Pigeucula and Pterygium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -
Controversies in Scleral Lenses 2019 Curvature Versus Elevation
Controversies in Scleral Lenses Normal Keratoconus PMD Keratoglobus 2019 Curvature versus Elevation Axial Display Elevation Map Power Map Height Map Axial Display Elevation Display Patient CB Moderate KC Axial Display Map +180um +180 +379 +379um Elevation Display -110 - 276 Elevation Map 655 Above the 290 microns Micron Sphere Height -276um Differential Depression Below the -110um Sphere N = 87 Patients 127 CL Fits Less than 350um Greater than 350um Patients with 350um or less of corneal elevation difference (along the greatest meridian of change) have an 88.2% chance of success with a corneal GP lens. The Re-Birth of Scleral Lenses Glass Scleral Lenses 1887 Molding Glass Scleral Lenses Average 8.5 High DK Scleral Materials Traditional Corneal / Scleral • Menicon Z Dk = 163 Shape • B & L, Boston XO2 DK = 141 • Contamac, Optimum Extreme DK = 125 • B & L, Boston XO DK = 100 • Paragon HDS 100 DK = 100 • Contamac, Optimum Extra DK = 100 • Lagado, Tyro -97 DK = 97 Scleral Shape Cone Angle Circa 1948 Klaus Pfortner New Understandings Argentina Scleral Lens Fitting Objectives Anatomy of a Scleral Lens 1. Central Vault Zone (250 to 400 microns) 2. Peripheral Lift Zone 4 3 2 1 2 3 4 3. Limbal Lift Zone 4. Scleral Landing Zone Ocular Surface Disease Scleral Lens Indications Scleral Irregular Astigmatism Lens • Keratoconus Indications • Pellucid Marginal Degeneration • Post Corneal Trauma • Post keratoplasty • Post K-Pro • Post Refractive Surgery RK, PRK and LASIK • Post HSV and HZV • Athletes • GP stability (rocking) issues Corneal Irregularity -

Pterygium & Pinguecula
Dr. Anthony O. Roberts 9715 Medical Center Drive Pterygium & Pinguecula Suite 502 Rockville, MD 20850 A pterygium is a mass of fleshy tissue that Phone: 301-279-0600 E-mail: [email protected] grows over the cornea (the clear front window of the eye). It may remain small or may grow large enough to interfere with vision. A ptery- gium most commonly occurs on the inner cor- Eye Care Services ner of the eye, but it can appear on the outer Eye Exams corner as well. Glaucoma Testing & The exact cause of pterygia is not well understood. They occur more often Treatment in people who spend a lot of time outdoors, especially in sunny climates. Cataract Surgery Long-term exposure to sunlight, especially to ultraviolet (UV) rays, and Diabetic Evaluation chronic eye irritation from dry, dusty conditions seem to play an important LASIK Eye Surgery role. Dry eye also may contribute to pterygium. PRK Surgery Refractive Procedures When a pterygium becomes red and irritated, eyedrops or ointments can be used to help reduce the inflammation. If the pterygium grows rapidly or is Our Practice large enough to threaten sight, it can be removed surgically. At Shady Grove Ophthal- mology, we understand the Despite proper surgical removal, a pterygium may return, particularly in importance of your vision. young people. Protecting the eyes from excessive ultraviolet light with We are committed to offering proper sunglasses, avoiding dry, dusty conditions, and using artificial tears the highest quality eye care can also help. using the most state-of-the- art technologies. Dr. An- thony Roberts delivers pre- A pinguecula is a yellowish patch or bump on the white of the eye, most mium quality eye care and often on the side closest to the nose. -

