulting in patient harm and unnecessary medical costs. Genomics is at the forefront of research to understand interindividual variability, and there are many genotype-drug response associations in diabetes with inconsistent findings. Here, we conducted a systematic review to comprehensively examine and synthesize the effect of genetic polymorphisms on the incidence of ADRs of oral glucose-lowering drugs in people with type 2 diabetes. Edited by: Celine Verstuyft, Methods: A literature search was made to identify articles that included specific Université Paris-Saclay, France results of research on genetic polymorphism and adverse effects associated with Reviewed by: oral glucose-lowering drugs. The electronic search was carried out on 3rd October Zhiguo Xie, 2020, through Cochrane Library, PubMed, and Web of Science using keywords and Central South University, China Vera Ribeiro, MeSH terms. University of Algarve, Portugal Result: Eighteen articles consisting of 10, 383 subjects were included in this review. -

Sulfonylureas
Therapeutic Class Overview Sulfonylureas INTRODUCTION In the United States (US), diabetes mellitus affects more than 30 million people and is the 7th leading cause of death (Centers for Disease Control and Prevention [CDC] 2018). Type 2 diabetes mellitus (T2DM) is the most common form of diabetes and is characterized by elevated fasting and postprandial glucose concentrations (American Diabetes Association [ADA] 2019[a]). It is a chronic illness that requires continuing medical care and ongoing patient self-management education and support to prevent acute complications and to reduce the risk of long-term complications (ADA 2019[b]). ○ Complications of T2DM include hypertension, heart disease, stroke, vision loss, nephropathy, and neuropathy (ADA 2019[a]). In addition to dietary and lifestyle management, T2DM can be treated with insulin, one or more oral medications, or a combination of both. Many patients with T2DM will require combination therapy (Garber et al 2019). Classes of oral medications for the management of blood glucose levels in patients with T2DM focus on increasing insulin secretion, increasing insulin responsiveness, or both, decreasing the rate of carbohydrate absorption, decreasing the rate of hepatic glucose production, decreasing the rate of glucagon secretion, and blocking glucose reabsorption by the kidney (Garber et al 2019). Pharmacologic options for T2DM include sulfonylureas (SFUs), biguanides, thiazolidinediones (TZDs), meglitinides, alpha-glucosidase inhibitors, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) analogs, amylinomimetics, sodium-glucose cotransporter 2 (SGLT2) inhibitors, combination products, and insulin (Garber et al 2019). SFUs are the oldest of the oral antidiabetic medications, and all agents are available generically. The SFUs can be divided into 2 categories: first-generation and second-generation. -

Comparison of Glimepiride, Alogliptin and Alogliptin+Pioglitazone Combination in Poorly Controlled Type 2 Diabetic Patients ( Protocol: Takeda ALO-IIT)
Takeda_ALO-IIT_Ver 3.3 date: 29/Dec/2016 Comparison of glimepiride, alogliptin and alogliptin+pioglitazone combination in poorly controlled type 2 diabetic patients ( Protocol: Takeda_ALO-IIT) Version No: 3.3 date:29/Dec/2016 Principal Investigator’s Affiliation: Seoul National University Bundang Hospital 1 Takeda_ALO-IIT_Ver 3.3 date: 29/Dec/2016 Principal Investigator’s Name: Sung Hee Choi Research Outline Comparison of glimepiride, alogliptin and alogliptin+pioglitazone combination in Title of Research poorly controlled type 2 diabetic patients Principal Investigator Professor Sung Hee Choi Institution Supporting Takeda Pharmaceuticals Korea Co. Ltd. Research Expenses The primary objective is to compare the change in HbA1c in week 24 in 3 treatment