Sclera, Choroid, Retina, Oh My! AMIEE HO, OD, FAAO PACIFIC UNIVERSITY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Peripapillary Retinal Vascular Involvement in Early Post-COVID-19 Patients
Journal of Clinical Medicine Article Peripapillary Retinal Vascular Involvement in Early Post-COVID-19 Patients 1,2, 1,2, 1,2, Alfonso Savastano y , Emanuele Crincoli y , Maria Cristina Savastano * , Saad Younis 3, Gloria Gambini 1,2, Umberto De Vico 1,2 , Grazia Maria Cozzupoli 1,2 , Carola Culiersi 1,2 , Stanislao Rizzo 1,2,4 and Gemelli Against COVID-19 Post-Acute Care Study Group 2 1 Ophthalmology Unit, Fondazione Policlinico Universitario A. Gemelli IRCCS, 00196 Rome, Italy; [email protected] (A.S.); [email protected] (E.C.); [email protected] (G.G.); [email protected] (U.D.V.); [email protected] (G.M.C.); [email protected] (C.C.); [email protected] (S.R.) 2 Department of Ophthalmology, Catholic University of “Sacro Cuore”, 00168 Rome, Italy 3 Department of Ophthalmology, Western Eye Hospital, Imperial College Healthcare NHS Trust, London NW1 5QH, UK; [email protected] 4 Neuroscience Institute, Consiglio Nazionale delle Ricerche, Istituto di Neuroscienze, 56124 Pisa, Italy * Correspondence: [email protected]; Tel.: +39-063-015-4928 These authors contributed equally to this work. y Received: 5 August 2020; Accepted: 3 September 2020; Published: 8 September 2020 Abstract: The ability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-20s) to cause multi-organ ischemia and coronavirus-induced posterior segment eye diseases in mammals gave concern about potential sight-threatening ischemia in post coronavirus disease 2019 patients. The radial peripapillary capillary plexus (RPCP) is a sensitive target due to the important role in the vascular supply of the peripapillary retinal nerve fiber layer (RNFL). -
Controversies in Scleral Lenses 2019 Curvature Versus Elevation
Controversies in Scleral Lenses Normal Keratoconus PMD Keratoglobus 2019 Curvature versus Elevation Axial Display Elevation Map Power Map Height Map Axial Display Elevation Display Patient CB Moderate KC Axial Display Map +180um +180 +379 +379um Elevation Display -110 - 276 Elevation Map 655 Above the 290 microns Micron Sphere Height -276um Differential Depression Below the -110um Sphere N = 87 Patients 127 CL Fits Less than 350um Greater than 350um Patients with 350um or less of corneal elevation difference (along the greatest meridian of change) have an 88.2% chance of success with a corneal GP lens. The Re-Birth of Scleral Lenses Glass Scleral Lenses 1887 Molding Glass Scleral Lenses Average 8.5 High DK Scleral Materials Traditional Corneal / Scleral • Menicon Z Dk = 163 Shape • B & L, Boston XO2 DK = 141 • Contamac, Optimum Extreme DK = 125 • B & L, Boston XO DK = 100 • Paragon HDS 100 DK = 100 • Contamac, Optimum Extra DK = 100 • Lagado, Tyro -97 DK = 97 Scleral Shape Cone Angle Circa 1948 Klaus Pfortner New Understandings Argentina Scleral Lens Fitting Objectives Anatomy of a Scleral Lens 1. Central Vault Zone (250 to 400 microns) 2. Peripheral Lift Zone 4 3 2 1 2 3 4 3. Limbal Lift Zone 4. Scleral Landing Zone Ocular Surface Disease Scleral Lens Indications Scleral Irregular Astigmatism Lens • Keratoconus Indications • Pellucid Marginal Degeneration • Post Corneal Trauma • Post keratoplasty • Post K-Pro • Post Refractive Surgery RK, PRK and LASIK • Post HSV and HZV • Athletes • GP stability (rocking) issues Corneal Irregularity -

Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission
Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission The use of oral doxycycline and vitamin C in the management of acute corneal hydrops: a case comparison Abstract- We compare two patients presenting to clinic with an uncommon complication of keratoconus, acute corneal hydrops. Management of the patients differs. One heals quickly, while the other has a delayed course to resolution. I. Case A a. Demographics: 40 yo AAM b. Case History i. CC: red eye, tearing, decreased VA x 1 day OS ii. POHx: (+) keratoconus OU iii. PMHx: depression, anxiety, asthma iv. Meds: Albuterol, Ziprasidone v. Scleral CL wearer for approximately 6 months OU vi. Denies any pain OS, denies previous occurrence OU, no complaints OD c. Pertinent Findings i. VA cc (CL’s)- 20/25 OD, 20/200 PH 20/60+2 OS ii. Slit Lamp 1. Inferior corneal thinning and Fleisher ring OD, central scarring OD, 2+ diffuse microcystic edema OS, Descemet’s break OS (photos and anterior segment OCT) 2. 2+ diffuse injection OS 3. D&Q A/C OU iii. Intraocular Pressures: deferred OD due to CL, 9mmHg OS (tonopen) iv. Fundus Exam- unremarkable OU II. Case B a. Demographics: 39 yo AAM b. Case History i. CC: painful, red eye, tearing, decreased VA x 1 day OS ii. POHx: unremarkable iii. PMHx: hypertension iv. Meds: unknown HTN medication v. Wears Soflens toric CL’s OU; reports previous doctor had difficulty achieving proper fit OU; denies diagnosis of keratoconus OU vi. Denies any injury OS, denies previous occurrence OU, no complaints OD c. -

Smoking and Eye Disease
Smoking and Eye Disease Here are some eye problems that are made worse Smoking and eye disease by smoking: Smoking tobacco (cigarettes, cigars or pipes) can cause lung disease, heart disease, cancer, and Dry eye. This is when your eyes do not have many other serious health problems. But did you enough—or the right kind of—tears. Smoking know that smoking can also harm your eyes? with dry eye will make your eyes more likely to feel scratchy, sting, burn or be red. Eye Words to Know Cataracts. If you smoke you are at increased risk for getting cataracts. A cataract is clouding of Retina: Layer of nerve cells lining the back your eye’s naturally clear lens. It causes blurry wall inside the eye. This layer senses light and vision and makes colors look dull, faded or sends signals to the brain so you can see. yellowish. Cataracts are removed in surgery. Macula: Small but important area in the center of the retina. You need the macula to Age-related macular degeneration (AMD). This clearly see details of objects in front of you. disease happens when a part of the retina called the macula is damaged. You lose your central Lens: Clear part of the eye behind the colored vision and cannot see fine details. But your iris. It helps to focus light on the retina (back peripheral (side) vision stays normal. Sometimes of the eye) so you can see. medicine or surgery can help certain people with Optic nerve: A nerve at the back of your AMD from getting worse. -

Pterygium & Pinguecula
Dr. Anthony O. Roberts 9715 Medical Center Drive Pterygium & Pinguecula Suite 502 Rockville, MD 20850 A pterygium is a mass of fleshy tissue that Phone: 301-279-0600 E-mail: [email protected] grows over the cornea (the clear front window of the eye). It may remain small or may grow large enough to interfere with vision. A ptery- gium most commonly occurs on the inner cor- Eye Care Services ner of the eye, but it can appear on the outer Eye Exams corner as well. Glaucoma Testing & The exact cause of pterygia is not well understood. They occur more often Treatment in people who spend a lot of time outdoors, especially in sunny climates. Cataract Surgery Long-term exposure to sunlight, especially to ultraviolet (UV) rays, and Diabetic Evaluation chronic eye irritation from dry, dusty conditions seem to play an important LASIK Eye Surgery role. Dry eye also may contribute to pterygium. PRK Surgery Refractive Procedures When a pterygium becomes red and irritated, eyedrops or ointments can be used to help reduce the inflammation. If the pterygium grows rapidly or is Our Practice large enough to threaten sight, it can be removed surgically. At Shady Grove Ophthal- mology, we understand the Despite proper surgical removal, a pterygium may return, particularly in importance of your vision. young people. Protecting the eyes from excessive ultraviolet light with We are committed to offering proper sunglasses, avoiding dry, dusty conditions, and using artificial tears the highest quality eye care can also help. using the most state-of-the- art technologies. Dr. An- thony Roberts delivers pre- A pinguecula is a yellowish patch or bump on the white of the eye, most mium quality eye care and often on the side closest to the nose. -

