Diagnosis and Management of Common Eye Problems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary Benchmarks for Preferred Practice Pattern® Guidelines
SUMMARY BENCHMARKS FOR PREFERRED PRACTICE PATTERN® GUIDELINES TABLE OF CONTENTS Summary Benchmarks for Preferred Practice Pattern Guidelines Introduction . 1 Glaucoma Primary Open-Angle Glaucoma (Initial Evaluation) . 3 Primary Open-Angle Glaucoma (Follow-up Evaluation) . 5 Primary Open-Angle Glaucoma Suspect (Initial and Follow-up Evaluation) . 6 Primary Angle-Closure Disease (Initial Evaluation and Therapy) . 8 Retina Age-Related Macular Degeneration (Initial and Follow-up Evaluation) . 10 Age-Related Macular Degeneration (Management Recommendations) . 11 Diabetic Retinopathy (Initial and Follow-up Evaluation) . 12 Diabetic Retinopathy (Management Recommendations) . 13 Idiopathic Epiretinal Membrane and Vitreomacular Traction (Initial Evaluation and Therapy) . 14 Idiopathic Macular Hole (Initial Evaluation and Therapy) . 15 Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration (Initial and Follow-up Evaluation) . 17 Retinal and Ophthalmic Artery Occlusions (Initial Evaluation and Therapy) . 18 Retinal Vein Occlusions (Initial Evaluation and Therapy) . 19 Cataract/Anterior Segment Cataract (Initial and Follow-up Evaluation) . 20 Cornea/External Disease Bacterial Keratitis (Initial Evaluation) . 22 Bacterial Keratitis (Management Recommendations) . 23 Blepharitis (Initial and Follow-up Evaluation) . 24 Conjunctivitis (Initial Evaluation) . 25 Conjunctivitis (Management Recommendations) . 26 Corneal Ectasia (Initial Evaluation and Follow-up) . 27 Corneal Edema and Opacification (Initial Evaluation) . 28 Corneal Edema -

Repair of Open Globe Injury
Advances in Ophthalmology & Visual System Case Report Open Access Case report: repair of open globe injury Abstract Volume 3 Issue 1 - 2015 Globe rupture is a common sight-threatening ophthalmic emergency. We present a twelve-year-old girl with ocular trauma by sharp object resulting in corneal laceration, Nader Hussein Fouad Hassan Department of Ophthalmology, Benha University Hospital, hyphema, traumatic cataract and iris prolapse. This case illustrates the importance of early Egypt diagnosis, proper wound repair of ruptured globe as well as management of post-operative complications and value of early post-operative visual rehabilitation. Correspondence: Nader Hussein Fouad Hassan, Ophthalmology department, Benha University Hospital, Keywords: globe rupture, open globe injury, corneal laceration Kaliyobeya, Egypt, Tel +201224727982, Email Received: October 16, 2015 | Published: October 19, 2015 Abbreviations: FB, foreign body; VA, visual acuity; CT scan, patient then was given tetanus immunization, antiemetics, analgesics computerized tomography; RD, retinal detachment; INR, international and intravenous broad spectrum antibiotics and prepared for globe normalized ratio; GA, general anesthesia; D, diopter rupture repair under GA. Laboratory tests included a full blood count, liver function tests, INR, prothrombin time, partial thromboplastin Introduction time, kidney function tests, all were within normal. Ruptured Globe is a common ophthalmic emergency. It is a leading cause of blindness. Early examination with high level of suspicion is recommended in any patient with ocular trauma. Many signs may obscure detection of globe rupture, so the ophthalmologist should examine the patient thoroughly and treat the patient as early as impossible including early visual rehabilitation for young patients to prevent amblyopia. Globe rupture may be associated with traumatic hyphema, traumatic cataract, lens dislocation, vitreous hemorrhage, retinal detachment, uveal prolapse, scleral wound, orbital wall fractures, or optic nerve damage. -
Aafp Fmx 2020
10/7/2020 Common Acute Eye Presentations Dr. Ahmed Mian HonBSc, BEd, MD CCFP (EM) Staff ER Consultant Department of Emergency Medicine, Humber River Hospital and University Health Network Medical Director and Chair, Medical Education HRH ED Investigative Coroner, Province of Ontario Faculty DFCM/EM University of Toronto and DFM Queens' University 1 ACTIVITY DISCLAIMER The material presented here is being made available by the American Academy of Family Physicians for educational purposes only. Please note that medical information is constantly changing; the information contained in this activity was accurate at the time of publication. This material is not intended to represent the only, nor necessarily best, methods or procedures appropriate for the medical situations discussed. Rather, it is intended to present an approach, view, statement, or opinion of the faculty, which may be helpful to others who face similar situations. The AAFP disclaims any and all liability for injury or other damages resulting to any individual using this material and for all claims that might arise out of the use of the techniques demonstrated therein by such individuals, whether these claims shall be asserted by a physician or any other person. Physicians may care to check specific details such as drug doses and contraindications, etc., in standard sources prior to clinical application. This material might contain recommendations/guidelines developed by other organizations. Please note that although these guidelines might be included, this does not necessarily imply the endorsement by the AAFP. 2 2 1 10/7/2020 Disclosure It is the policy of the AAFP that all individuals in a position to control content disclose any relationships with commercial interests upon nomination/invitation of participation. -