groups: the glimepiride monotherapy treatment group; the alogliptin monotherapy treatment group; the alogliptin - pioglitazone combination therapy treatment group. - The secondary objective is to compare the change in HbA1c in week 12 and fasting plasma glucose (FPG) in week 12 and 24 in the following 3 treatment groups over the course of 3 months (at the Baseline, in Week 12): (the glimepiride Research Objective monotherapy treatment group, the alogliptin monotherapy treatment group, and the alogliptin - pioglitazone combination therapy treatment group). - Also, the change in parameters of glycemic variability assessed by CGM will be investigated. - Also, for a 6-month period, the average change in the lipid profile will be compared (Baseline, Week 12, Week 24). · This trial is a three-armed, open label, random assignment trial. · The research subjects are patients who are first starting their treatment or patients who have failed with the metformin treatment and are changing their medication. -

AVANDARYL™ (Rosiglitazone Maleate and Glimepiride) Tablets
AA:LX PRESCRIBING INFORMATION AVANDARYL™ (rosiglitazone maleate and glimepiride) Tablets DESCRIPTION AVANDARYL (rosiglitazone maleate and glimepiride) tablets contain 2 oral antidiabetic drugs used in the management of type 2 diabetes: Rosiglitazone maleate and glimepiride. Rosiglitazone maleate is an oral antidiabetic agent of the thiazolidinedione class which acts primarily by increasing insulin sensitivity. Rosiglitazone maleate is not chemically or functionally related to the sulfonylureas, the biguanides, or the alpha-glucosidase inhibitors. Chemically, rosiglitazone maleate is (±)-5-[[4-[2-(methyl-2-pyridinylamino) ethoxy]phenyl] methyl]-2,4-thiazolidinedione, (Z)-2-butenedioate (1:1) with a molecular weight of 473.52 (357.44 free base). The molecule has a single chiral center and is present as a racemate. Due to rapid interconversion, the enantiomers are functionally indistinguishable. The molecular formula is C18H19N3O3S•C4H4O4. Rosiglitazone maleate is a white to off-white solid with a melting point range of 122° to 123°C. The pKa values of rosiglitazone maleate are 6.8 and 6.1. It is readily soluble in ethanol and a buffered aqueous solution with pH of 2.3; solubility decreases with increasing pH in the physiological range. The structural formula of rosiglitazone maleate is: Glimepiride is an oral antidiabetic drug of the sulfonylurea class. Glimepiride is a white to yellowish-white, crystalline, odorless to practically odorless powder. Chemically, glimepiride is 1-[[p-[2-(3-ethyl-4-methyl-2-oxo-3-pyrroline-1-carboxamido)ethyl]phenyl]sulfonyl]-3-(trans-4- methylcyclohexyl)urea with a molecular weight of 490.62. The molecular formula for glimepiride is C24H34N4O5S. Glimepiride is practically insoluble in water. -

Effect of Sulfonylureas Administered Centrally on the Blood Glucose Level in Immobilization Stress Model
Korean J Physiol Pharmacol Vol 19: 197-202, May, 2015 pISSN 1226-4512 http://dx.doi.org/10.4196/kjpp.2015.19.3.197 eISSN 2093-3827 Effect of Sulfonylureas Administered Centrally on the Blood Glucose Level in Immobilization Stress Model Naveen Sharma1, Yun-Beom Sim1, Soo-Hyun Park1, Su-Min Lim1, Sung-Su Kim1, Jun-Sub Jung1, Jae-Seung Hong2, and Hong-Won Suh1 1Department of Pharmacology, Institute of Natural Medicine, 2Department of Physical Education, College of Natural Medicine, College of Medicine, Hallym University, Chuncheon 200-702, Korea Sulfonylureas are widely used as an antidiabetic drug. In the present study, the effects of sul- fonylurea administered supraspinally on immobilization stress-induced blood glucose level were studied in ICR mice. Mice were once enforced into immobilization stress for 30 min and returned to the cage. The blood glucose level was measured 30, 60, and 120 min