Gibberman – Advances in Scleral Lens Technology
ADVANCES IN SCLERAL LENS TECHNOLOGY ALEX GIBBERMAN, OD, FAAO, FSLS 2020 EYECARE, LOVELAND, OHIO A BRIEF HISTORY OF THE WORLD…OF SCLERALS 16th century- Da Vinci concepts. Blown glass shell. No power. 1887-Muller brothers. Thinner blown glass shells 1888- Adolf Fick. Glass lenses first to treat k conus with correction. First to note corneal edema 1889- Dr. Kirstein is born! Also August Muller is first to use scleral to correct for high myopia HISTORY CONTINUED… 1890’s- The use of saline with scleral insertion is introduced 1912- Zeiss makes first diagnostic fitting set Also notable in 1912, Dr Zelczak is born! 1957-PMMA sclerals introduced. 1970s-John James Little and Arthur Irving first to use RGP sclerals 1983-RGP scleral materials updated by optometrist Don Ezekiel MODERN SCLERALS Between the mid 1980s and now, significant material and dk improvements have occurred. Late 1980s- Back toric optics were introduced to sclerals 1992- the first impression based, computer scanned and created lens was made in the UK 2013-EyePrintPro was developed to take an impression and match exact contour of the eye Current- multifocal optics, decentered optics, front toric and back toric optics, prism and higher order aberration correction are all possible Scleral topographers: Getting us closer to empirical fitting. We will discuss in more detail SPECIFICATIONS OF A MODERN SCLERAL LENS? Here is just one example Base Curve 7.50 Diameter 16.1 mm Sagittal Depth: 3500um Toric Peripheral curve, flatten horizontal meridian 100um steepen vertical meridian 200um Front toric overall power -400 -125 x 105 Multifocal Center ADD 2.5mm Zone +250 ADD Nasal microvault or notch to avoid pinguecula Material: Optimum Infinite Dk 200 needs hydropeg coating WHAT A CURRENT SCLERAL LOOKS LIKE SCLERAL TOPOGRAPHERS Eaglet- Eye surface profiler Pentacam- CSP Visionary Optics-Smap3D Latitude Focal Points Focal Points will allow the import of multiple types of scleral topography files such as Eaglet ESP, Pentacam CSP and sMap. -
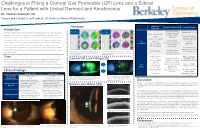
Lens for a Patient with Limbal Dermoid and Keratoconus
Challenges in Fitting a Corneal Gas Permeable (GP) Lens and a Scleral Lens for a Patient with Limbal Dermoid and Keratoconus By: Vakishan Nadarajah, OD Cornea and Contact Lens Resident, UC Berkeley School of Optometry Initial Lens Pentacam Initial Lens Evaluation Lens Modifications Introduction Parameters Moderate apical Right Eye: Left Eye: Flattened BC to 7.30 Limbal dermoids are benign congenital tumors containing histological tissue such as epidermal clearance & small – appendages, teeth, or bone. If enlarged, they can cause amblyopia due to induced corneal OAD: 8.8mm, BC: central bubbles Decreased apical 7.20 (Figure 5a) astigmatism. Keratoconus is an ocular disease that causes irregularity from progressive corneal clearance, but small Power: -7.75DS insertion bubble still thinning. Corneal GPs and scleral lenses are non-surgical devices indicated to improve vision Mid-peripheral OD OZ: 6.4 present for such irregular corneas by providing an optically regular surface for light to refract through. bearing temporally due Corneal GP (Figure 5b) SCr: 8.6/0.6 to inferonasal However, it is much more difficult to fit lenses for patients with both irregular corneas and PCr: 10.5/0.4 decentration Patient reported irregular conjunctivas. Fortunately, these gas permeable lenses can be altered in size and fit to improved comfort and provide optimal vision. This case outlines techniques to best fit a patient with irregular corneas Adequate edge Figure 3) Pentacam analysis shows mild keratoconus Figure 4) Pentacam analysis shows severe keratoconus -

