Resolution of Pinguecula-Related Dry Eye Disease After Argon Laser Photocoagulation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -
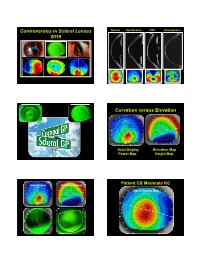
Controversies in Scleral Lenses 2019 Curvature Versus Elevation
Controversies in Scleral Lenses Normal Keratoconus PMD Keratoglobus 2019 Curvature versus Elevation Axial Display Elevation Map Power Map Height Map Axial Display Elevation Display Patient CB Moderate KC Axial Display Map +180um +180 +379 +379um Elevation Display -110 - 276 Elevation Map 655 Above the 290 microns Micron Sphere Height -276um Differential Depression Below the -110um Sphere N = 87 Patients 127 CL Fits Less than 350um Greater than 350um Patients with 350um or less of corneal elevation difference (along the greatest meridian of change) have an 88.2% chance of success with a corneal GP lens. The Re-Birth of Scleral Lenses Glass Scleral Lenses 1887 Molding Glass Scleral Lenses Average 8.5 High DK Scleral Materials Traditional Corneal / Scleral • Menicon Z Dk = 163 Shape • B & L, Boston XO2 DK = 141 • Contamac, Optimum Extreme DK = 125 • B & L, Boston XO DK = 100 • Paragon HDS 100 DK = 100 • Contamac, Optimum Extra DK = 100 • Lagado, Tyro -97 DK = 97 Scleral Shape Cone Angle Circa 1948 Klaus Pfortner New Understandings Argentina Scleral Lens Fitting Objectives Anatomy of a Scleral Lens 1. Central Vault Zone (250 to 400 microns) 2. Peripheral Lift Zone 4 3 2 1 2 3 4 3. Limbal Lift Zone 4. Scleral Landing Zone Ocular Surface Disease Scleral Lens Indications Scleral Irregular Astigmatism Lens • Keratoconus Indications • Pellucid Marginal Degeneration • Post Corneal Trauma • Post keratoplasty • Post K-Pro • Post Refractive Surgery RK, PRK and LASIK • Post HSV and HZV • Athletes • GP stability (rocking) issues Corneal Irregularity -

Pterygium & Pinguecula
Dr. Anthony O. Roberts 9715 Medical Center Drive Pterygium & Pinguecula Suite 502 Rockville, MD 20850 A pterygium is a mass of fleshy tissue that Phone: 301-279-0600 E-mail: [email protected] grows over the cornea (the clear front window of the eye). It may remain small or may grow large enough to interfere with vision. A ptery- gium most commonly occurs on the inner cor- Eye Care Services ner of the eye, but it can appear on the outer Eye Exams corner as well. Glaucoma Testing & The exact cause of pterygia is not well understood. They occur more often Treatment in people who spend a lot of time outdoors, especially in sunny climates. Cataract Surgery Long-term exposure to sunlight, especially to ultraviolet (UV) rays, and Diabetic Evaluation chronic eye irritation from dry, dusty conditions seem to play an important LASIK Eye Surgery role. Dry eye also may contribute to pterygium. PRK Surgery Refractive Procedures When a pterygium becomes red and irritated, eyedrops or ointments can be used to help reduce the inflammation. If the pterygium grows rapidly or is Our Practice large enough to threaten sight, it can be removed surgically. At Shady Grove Ophthal- mology, we understand the Despite proper surgical removal, a pterygium may return, particularly in importance of your vision. young people. Protecting the eyes from excessive ultraviolet light with We are committed to offering proper sunglasses, avoiding dry, dusty conditions, and using artificial tears the highest quality eye care can also help. using the most state-of-the- art technologies. Dr. An- thony Roberts delivers pre- A pinguecula is a yellowish patch or bump on the white of the eye, most mium quality eye care and often on the side closest to the nose. -

Gibberman – Advances in Scleral Lens Technology