Endogenous Brucella Endophthalmitis: a Case Report
Saudi Journal of Ophthalmology (2017) xxx, xxx–xxx Case Report Endogenous Brucella endophthalmitis: A case report ⇑ Merih Oray a, ; Zafer Cebeci a; Nur Kir a; Banu Turgut Ozturk b; Lutfiye Oksuz c; Ilknur Tugal-Tutkun a Abstract Brucellosis may be associated with a wide range of ophthalmic manifestations including endophthalmitis, which is a sight- threatening condition that needs to be rapidly recognized and treated to avoid permanent visual loss. A 26-year-old female with a 6-month history of vision loss in the left eye was treated with high dose systemic corticosteroids and azathioprine with an initial misdiagnosis elsewhere. A dense vitreous haze with opacities at the posterior hyaloid and a wide area of retinochoroiditis led to the diagnosis of endogenous endophthalmitis at presentation to us. The vitreous sample and blood cultures demonstrated growth of Brucella melitensis. She received 6 months of systemic antibiotherapy, which resulted in resolution of inflammation; however, visual acuity remained poor due to irreversible damage. Infectious etiology, including brucellosis in endemic countries, has to be considered in the differential diagnosis before administering immunomodulatory therapy in patients with panuveitis of unknown origin. Keywords: Endogenous endophthalmitis, Ocular brucellosis, Panuveitis Ó 2017 The Authors. Production and hosting by Elsevier B.V. on behalf of Saudi Ophthalmological Society, King Saud University. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/). http://dx.doi.org/10.1016/j.sjopt.2017.03.002 Introduction We herein present an unusual case of endogenous endophthalmitis due to B. melitensis. Brucellosis (Malta fever) is a zoonotic systemic disease caused by Brucella melitensis or Brucella abortus. -

URGENT/EMERGENT When to Refer Financial Disclosure
URGENT/EMERGENT When to Refer Financial Disclosure Speaker, Amy Eston, M.D. has a financial interest/agreement or affiliation with Lansing Ophthalmology, where she is employed as a ophthalmologist. 58 yr old WF with 6 month history of decreased vision left eye. Ache behind the left eye for 2-3 months. Using husband’s contact lens solution made it feel better. Seen by two eye care professionals. Given glasses & told eye exam was normal. No past ocular history Medical history of depression Takes only aspirin and vitamins 20/20 OD 20/30 OS Eye Pressure 15 OD 16 OS – normal Dilated fundus exam & slit lamp were normal Pupillary exam was normal Extraocular movements were full Confrontation visual fields were full No red desaturation Color vision was slightly decreased but the same in both eyes Amsler grid testing was normal OCT disc – OD normal OS slight decreased RNFL OCT of the macula was normal Most common diagnoses: Dry Eye Optic Neuritis Treatment - copious amount of artificial tears. Return to recheck refraction Visual field testing Visual Field testing - Small defect in the right eye Large nasal defect in the left eye Visual Field - Right Hemianopsia. MRI which showed a subacute parietal and occipital lobe infarct. ANISOCORIA Size of the Pupil Constrictor muscles innervated by the Parasympathetic system & Dilating muscles innervated by the Sympathetic system The Sympathetic System Begins in the hypothalamus, travels through the brainstem. Then through the upper chest, up through the neck and to the eye. The Sympathetic System innervates Mueller’s muscle which helps to elevate the upper eyelid. -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -
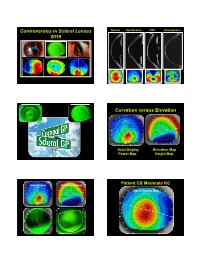
Controversies in Scleral Lenses 2019 Curvature Versus Elevation
Controversies in Scleral Lenses Normal Keratoconus PMD Keratoglobus 2019 Curvature versus Elevation Axial Display Elevation Map Power Map Height Map Axial Display Elevation Display Patient CB Moderate KC Axial Display Map +180um +180 +379 +379um Elevation Display -110 - 276 Elevation Map 655 Above the 290 microns Micron Sphere Height -276um Differential Depression Below the -110um Sphere N = 87 Patients 127 CL Fits Less than 350um Greater than 350um Patients with 350um or less of corneal elevation difference (along the greatest meridian of change) have an 88.2% chance of success with a corneal GP lens. The Re-Birth of Scleral Lenses Glass Scleral Lenses 1887 Molding Glass Scleral Lenses Average 8.5 High DK Scleral Materials Traditional Corneal / Scleral • Menicon Z Dk = 163 Shape • B & L, Boston XO2 DK = 141 • Contamac, Optimum Extreme DK = 125 • B & L, Boston XO DK = 100 • Paragon HDS 100 DK = 100 • Contamac, Optimum Extra DK = 100 • Lagado, Tyro -97 DK = 97 Scleral Shape Cone Angle Circa 1948 Klaus Pfortner New Understandings Argentina Scleral Lens Fitting Objectives Anatomy of a Scleral Lens 1. Central Vault Zone (250 to 400 microns) 2. Peripheral Lift Zone 4 3 2 1 2 3 4 3. Limbal Lift Zone 4. Scleral Landing Zone Ocular Surface Disease Scleral Lens Indications Scleral Irregular Astigmatism Lens • Keratoconus Indications • Pellucid Marginal Degeneration • Post Corneal Trauma • Post keratoplasty • Post K-Pro • Post Refractive Surgery RK, PRK and LASIK • Post HSV and HZV • Athletes • GP stability (rocking) issues Corneal Irregularity -