after immobilization stress initiation. W e found that intracerebroventricular (i.c.v.) injection with 30 μ g of glyburide, glipizide, glimepiride or tolazamide attenuated the increased blood glucose level induced by immobilization stress. Immo- bilization stress causes an elevation of the blood corticosterone and insulin levels. Sulfonylureas pre- treated i.c.v. caused a further elevation of the blood corticosterone level when mice were forced into the stress. In addition, sulfonylureas pretreated i.c.v. alone caused an elevation of the plasma insulin level. Furthermore, immobilization stress-induced insulin level was reduced by i.c.v. pretreated sulfonylureas. Our results suggest that lowering effect of sulfonylureas administered supraspinally against immobilization stress-induced increase of the blood glucose level appears to be primarily mediated via elevation of the plasma insulin level. -
Glimepiride Market UK-IE Language English Size 170 X 550 Mm (PIL) Min
Artwork No. - Colours Used Customer Accord Pantone Black Description Glimepiride Market UK-IE Language English Size 170 x 550 mm (PIL) Min. Font Size 9 Version No. 10 (Page 1 of 2) (IB026) Date 25/07/14 (Glimepiride (ACC-UK-IE)NEW-IB026-VAR-PIL) Prepared By Checked By Approved By Regulatory Affairs Regulatory Affairs Quality Assurance You should therefore always take some form of • have frequent episodes of hypoglycaemia • Feeling or being sick, diarrhoea, feeling full or sugar with you (e.g. sugar cubes). Remember • have fewer or no warning signals of bloated, and abdominal pain that artificial sweeteners are not effective. Please hypoglycaemia • Decrease in the amount of sodium level in your Package leaflet: Information for the user contact your doctor or go to the hospital if taking blood (shown by blood tests) sugar does not help or if the symptoms recur. Glimepiride Tablets contains lactose Glimepiride 1 mg Tablets If you have been told by your doctor that you Not known (frequency cannot be estimated Glimepiride 2 mg Tablets Laboratory Tests cannot tolerate some sugars, contact your doctor from the available data) The level of sugar in your blood or urine should before taking this medicinal product. • Allergy (hypersensitivity) of the skin may occur Glimepiride 3 mg Tablets be checked regularly. Your doctor may also take such as itching, rash, hives and increased blood tests to monitor your blood cell levels and sensitivity to sun. Some mild allergic reactions Glimepiride 4 mg Tablets liver function. 3. How to take Glimepiride Tablets may develop into serious reactions with Glimepiride swallowing or breathing problems, swelling of Always take this medicine exactly as described in your lips, throat or tongue. -

AMARYL® Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION • Potential Increased Risk of Cardiovascular Mortality with Sulfonylureas: These highlights do not include all the information needed to use Inform patient of risks, benefits and treatment alternatives (5.4). AMARYL® safely and effectively. See full prescribing information for • Macrovascular Outcomes: No clinical studies establishing conclusive AMARYL. evidence of macrovascular risk reduction with AMARYL or any other anti-diabetic drug (5.5). AMARYL (glimepiride) tablets Initial U.S. Approval: 1995 ------------------------------ADVERSE REACTIONS--------------------------- Common adverse reactions in clinical trials (≥5% and more common than ---------------------------INDICATIONS AND USAGE------------------------ with placebo) include hypoglycemia, headache, nausea, and dizziness (6.1). AMARYL is a sulfonylurea indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (1.1). To report SUSPECTED ADVERSE REACTIONS, contact sanofi-aventis U.S. LLC at 1-800-633-1610 or FDA at 1-800-FDA-1088 or Important Limitations of Use: www.fda.gov/medwatch. • Not for treating type 1 diabetes mellitus or diabetic ketoacidosis (1.1). ------------------------------DRUG INTERACTIONS--------------------------- ----------------------DOSAGE AND ADMINISTRATION-------------------- • Certain medications may affect glucose metabolism, requiring AMARYL • Recommended starting dose is 1 or 2 mg once daily. Increase in 1 or 2 mg dose adjustment and close monitoring of blood -