ADVANCES IN SCLERAL LENS TECHNOLOGY ALEX GIBBERMAN, OD, FAAO, FSLS 2020 EYECARE, LOVELAND, OHIO A BRIEF HISTORY OF THE WORLD…OF SCLERALS 16th century- Da Vinci concepts. Blown glass shell. No power. 1887-Muller brothers. Thinner blown glass shells 1888- Adolf Fick. Glass lenses first to treat k conus with correction. First to note corneal edema 1889- Dr. Kirstein is born! Also August Muller is first to use scleral to correct for high myopia HISTORY CONTINUED… 1890’s- The use of saline with scleral insertion is introduced 1912- Zeiss makes first diagnostic fitting set Also notable in 1912, Dr Zelczak is born! 1957-PMMA sclerals introduced. 1970s-John James Little and Arthur Irving first to use RGP sclerals 1983-RGP scleral materials updated by optometrist Don Ezekiel MODERN SCLERALS Between the mid 1980s and now, significant material and dk improvements have occurred. Late 1980s- Back toric optics were introduced to sclerals 1992- the first impression based, computer scanned and created lens was made in the UK 2013-EyePrintPro was developed to take an impression and match exact contour of the eye Current- multifocal optics, decentered optics, front toric and back toric optics, prism and higher order aberration correction are all possible Scleral topographers: Getting us closer to empirical fitting. We will discuss in more detail SPECIFICATIONS OF A MODERN SCLERAL LENS? Here is just one example Base Curve 7.50 Diameter 16.1 mm Sagittal Depth: 3500um Toric Peripheral curve, flatten horizontal meridian 100um steepen vertical meridian 200um Front toric overall power -400 -125 x 105 Multifocal Center ADD 2.5mm Zone +250 ADD Nasal microvault or notch to avoid pinguecula Material: Optimum Infinite Dk 200 needs hydropeg coating WHAT A CURRENT SCLERAL LOOKS LIKE SCLERAL TOPOGRAPHERS Eaglet- Eye surface profiler Pentacam- CSP Visionary Optics-Smap3D Latitude Focal Points Focal Points will allow the import of multiple types of scleral topography files such as Eaglet ESP, Pentacam CSP and sMap. -
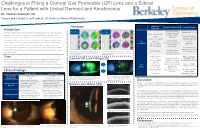
Lens for a Patient with Limbal Dermoid and Keratoconus
Challenges in Fitting a Corneal Gas Permeable (GP) Lens and a Scleral Lens for a Patient with Limbal Dermoid and Keratoconus By: Vakishan Nadarajah, OD Cornea and Contact Lens Resident, UC Berkeley School of Optometry Initial Lens Pentacam Initial Lens Evaluation Lens Modifications Introduction Parameters Moderate apical Right Eye: Left Eye: Flattened BC to 7.30 Limbal dermoids are benign congenital tumors containing histological tissue such as epidermal clearance & small – appendages, teeth, or bone. If enlarged, they can cause amblyopia due to induced corneal OAD: 8.8mm, BC: central bubbles Decreased apical 7.20 (Figure 5a) astigmatism. Keratoconus is an ocular disease that causes irregularity from progressive corneal clearance, but small Power: -7.75DS insertion bubble still thinning. Corneal GPs and scleral lenses are non-surgical devices indicated to improve vision Mid-peripheral OD OZ: 6.4 present for such irregular corneas by providing an optically regular surface for light to refract through. bearing temporally due Corneal GP (Figure 5b) SCr: 8.6/0.6 to inferonasal However, it is much more difficult to fit lenses for patients with both irregular corneas and PCr: 10.5/0.4 decentration Patient reported irregular conjunctivas. Fortunately, these gas permeable lenses can be altered in size and fit to improved comfort and provide optimal vision. This case outlines techniques to best fit a patient with irregular corneas Adequate edge Figure 3) Pentacam analysis shows mild keratoconus Figure 4) Pentacam analysis shows severe keratoconus -

Ryan P. Ames, OD, MBA the Chief Complaint Drives the Bus December 2019 This Is One of the Fundamental Concepts in Patient Driv