Chalazion Treatment
Chalazion Treatment This material will help you understand treatments for chalazion. What is a chalazion? A chalazion is a red, tender lump in the eyelid. It is also known as a stye. The swelling occurs because one of the oil glands that is next to each eyelash can get backed up and become inflamed. This is very similar to a pimple. How is a chalazion treated? In many cases, chalazia resolve on their own without treatment. Applying a warm compress over your eye for 5- 10 minutes two to four times a day can soften the oil that is backed up. This helps the chalazion heal. If the chalazion does not heal after one month of using warm compresses, your doctor may suggest surgical removal or injection with medications to help it heal faster. How is a chalazion surgically removed? Surgical removal of a chalazion is an outpatient procedure. Before the procedure, your doctor will give you a local anesthetic to numb the area around the chalazion. Next, your doctor will place a clamp to help hold your eyelid in place for the procedure. That way, you will not need to worry about keeping your eyelid open for the procedure. The doctor will then make a small incision in the eyelid and remove the chalazion with a special instrument. The location of the incision (front or back of the eyelid) depends on the size of the chalazion. Small chalazia can be removed by making an incision on the inside of the eyelid. If your chalazion is large, the doctor may make an incision on the front of the eyelid and close it with dissolvable stitches. -

The Simplified Trachoma Grading System, Amended Anthony W Solomon,A Amir B Kello,B Mathieu Bangert,A Sheila K West,C Hugh R Taylor,D Rabebe Tekeraoie & Allen Fosterf
PolicyPolicy & practice & practice The simplified trachoma grading system, amended Anthony W Solomon,a Amir B Kello,b Mathieu Bangert,a Sheila K West,c Hugh R Taylor,d Rabebe Tekeraoie & Allen Fosterf Abstract A simplified grading system for trachoma was published by the World Health Organization (WHO) in 1987. Intended for use by non-specialist personnel working at community level, the system includes five signs, each of which can be present or absent in any eye: (i) trachomatous trichiasis; (ii) corneal opacity; (iii) trachomatous inflammation—follicular; (iv) trachomatous inflammation—intense; and (v) trachomatous scarring. Though neither perfectly sensitive nor perfectly specific for trachoma, these signs have been essential tools for identifying populations that need interventions to eliminate trachoma as a public health problem. In 2018, at WHO’s 4th global scientific meeting on trachoma, the definition of one of the signs, trachomatous trichiasis, was amended to exclude trichiasis that affects only the lower eyelid. This paper presents the amended system, updates its presentation, offers notes on its use and identifies areas of ongoing debate. Introduction (ii) corneal opacity; (iii) trachomatous inflammation—fol- licular; (iv) trachomatous inflammation—intense; and (v) tra- Trachoma is the most important infectious cause of blindness.1 chomatous scarring.19 Trachomatous inflammation—follicular Repeated conjunctival infection2 with particular strains of and trachomatous inflammation—intense are signs of active Chlamydia trachomatis3–5 -