GLIMEPIRIDE- Glimepiride Tablet Redpharm Drug, Inc
GLIMEPIRIDE- glimepiride tablet RedPharm Drug, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use GLIMEPIRIDE TABLETS safely and effectively. See full prescribing information for GLIMEPIRIDE TABLETS. GLIMEPIRIDE Tablets USP for oral use Initial U.S. Approval: 1995 INDICATIONS AND USAGE Glimepiride is a sulfonylurea indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus ( 1.1) Important Limitations of Use: Not for treating type 1 diabetes mellitus or diabetic ketoacidosis ( 1.1) DOSAGE AND ADMINISTRATION Recommended starting dose is 1 or 2 mg once daily. Increase in 1 or 2 mg increments no more frequently than every 1 to 2 weeks based on glycemic response. Maximum recommended dose is 8 mg once daily ( 2.1) Administer with breakfast or first meal of the day. ( 2.1 ) Use 1 mg starting dose and titrate slowly in patients at increased risk for hypoglycemia (e.g., elderly, patients with renal impairment) ( 2.1) DOSAGE FORMS AND STRENGTHS Tablets (scored): 1 mg, 2 mg, 4 mg ( 3) CONTRAINDICATIONS Hypersensitivity to glimepiride or any of the product’s ingredients ( 4) Hypersensitivity to sulfonamide derivatives ( 4) WARNINGS AND PRECAUTIONS Hypoglycemia: May be severe. Ensure proper patient selection, dosing, and instructions, particularly in at-risk populations (e.g., elderly, renally impaired) and when used with other anti-diabetic medications ( 5.1). Hypersensitivity Reactions: Postmarketing reports include anaphylaxis, angioedema and Stevens- Johnson Syndrome. Promptly discontinue glimepiride, assess for other causes, institute appropriate monitoring and treatment, and initiate alternative treatment for diabetes ( 5.2). -

Indiscriminative Effects of Repaglinide and Other Specific Modulators of Transmembrane KATP-Channel Gating Properties Upon Ischa
Journal of Clinical and Basic Cardiology An Independent International Scientific Journal Journal of Clinical and Basic Cardiology 2003; 6 (Issue 1-4), 81-85 Indiscriminative Effects of Repaglinide and Other Specific Modulators of Transmembrane KATP-Channel Gating Properties upon Ischaemic/Hypoxic Bovine Coronary Artery Smooth Muscle Relaxation Gasser R, Esche G, Gasser S, Holzmann S, Köppel H Moosbrugger B, Salzer M Homepage: www.kup.at/jcbc Online Data Base Search for Authors and Keywords Indexed in Chemical Abstracts EMBASE/Excerpta Medica Krause & Pachernegg GmbH · VERLAG für MEDIZIN und WIRTSCHAFT · A-3003 Gablitz/Austria ORIGINAL PAPERS, BASIC CARDIOLOGY Repaglinide and Coronary Dilation J Clin Basic Cardiol 2003; 6: 81 Indiscriminative Effects of Repaglinide and Other Specific Modulators of Transmembrane KATP-Channel Gating Properties upon Ischaemic/Hypoxic Bovine Coronary Artery Smooth Muscle Relaxation R. Gasser1, H. Köppel2, B. Moosbrugger1, G. Esche1, M. Salzer1, S. Gasser1, S. Holzmann3 The opening of KATP channels both in myocardium and vascular smooth muscle constitutes an important mechanism in the regulation of myocardial metabolism and perfusion, in particular, during hypoxia and ischaemia. In coronary smooth muscle, KATP channel opening invariably leads to vasodilation and hence to improved myocardial perfusion. Blockade of these chan- nels may disturb this pivotal response. We compare the effects of glibenclamide with two new sulfonylureas on coronary artery dilation secondary to hypoxia and simulated ischaemia. We use bovine coronary arteries in a modified Tyrode solution (equili- brated with 95 % O2 and 5 % CO2 at 37 °C at a constant pH of 7.4). The solution contained the following solutes (in mM): NaCl 112.8, KCl 26.8, CaCl2 1.36, MgSO4 1.16, NaHCO3 11.9, glucose 10.1. -