Ryan P. Ames, OD, MBA [email protected] 888.456.2046 The Chief Complaint Drives the Bus December 2019 This is one of the fundamental concepts in patient driven care and in proper documentation. Nearly every day we see a patient, one will come in complaining of one thing, and we will discover a completely different condition that we feel is more important. They may not even have symptoms of this new condition. The Chief Complaint (CC) or Reason for Visit (RFV) can certainly be doctor directed from a prior visit. But the concept is the same, whether the CC/RFV is doctor directed or patient driven, this is the condition that will become the primary diagnosis. Remember, auditors are often employed by third-party companies and they derive their revenue based on a percentage of what they recover. Therefore, they are going to look for low-hanging fruit that has a high potential for recoupment of payment. The CC/RFV is a very easily identified element of the exam and if the primary diagnosis does not address it, they could deem the entire encounter unnecessary and recoup the payment. The other day I saw a long-time patient with no prior medical diagnosis except a pinguecula. He also had no visual complaints. He came in saying, “I think those white bumps are getting bigger and are sometimes red.” On exam, the vision in his right eye was slightly reduced to 20/25- with no improvement after refraction. During the retinal exam, her appeared to have mild epiretinal membranes and the OCT confirmed that finding. -

Diagnosis and Management of Common Eye Problems
Diagnosis and Management of Common Eye Problems Review of Ocular Anatomy Picture taken from Basic Ophthalmology for Medical Students and Primary Care Residents published by the American Academy of Ophthalmology Diagnosis and Management of Common Eye Problems Fernando Vega, MD Lacrimal system and eye musculature Eyelid anatomy Picture taken from Basic Ophthalmology for Medical Students and Primary Care Residents published by the American Academy of Ophthalmology n Red Eye Disorders: An Anatomical Approach n Lids n Orbit n Lacrimal System n Conjunctivitis n Cornea n Anterior Chamber Fernando Vega, MD 1 Diagnosis and Management of Common Eye Problems Red Eye Disorders: What is not in the scope of Red Eye Possible Causes of a Red Eye n Loss of Vision n Trauma n Vitreous Floaters n Chemicals n Vitreous detatchment n Infection n Retinal detachment n Allergy n Chronic Irritation n Systemic Infections Symptoms can help determine the Symptoms Continued diagnosis Symptom Cause Symptom Cause Itching allergy Deep, intense pain Corneal abrasions, scleritis Scratchiness/ burning lid, conjunctival, corneal Iritis, acute glaucoma, sinusitis disorders, including Photophobia Corneal abrasions, iritis, acute foreign body, trichiasis, glaucoma dry eye Halo Vision corneal edema (acute glaucoma, Localized lid tenderness Hordeolum, Chalazion contact lens overwear) Diagnostic steps to evaluate the patient with Diagnostic steps continued the red eye n Check visual acuity n Estimate depth of anterior chamber n Inspect pattern of redness n Look for irregularities in pupil size or n Detect presence or absence of conjunctival reaction discharge: purulent vs serous n Look for proptosis (protrusion of the globe), n Inspect cornea for opacities or irregularities lid malfunction or limitations of eye n Stain cornea with fluorescein movement Fernando Vega, MD 2 Diagnosis and Management of Common Eye Problems How to interpret findings n Decreased visual acuity suggests a serious ocular disease. -

Pigeucula and Pterygium