Ophthalmic Management of Facial Nerve Palsy
Eye (2004) 18, 1225–1234 & 2004 Nature Publishing Group All rights reserved 0950-222X/04 $30.00 www.nature.com/eye 1 2 3 Ophthalmic V Lee , Z Currie and JRO Collin REVIEW management of facial nerve palsy Abstract The facial nerve travels with the eighth cranial nerve through the internal auditory canal and The ophthalmologist plays a pivotal role in the through the internal fallopian canal in the evaluation and rehabilitation of patients with petrous temporal bone for the longest facial nerve palsy. It is crucial to recognize and interosseus course of any cranial nerve (30 mm). treat the potentially life-threatening The fibres for the pterygopalatine ganglion underlying causes. The immediate ophthalmic leave at the geniculate ganglion as the greater priority is to ensure adequate corneal superficial petrosal nerve. The nerve to the protection. The medium to long-term stapedius and the chorda tympani (innervation management consists of treatment of epiphora, to the salivary glands) leave prior to the nerve hyperkinetic disorders secondary to aberrant exiting through the stylomastoid foramen as a regeneration and poor cosmesis. Patients purely motor nerve to the muscles of facial should be appropriately referred for general expression.2 Within the substance of the parotid 1 facial re-animation. This review aims to Central Eye Service gland, it divides into the five main Central Middlesex Hospital provide a guide to the management of this branchesFthe temporal, zygomatic, buccal, Acton Lane complex condition. Park Royal mandibular, and cervical branches. Facial nerve Eye (2004) 18, 1225–1234. doi:10.1038/sj.eye.6701383 Acton London, UK lesions above the geniculate ganglion classically Published online 16 April 2004 cause more severe ophthalmic symptoms 2Department of because lacrimal secretion and orbicularis Keywords: gold weight; tarsorrhapy; facial Ophthalmology closure are involved. -

Pterygium & Pinguecula
Dr. Anthony O. Roberts 9715 Medical Center Drive Pterygium & Pinguecula Suite 502 Rockville, MD 20850 A pterygium is a mass of fleshy tissue that Phone: 301-279-0600 E-mail: [email protected] grows over the cornea (the clear front window of the eye). It may remain small or may grow large enough to interfere with vision. A ptery- gium most commonly occurs on the inner cor- Eye Care Services ner of the eye, but it can appear on the outer Eye Exams corner as well. Glaucoma Testing & The exact cause of pterygia is not well understood. They occur more often Treatment in people who spend a lot of time outdoors, especially in sunny climates. Cataract Surgery Long-term exposure to sunlight, especially to ultraviolet (UV) rays, and Diabetic Evaluation chronic eye irritation from dry, dusty conditions seem to play an important LASIK Eye Surgery role. Dry eye also may contribute to pterygium. PRK Surgery Refractive Procedures When a pterygium becomes red and irritated, eyedrops or ointments can be used to help reduce the inflammation. If the pterygium grows rapidly or is Our Practice large enough to threaten sight, it can be removed surgically. At Shady Grove Ophthal- mology, we understand the Despite proper surgical removal, a pterygium may return, particularly in importance of your vision. young people. Protecting the eyes from excessive ultraviolet light with We are committed to offering proper sunglasses, avoiding dry, dusty conditions, and using artificial tears the highest quality eye care can also help. using the most state-of-the- art technologies. Dr. An- thony Roberts delivers pre- A pinguecula is a yellowish patch or bump on the white of the eye, most mium quality eye care and often on the side closest to the nose. -

Epstein Barr Virus Dacryoadenitis Resulting in Keratoconjunctivitis Sicca in a Child
Epstein Barr Virus Dacryoadenitis Resulting in Keratoconjunctivitis Sicca in a Child C. Stephen Foster, M.D. We evaluated a 10 year-old male with bilateral severe dry eye who was profoundly disabled by pain and photophobia despite aggressive conventional lubricant and tear conservation therapy. Serologic studies were initially unrevealing and misleading. A lacrimal gland biopsy, orbital portion, left side, was performed, and tissue was processed for light and immunohistochemical studies, which enabled us to establish the diagnosis. The boy, six months prior to evaluation, had been swimming in a river in Arkansas with friends, and all developed "conjunctivitis" after this outing, but only the patient's ocular symptoms persisted, with bilateral lid swelling, conjunctival injection, and ocular discomfort. Viral conjunctivitis was diagnosed and treated with topical tobramycin and dexamethasone four times daily for two weeks without effect. Increasingly severe superficial punctate keratopathy developed, and Pred Forte every two hours and Decadron ointment at bedtime along with Ciloxan drops every four hours and lubricants were prescribed. Three weeks of this therapy was also not effective in reducing the signs and symptoms. Schirmer values were zero bilaterally, cornea sensitivity was normal bilaterally, and all cultures were negative. Serologic studies disclosed elevated alkaline phosphatase and aspartate aminotransferase, and serum angiotensin converting enzyme determination was elevated and gallium scanning disclosed abnormal uptake of gallium citrate in the parotid and lacrimal glands. All other studies were within normal limits, and HLA typing was not diagnostically helpful. The diagnosis of sarcoidosis was made, and the patient was treated with systemic Prednisone, 100 mg PO QD, without noticeable effect on the ocular signs and symptoms.