Sulfonylurea Treatment of Type 2 Diabetic Patients Does Not Reduce the Vasodilator Response to Ischemia
Pathophysiology/Complications ORIGINAL ARTICLE Sulfonylurea Treatment of Type 2 Diabetic Patients Does Not Reduce the Vasodilator Response to Ischemia 1 1 PAOLO SPALLAROSSA, MD LUCA OLIVOTTI, MD vided by the discovery that sulfonylurea 2 2 MARA SCHIAVO, MD RENZO CORDERA, MD drugs stimulate insulin secretion by 1 1 ϩ PIERFRANCO ROSSETTIN, MD CLAUDIO BRUNELLI, MD  1 blocking -cell ATP-sensitive K (KATP) STEFANO CORDONE, MD channels (5). KATP channels are also abundantly present in the cardiac muscle and in vascular smooth muscle cells in coronary and peripheral arteries, where they play a key role in the protective OBJECTIVE — Sulfonylureas block the activation of vascular potassium-dependent ATP channels and impair the vasodilating response to ischemia in nondiabetic individuals, but it is mechanisms that are triggered during not known whether this occurs in type 2 diabetic patients under chronic treatment with these ischemia (6,7). Soon after the onset of drugs. Glimepiride, a new sulfonylurea, apparently has no cardiovascular interactions. The aim ischemia, the activation of KATP channels of our study was to compare the effect of the widely used compound glibenclamide, the pan- decreases vascular resistance and in- creas-specific glimepiride, and diet treatment alone on brachial artery response to acute forearm creases blood flow (ischemic vasodila- ischemia. tion) and renders myocardial cells more resistant to a subsequent bout of ischemia RESEARCH DESIGN AND METHODS — Brachial artery examination was performed Ϯ Ϯ (the so-called ischemic preconditioning) by a high-resolution ultrasound technique on 20 type 2 diabetic patients aged (mean SD) 67 (8,9). A great deal of experimental evi- 2 years and on 18 nondiabetic patients matched for age, hypertension, and dislipidemia. -
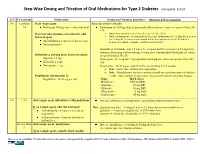
Step-Wise Dosing and Titration of Oral Medications for Type 2 Diabetes Last Update 5/3/10
Step-Wise Dosing and Titration of Oral Medications for Type 2 Diabetes last update 5/3/10 A1C S Creatinine Medications Dosing and Titration guidelines - (Recheck A1C in 3 months) 7-8 Less than Start single agent Increase every 1-2 weeks 1.4 Metformin 500 mg twice a day with food Metformin: by 500 mg daily if preprandial blood glucose values are greater than 130- 150. If on max tolerated dose of metformin, add o Note: slow titration is needed to decrease GI side effects 2nd oral agent o Note: metformin use is contraindicated in renal dysfunction (Scr>1.5mg/dL in men or Scr>1.4mg/dL in females) and should not be used in patients aged >80 unless a Add sulfonylurea (preferred due to cost) measured creatinine clearance is within normal limits. Add pioglitazone Glipizide or Glyburide: add 2.5 mg in the evening and then increase by 2.5 mg in the morning alternating with increasing evening dose if preprandial blood glucose values Sulfonylurea starting doses before breakfast: are greater than 130-150. Glipizide 2.5 mg Glimepiride: by 1 mg daily if preprandial blood glucose values are greater than 130- Glyburide 2.5 mg 150 Glimepiride 1 mg Pioglitazone : by 15 mg per day if A1C is greater than 7 in 3 months. o Note: slower dose titration for pioglitazone o Note: Rosiglitazone has been associated with increased incidence of adverse Pioglitazone starting dose is: events. (American Diabetes Association: Consensus 2009 and 2007 Black Box Warning) Pioglitazone 15-30 mg per day Name MAX doses Metformin - 1000 mg BID Glipizide - 20 mg BID Glyburide -