What Is a Pinguecula and a Pterygium (Surfer's Eye)? Written By: Kierstan Boyd Reviewed By: James M Huffman, MD Oct. 29, 2020 Pinguecula and pterygium are growths on your eye’s conjunctiva, the clear covering over the white part of the eye. Pinguecula is a yellowish, raised growth on the conjunctiva. It’s usually on the side of the eye near your nose, but can happen on the other side too. A pinguecula is a deposit of protein, fat, or calcium. Pterygium is a growth of fleshy tissue (has blood vessels) that may start as a pinguecula. It can remain small or grow large enough to cover part of the cornea. When this happens, it can affect your vision. Both pinguecula and pterygium are believed to be caused by a combination of exposure to ultraviolet (UV) light from the sun, wind and dust. Avoiding pinguecula and pterygium lf you have had a pinguecula or a pterygium at least once before, try to avoid the things that cause these growths. Here are some ways: ● wear sunglasses to protect your eyes from ultraviolet (UV) light ● protect your eyes from dust by wearing glasses or goggles ● use artificial tears when your eyes are dry Symptoms of pinguecula and pterygium can range from mild to severe. They include: ● redness and swelling of the conjunctiva, mostly while the pterygium grows ● a yellow spot or bump on the white of your eye ● dry, itchy, burning eyes. Or feeling like sand or grit is stuck in your eye ● blurry vision In many cases pinguecula and pterygium do not need to be treated. -

Disclosure Ocular Anatomy and Motility Ocular Anatomy Overview the Human Vision System the Human Vision System Lids and Lacrimal
10/19/2012 Disclosure Ocular Anatomy and Motility Jenean Carlton BA, ABOC, NCLC 9President, Carlton & Associates, LLC – Carlton and Associates, 6 Course #214 Monterey Symposium LLC provides communications and educational materials for the optical industry 9Contributing Editor for Refractive Eyecare magazine. 6 Jenean Carlton BA, ABOC, NCLC 9Contributing Author Eyecare Business magazine. 9Communications Committee member OWA. 9Has been in the optical industry for 30 years with more than half of this time working in practices. 9Vision Monday’s Most Influential Women Award in Optical 2005 1 Ocular Anatomy Overview The Human Vision System 9 The eye is an amazing organ that works like a camera. 9 Think of the cornea and crystalline lens as the lenses of a camera, the iris as the shutter, and the retina as the photographic film. The Human Vision System Lids and Lacrimal System Vision takes place in the occipital lobe of The tear film has 3 layers: the brain Outer: the lipid layer (meibomian 9The brain can be glands in lids) is the oil layer. thought of as the development Middle: the aqueous layer center because it (lacrimal glands) is mainly water and provides oxygen converts and nutrients. electrical signals from the retina Inner: the mucin layer (goblet cells in conjunctiva) helps the tears into vision. adhere to the cornea. It is the mucus layer. 1 10/19/2012 Dry Eye Syndrome Lid Disorders What causes dry eyes? Ectropion= Out Treatments Entropion= In Ptosis- a drooping of the lid. Lids can have other problems too like turning out, in. Lids Disorders Lid Disorders Blepharitis is a chronic Hordeolum (stye) - inflammation- not an acute inflammation of a infection. -

Sclera, Choroid, Retina, Oh My! AMIEE HO, OD, FAAO PACIFIC UNIVERSITY
Statement of Disclosures No financial disclosures https://en.wikipedia.org/wiki/The_Wizard_of_Oz_(1939_film)#/media/File:Judy_Garland_in_The_Wizard_of_Oz_trailer_2.jpg Sclera, Choroid, Retina, oh my! AMIEE HO, OD, FAAO PACIFIC UNIVERSITY Cases The Red Eye The Black Spot Good Vision Super Healthy Guy The Red Eye A little bump in the road 64 year old African American male Ocular History CC: Eye pain and redness OD x 3 days Ocular Hx: ◦ >> Pain with bright light ◦ Age‐related cataracts OU ◦ Pain is dull(?) ◦ Dry eye OU vs. mild mucus fishing syndrome ◦ Gradually more painful ◦ Mild blurred vision ◦ Slightly more scleral show OS>OD ◦ Exophthalmometry nearly symmetric ◦ A little watery https://pixabay.com/photos/cat‐wink‐funny‐fur‐animal‐red‐1333926/ ◦ First time, no previous Hx of similar pain ◦ Refractive error OU and presbyopia ◦ (‐)trauma; (‐)FB; (‐)itchiness; (‐)mucus; (‐) CL