Comparitive Study of Astigmatism Before and After Pterygium Excision
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 18, Issue 8 Ser. 6 (August. 2019), PP 24-26 www.iosrjournals.org Comparitive Study of Astigmatism before and After Pterygium Excision. Dr. Divya V Shenoy¹, Dr. Nelly Nazareth² 1 (Postgraduate , Deparment of Ophthalmology, Father Muller Medical college Hosptial , India) 2 (Associate Professor, Department of Ophthalmology, Fathermuller Medical college Hospital , India) Corresponding author: Dr. Divya V Shenoy Abstract: Objective:To study the reversal of induced astigmatism by pterygium following its excision and conjunctival limbal autograft with no suture and no glue technique. Methods: 33 patients with nasal pterygium were included. All patients were examined and graded for the degree of pterygium, keratometry and visual acuity before and after the procedure. All patients underwent pterygium excision with conjunctival limbal autograft with no suture no glue technique by the same surgeon.Results :Amoung 33 patients ,16 patients with grade 1 and 17 with grade 2 were included.There was significant reduction of astigmatism post operatively in the form of reduction in the difference between K1 and K2 for Grade 1 (p= 0.001) and Grade 2 ptergia. (p< 0.001)The post operative difference of K1-K2 stabilizes at 1 month.Conclusion: There is significant improvement in post op visual acuity and induced astigmatism following pterygium excision . Key words: Pterygium, Astigmatism. ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission: 29-07-2019 Date of Acceptance: 14-08-2019 ----------------------------------------------------------------------------------------------------------------------------- ---------- I. Introduction Pterygium is a fibroelastic degeneration of the conjunctiva with encroachment onto the cornea.It is a wingshaped overgrowth of fibrovascular connective tissue of the bulbar conjunctiva toward and onto the cornea. -

Causes of Heterochromia Iridis with Special Reference to Paralysis Of
CAUSES OF HETEROCHROMIA IRIDIS WITH SPECIAL REFER- ENCE TO PARALYSIS OF THE CERVICAL SYMPATHETIC. F. PHINIZY CALHOUN, M. D. ATLANTA, GA. This abstract of a candidate's thesis presented for membership in the American Ophthal- mological Society, includes the reports of cases, a general review of the literature of the sub- ject, the results of experiments, and histologic observations on the effect of extirpation of the cervical sympathetic in the rab'bit, the conclusions reached from the investigation, and a bib- liography. That curious condition which con- thinks that the word hetcrochromia sists in a difference in the pigmentation should apply to those cases in which of the two eyes, is regarded by the parts of the same iris have different casual observer as a play or caprice of colors. In those cases where a cycli- nature. This phenomenon has for cen- tis accompanies the iris decoloration, turies been noted, and was called hcte- Butler8 uses the term "heterochromic roglaucus by Aristotle1. One who cyclitis," but the "Chronic Cyclitis seriously studies the subject, is at once with Decoloration of the Iris" as de- impressed with the complexity of the scribed by Fuchs" undoubtedly gives a situation, and soon learns that nature more accurate description of the dis- plays a comparatively small part in its ease, notwithstanding its long title. causation. It is however only within The commonly accepted and most uni- a comparatively recent time that the versally used term Hetcrochromia Iri- pathologic aspect has been considered, dis exactly expresses and implies the and in this discussion I especially wish picture from its derivation (irtpoa to draw attention to that part played other, xpw/xa) color. -