Gibberman – Advances in Scleral Lens Technology
ADVANCES IN SCLERAL LENS TECHNOLOGY ALEX GIBBERMAN, OD, FAAO, FSLS 2020 EYECARE, LOVELAND, OHIO A BRIEF HISTORY OF THE WORLD…OF SCLERALS 16th century- Da Vinci concepts. Blown glass shell. No power. 1887-Muller brothers. Thinner blown glass shells 1888- Adolf Fick. Glass lenses first to treat k conus with correction. First to note corneal edema 1889- Dr. Kirstein is born! Also August Muller is first to use scleral to correct for high myopia HISTORY CONTINUED… 1890’s- The use of saline with scleral insertion is introduced 1912- Zeiss makes first diagnostic fitting set Also notable in 1912, Dr Zelczak is born! 1957-PMMA sclerals introduced. 1970s-John James Little and Arthur Irving first to use RGP sclerals 1983-RGP scleral materials updated by optometrist Don Ezekiel MODERN SCLERALS Between the mid 1980s and now, significant material and dk improvements have occurred. Late 1980s- Back toric optics were introduced to sclerals 1992- the first impression based, computer scanned and created lens was made in the UK 2013-EyePrintPro was developed to take an impression and match exact contour of the eye Current- multifocal optics, decentered optics, front toric and back toric optics, prism and higher order aberration correction are all possible Scleral topographers: Getting us closer to empirical fitting. We will discuss in more detail SPECIFICATIONS OF A MODERN SCLERAL LENS? Here is just one example Base Curve 7.50 Diameter 16.1 mm Sagittal Depth: 3500um Toric Peripheral curve, flatten horizontal meridian 100um steepen vertical meridian 200um Front toric overall power -400 -125 x 105 Multifocal Center ADD 2.5mm Zone +250 ADD Nasal microvault or notch to avoid pinguecula Material: Optimum Infinite Dk 200 needs hydropeg coating WHAT A CURRENT SCLERAL LOOKS LIKE SCLERAL TOPOGRAPHERS Eaglet- Eye surface profiler Pentacam- CSP Visionary Optics-Smap3D Latitude Focal Points Focal Points will allow the import of multiple types of scleral topography files such as Eaglet ESP, Pentacam CSP and sMap. -
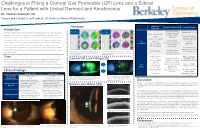
Lens for a Patient with Limbal Dermoid and Keratoconus
Challenges in Fitting a Corneal Gas Permeable (GP) Lens and a Scleral Lens for a Patient with Limbal Dermoid and Keratoconus By: Vakishan Nadarajah, OD Cornea and Contact Lens Resident, UC Berkeley School of Optometry Initial Lens Pentacam Initial Lens Evaluation Lens Modifications Introduction Parameters Moderate apical Right Eye: Left Eye: Flattened BC to 7.30 Limbal dermoids are benign congenital tumors containing histological tissue such as epidermal clearance & small – appendages, teeth, or bone. If enlarged, they can cause amblyopia due to induced corneal OAD: 8.8mm, BC: central bubbles Decreased apical 7.20 (Figure 5a) astigmatism. Keratoconus is an ocular disease that causes irregularity from progressive corneal clearance, but small Power: -7.75DS insertion bubble still thinning. Corneal GPs and scleral lenses are non-surgical devices indicated to improve vision Mid-peripheral OD OZ: 6.4 present for such irregular corneas by providing an optically regular surface for light to refract through. bearing temporally due Corneal GP (Figure 5b) SCr: 8.6/0.6 to inferonasal However, it is much more difficult to fit lenses for patients with both irregular corneas and PCr: 10.5/0.4 decentration Patient reported irregular conjunctivas. Fortunately, these gas permeable lenses can be altered in size and fit to improved comfort and provide optimal vision. This case outlines techniques to best fit a patient with irregular corneas Adequate edge Figure 3) Pentacam analysis shows mild keratoconus Figure 4) Pentacam analysis shows severe keratoconus -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -

The Red Eye Differential Diagnosis Differential Diagnosis of “Red Eye”
The Red Eye Differential Diagnosis Differential Diagnosis of “red eye” Conjunctiva Pupil Cornea Anterior IOP chamber Subconjunctival Bright red Normal Normal Normal Normal Haemorrhage Conjunctivitis Injected Normal Normal Normal Normal vessels, fornices. Discharge Iritis Injected Small, Normal, Turgid, Normal around cornea fixed, KPs deep irregular Acute glaucoma Entire eye red Fixed, Hazy Shallow High dilated, oval Conjunctivitis Papillae Follicles Purulent discharge Redness Chemosis Subconjunctival Haemorrhage • Diffuse or localised area of blood under conjunctiva. Asymptomatic • Idiopathic, trauma, cough, sneezing, aspirin, HT • Resolves within 10-14 days Dry Eye Syndrome • Poor quality – Meibomian gland disease,Acne rosacea – Lid related – Vitamin A deficiency • Poor quantity –KCS • Sjogren Syndrome • Rheumatoid Arthritis – Lacrimal disease ie, Sarcoidosis – Paralytic ie, VII CN palsy Corneal Abrasion • Surface epithelium sloughed off. • Stains with fluorescein • Usually due to trauma • Pain, FB sensation, tearing, red eye Corneal Ulcer • Infection – Bacterial: Adnexal infection, lid malposition, dry eye, CL – Viral: HSV, HZO – Fungal: –Protozoan:Acanthamoeba in CL wearer • Mechanical or trauma • Chemical: Alkali injuries are worse than acid Episcleritis • Superficial • Idiopathic, collagen vascular disorder (RA) • Asymptomatic, mild pain • Self-limiting or topical treatment Scleritis •Deep • Idiopathic • Collagen vascular disease (RA,AS, SLE, Wegener, PAN) • Zoster • Sarcoidosis • Dull, deep pain wakes patient at night • Systemic -

Canine Red Eye Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO
PEER REVIEWED Clinical Approach to the CANINE RED EYE Elizabeth Barfield Laminack, DVM; Kathern Myrna, DVM, MS; and Phillip Anthony Moore, DVM, Diplomate ACVO he acute red eye is a common clinical challenge for tion of the deep episcleral vessels, and is characterized general practitioners. Redness is the hallmark of by straight and immobile episcleral vessels, which run Tocular inflammation; it is a nonspecific sign related 90° to the limbus. Episcleral injection is an external to a number of underlying diseases and degree of redness sign of intraocular disease, such as anterior uveitis and may not reflect the severity of the ocular problem. glaucoma (Figures 3 and 4). Occasionally, episcleral Proper evaluation of the red eye depends on effective injection may occur in diseases of the sclera, such as and efficient diagnosis of the underlying ocular disease in episcleritis or scleritis.1 order to save the eye’s vision and the eye itself.1,2 • Corneal Neovascularization » Superficial: Long, branching corneal vessels; may be SOURCE OF REDNESS seen with superficial ulcerative (Figure 5) or nonul- The conjunctiva has small, fine, tortuous and movable vessels cerative keratitis (Figure 6) that help distinguish conjunctival inflammation from deeper » Focal deep: Straight, nonbranching corneal vessels; inflammation (see Ocular Redness algorithm, page 16). indicates a deep corneal keratitis • Conjunctival hyperemia presents with redness and » 360° deep: Corneal vessels in a 360° pattern around congestion of the conjunctival blood vessels, making the limbus; should arouse concern that glaucoma or them appear more prominent, and is associated with uveitis (Figure 4) is present1,2 extraocular disease, such as conjunctivitis (Figure 1). -

Ryan P. Ames, OD, MBA the Chief Complaint Drives the Bus December 2019 This Is One of the Fundamental Concepts in Patient Driv
Ryan P. Ames, OD, MBA [email protected] 888.456.2046 The Chief Complaint Drives the Bus December 2019 This is one of the fundamental concepts in patient driven care and in proper documentation. Nearly every day we see a patient, one will come in complaining of one thing, and we will discover a completely different condition that we feel is more important. They may not even have symptoms of this new condition. The Chief Complaint (CC) or Reason for Visit (RFV) can certainly be doctor directed from a prior visit. But the concept is the same, whether the CC/RFV is doctor directed or patient driven, this is the condition that will become the primary diagnosis. Remember, auditors are often employed by third-party companies and they derive their revenue based on a percentage of what they recover. Therefore, they are going to look for low-hanging fruit that has a high potential for recoupment of payment. The CC/RFV is a very easily identified element of the exam and if the primary diagnosis does not address it, they could deem the entire encounter unnecessary and recoup the payment. The other day I saw a long-time patient with no prior medical diagnosis except a pinguecula. He also had no visual complaints. He came in saying, “I think those white bumps are getting bigger and are sometimes red.” On exam, the vision in his right eye was slightly reduced to 20/25- with no improvement after refraction. During the retinal exam, her appeared to have mild epiretinal membranes and the OCT confirmed that finding.