wearer LEE: ~1 month ago Medical History Medications and Vitals Medical Hx: Medications Vitals o HEMOGLOBIN: 13.5 g/dL ◦Anemia o DILTIAZEM o HEMATOCRIT: 40.0 % o ALBUTEROL ◦Asthma o PLATELETS: 295 k/uL o BUDESONIDE/FORMOTEROL o INR: 1.3 RATIO ◦COPD o TIOTROPIUM o HEMOGLOBIN A1C: 5.9 % H o CARBOXYMETH 0.5% (REFRESH TEARS) ◦GERD o GLUCOSE: 101 mg/dL o OMEPRAZOLE ◦Hypertension o MICROALBUMIN: 1.6 mg/dL o ESTIMATED GLOMERULAR FILTRATION o Allergies: NKDA ◦Hyperlipidemia RATE: 70 mL/min/m2* o CHOLESTEROL: 183 mg/dL ◦Primary Hyperparathyroidism https://pixabay.com/illustrations/doctor‐african‐oncology‐orthopaedic‐3187935/ o HDL: 30 mg/dL L ◦Prostate Cancer o LDL: 129 mg/dL -

Cornea and External Disease Robert Cykiert, M.D
Cornea and External Disease Robert Cykiert, M.D. I. Basics papilla vascular response if giant, the differential includes atopy, vernal, GPC, prosthesis, suture follicles lymphatic response acute chronic EKC, pharygoconjunctival fever adult inclusion conjunctivitis medicamentosa (epinephrine, neosynephrine) toxic Parinaud's oculoglandular,syndrome r/o sarcoid HSV primary conjunctivitis r/o GPC, vernal conjunctivitis Newcastle's conjunctivitis with acute follicles, always check lid margin for HSV vesicles, ulcers membranes conjunctivitis ocular cicatricial pemphigoid erythema multiforme Stevens Johnson syndrome Srogrens syndrome atopy Symblepharon scieroderrna burns radiation burns trachoma EKC sarcoid drugs filaments exposure (keratoconjunctivitis sicca, neurotrophic, patching recurrent erosion) bullous keratopathy HSV meds superior limbic keratoconjunctivitis psoriasis aerosol keratitis diabetes mellitus radiation retained FB Thygeson's SPK ptosis Enlarged Corneal nerves MEN TIIb icthyosis Hanson's Kconus Refsums Fuchs corneal dystrophy old age failed PKP congenital glaucoma trauma neurofibromatosis MEN TIIb AD with thick corneal nerves, medullary thyroid cancer, pheochromocytoma, mucosal neuromas, and marfanoid habitus thickened lid margin with rostral lashes, thick lips, epibulbar neuromas cafe au lait spots, periungual, lingual neuromas often confused with NFI often die early from amyloid producing thyroid cancer in 10-20 year old with distant mets at dx thick nerves precede the cancer! corneal edema whenever epithelium disrupted, -
Avoiding Pinguecula and Pterygium
gggdgdgd May Vincent P. Basilice, M.D., P.C. Medical Director Michael S. Conners, M.D., Ph.D. Alexander J. Llinas, M.D., Ph.D. Alex J. Schaffer, O.D. Avoiding Pinguecula and Pterygium Pinguecula and pterygium are growths on your eye’s conjunctiva, the clear covering over the white part of the eye. Pinguecula is a growth that looks like a yellow spot or bump on the conjunctiva. It often appears on the side of the eye near your nose. A pinguecula is a deposit of protein, fat, or calcium. Pterygium is a growth of fleshy tissue that may start as a pinguecula. It can remain small or grow large enough to cover part of the cornea. When this happens, it can affect your vision. Both pinguecula and pterygium are believed to be caused by a combination of dry eye, sand exposure to wind, dust, and ultraviolet (UV) light from the sun. How to avoid pinguecula or a pterygium: If you have had a pinguecula or a pterygium at least once before, try to avoid the things that cause these growths. Here are some ways: Wear polarized sunglasses to protect your eyes from UV rays, wear goggles to protect your eyes from dust and use artificial tears when your eyes are dry. New Trifocal IOL Technology is Now Available The AcrySof® IQ PanOptix® Trifocal IOL is a new cutting-edge multifocal IOL that optimizes intermediate vision without compromising near and distance vision. The PanOptix Trifocal IOL focuses images clearly on the retina at the back of the eye. This allows for sharp vision after cataract removal.