A Complete Guide to Pterygium Surgery
A Complete Guide to Pterygium | Carnosidad del ojos Surgery A Complete Guide to Pterygium | Carnosidad del ojos Surgery A Complete Guide to Pterygium Surgery 1 1 Building a Practice with Passion – ¾ OF THE PAGE THIS TEXT OTHER PART FULL PHOTO OF DR. MARTINEZ LABELED AT BuildingTHE BOTTOM LEFT HAND a CORNERPractice J. Alberto Martinez, with MD Pterygium, Passion Cataract & Refractive Surgeon How you see the world truly matters. A lot of us take it for granted, but Dr. Alberto Martinez does not. Your vision J. Alberto Martinez, MD is his passion and Pterygium, Cataract & Refractive Surgeon life’s work. How you see the world truly matters. A lot of us take it for granted, but Dr. Alberto Martinez does not. Your vision is his passion and life’s work. Having come to the U.S. from Colombia at the age of A Complete Guide to Pterygium | Carnosidad del ojos Surgery 2 Witnessing the profound effect on this person’s life, he was completely captivated. Since that time, Dr. Martinez has completely dedicated himself to offering the finest vision health care combined with offering the latest in technology. He has put together a team of experts or ‘the special ops’ team to 2 Having come to the U.S. from Colombia as an economic refugee, Dr. Martinez came to America to pursue the American dream. He worked in blue-collar jobs for three years and then served in the United States Navy for six years before finishing college summa cum laude at American University, and being admitted to Georgetown University Medical School. -

Concomitant Use of Conjunctival Tissue Graft from Pterygium Itself in Primary Pterygium Surgery
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 18, Issue 11 Ser.2 (November. 2019), PP 80-84 www.iosrjournals.org Concomitant Use of Conjunctival Tissue Graft from Pterygium Itself in Primary Pterygium Surgery 1. DrM.V.D.LSathyanarayanana,M.S, Department of ophthalmology Govt,Medical college Kadapa Andhra Pradesh,India 2.Dr.M.Sravani 23rd year PG in Ophthalmology Govt.MedicalCollege Kadapa Andhra Pradesh,India Corresponding Author: DrM.V.D.LSathyanarayanana Aims & objectives:To evaluate the outcome of concomitant use of conjunctival tissue graft from pterygium itself without use of glue or sutures in primary pterygium surgery. Materials & Methods: Study was conducted on 25 patients whose age>30 yrs with thorough ocular examination and blood investigationsrequired for surgery. After peribulbar anesthesia, thin layer of conjunctival graft was fashioned from pterygium tissue .This conjunctival layer from the pterygium itself was then separated completely from the underlying fibrovascular tissue and kept onto the corneal surface then fibrovascular tissue was excised. Thin conjunctival layer was then transferred to bare sclera bed with epithelial side up and without any rotation and adhered to the bare sclera bed using fibrin blood clot Results: The study showed the patient has minimal recurrence rate, no graft oedema. Keywords:Conjunctiva, pterygium ,autograft , fibrin glue , glaucoma , pterygium recurrence. ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission:24-10-2019 Date of Acceptance:09-11-2019 ----------------------------------------------------------------------------------------------------------------------------- ---------- I. Introduction Pterygium is believed to be a consequence of ultraviolet-induced damage with subsequent elastotic degeneration of conjunctival collagen. %. It is a wing-shaped ocular surface lesion traditionally described as an encroachment of bulbar conjunctiva onto the cornea. -

Ryan P. Ames, OD, MBA the Chief Complaint Drives the Bus December 2019 This Is One of the Fundamental Concepts in Patient Driv
Ryan P. Ames, OD, MBA [email protected] 888.456.2046 The Chief Complaint Drives the Bus December 2019 This is one of the fundamental concepts in patient driven care and in proper documentation. Nearly every day we see a patient, one will come in complaining of one thing, and we will discover a completely different condition that we feel is more important. They may not even have symptoms of this new condition. The Chief Complaint (CC) or Reason for Visit (RFV) can certainly be doctor directed from a prior visit. But the concept is the same, whether the CC/RFV is doctor directed or patient driven, this is the condition that will become the primary diagnosis. Remember, auditors are often employed by third-party companies and they derive their revenue based on a percentage of what they recover. Therefore, they are going to look for low-hanging fruit that has a high potential for recoupment of payment. The CC/RFV is a very easily identified element of the exam and if the primary diagnosis does not address it, they could deem the entire encounter unnecessary and recoup the payment. The other day I saw a long-time patient with no prior medical diagnosis except a pinguecula. He also had no visual complaints. He came in saying, “I think those white bumps are getting bigger and are sometimes red.” On exam, the vision in his right eye was slightly reduced to 20/25- with no improvement after refraction. During the retinal exam, her appeared to have mild epiretinal membranes and the OCT confirmed that finding. -

Floaters-Survey-Ophthalmol-2016.Pdf
survey of ophthalmology 61 (2016) 211e227 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/survophthal Major review Vitreous floaters: Etiology, diagnostics, and management Rebecca Milston, MOptoma, Michele C. Madigan, PhDb,c, J. Sebag, MD, FACS, FRCOphth, FARVOd,* a Centre for Eye Health, University of New South Wales, Sydney, New South Wales, Australia b School of Optometry and Vision Science, University of New South Wales, Sydney, New South Wales, Australia c Save Sight Institute and Discipline of Clinical Ophthalmology, Sydney Medical School, University of Sydney, New South Wales, Australia d VMR Institute for Vitreous Macula Retina, Huntington Beach, California, USA article info abstract Article history: Vitreous is a hydrated extracellular matrix comprised primarily of water, collagens, and Received 3 July 2015 hyaluronan organized into a homogeneously transparent gel. Gel liquefaction results from Received in revised form 25 molecular alterations with dissociation of collagen from hyaluronan and aggregation of November 2015 collagen fibrils forming fibers that cause light scattering and hence symptomatic floaters, Accepted 25 November 2015 especially in myopia. With aging, gel liquefaction and weakened vitreoretinal adhesion Available online 8 December 2015 result in posterior vitreous detachment, the most common cause of primary symptomatic floaters arising from the dense collagen matrix of the posterior vitreous cortex. Recent Keywords: studies indicate that symptomatic floaters are not only more prevalent, but also have a vitreous negative impact on the quality of life that is greater than previously appreciated. We review collagen the literature concerning management of symptomatic vitreous floaters, currently either myopia with observation, vitrectomy, or Nd:YAG laser. -

Diagnosis and Management of Common Eye Problems
Diagnosis and Management of Common Eye Problems Review of Ocular Anatomy Picture taken from Basic Ophthalmology for Medical Students and Primary Care Residents published by the American Academy of Ophthalmology Diagnosis and Management of Common Eye Problems Fernando Vega, MD Lacrimal system and eye musculature Eyelid anatomy Picture taken from Basic Ophthalmology for Medical Students and Primary Care Residents published by the American Academy of Ophthalmology n Red Eye Disorders: An Anatomical Approach n Lids n Orbit n Lacrimal System n Conjunctivitis n Cornea n Anterior Chamber Fernando Vega, MD 1 Diagnosis and Management of Common Eye Problems Red Eye Disorders: What is not in the scope of Red Eye Possible Causes of a Red Eye n Loss of Vision n Trauma n Vitreous Floaters n Chemicals n Vitreous detatchment n Infection n Retinal detachment n Allergy n Chronic Irritation n Systemic Infections Symptoms can help determine the Symptoms Continued diagnosis Symptom Cause Symptom Cause Itching allergy Deep, intense pain Corneal abrasions, scleritis Scratchiness/ burning lid, conjunctival, corneal Iritis, acute glaucoma, sinusitis disorders, including Photophobia Corneal abrasions, iritis, acute foreign body, trichiasis, glaucoma dry eye Halo Vision corneal edema (acute glaucoma, Localized lid tenderness Hordeolum, Chalazion contact lens overwear) Diagnostic steps to evaluate the patient with Diagnostic steps continued the red eye n Check visual acuity n Estimate depth of anterior chamber n Inspect pattern of redness n Look for irregularities in pupil size or n Detect presence or absence of conjunctival reaction discharge: purulent vs serous n Look for proptosis (protrusion of the globe), n Inspect cornea for opacities or irregularities lid malfunction or limitations of eye n Stain cornea with fluorescein movement Fernando Vega, MD 2 Diagnosis and Management of Common Eye Problems How to interpret findings n Decreased visual acuity suggests a serious ocular disease.