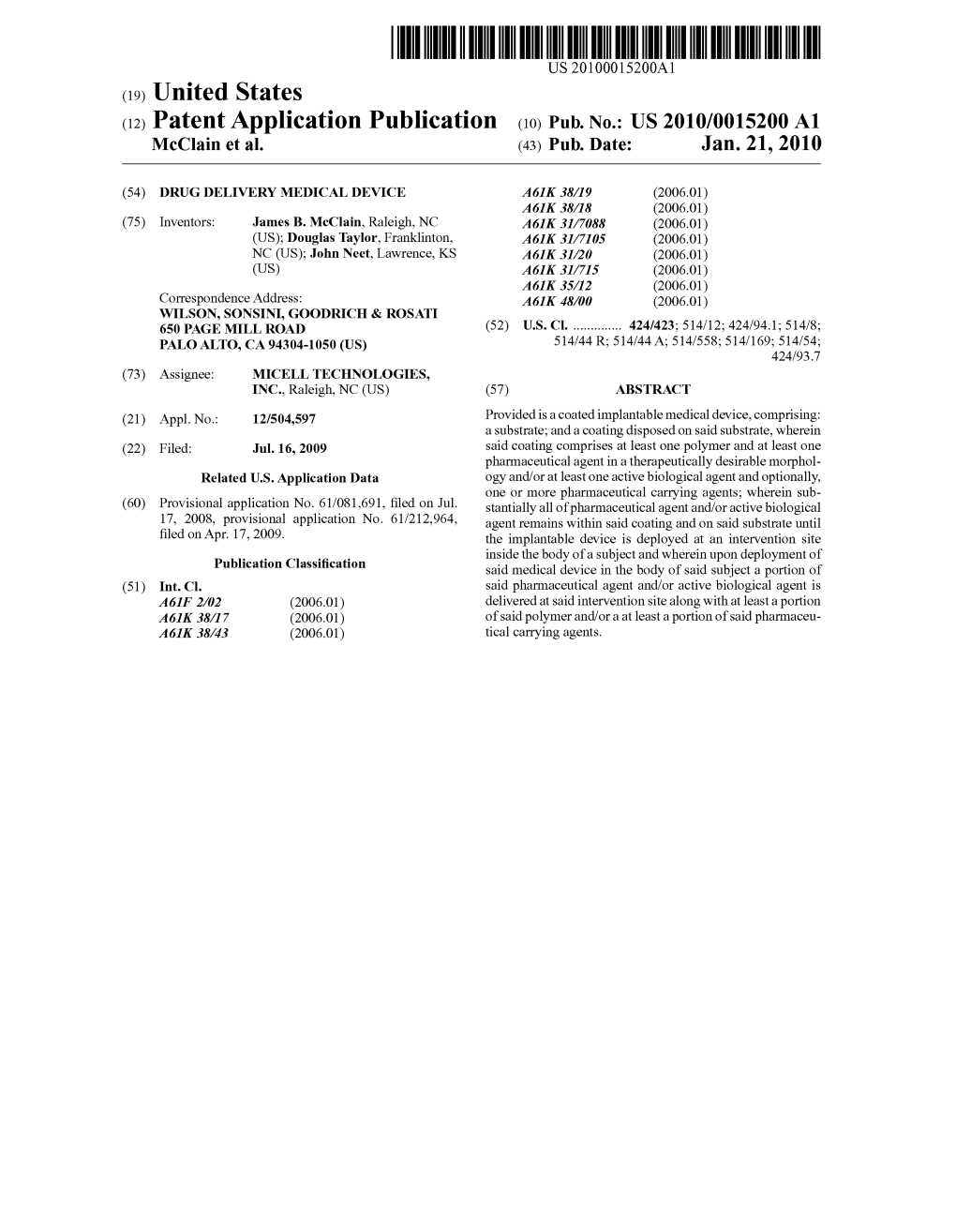
(12) Patent Application Publication (10) Pub. No.: US 2010/0015200 A1 Mcclain Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Herbal Contraindications & Drug Interactions
Herbal Contraindications & Drug Interactions plus Herbal Adjuncts with Medicines FOURTH EDITION, 2010 © by Francis Brinker, N.D. References 1. Sherman JA (comp.). The Complete Botanical Prescriber, 2nd ed. National College of Naturopathic Medicine, Portland, Ore., 1979 2. Brinker F. The Toxicology of Botanical Medicines, 3rd ed. Eclectic Medical Pub., Sandy, Ore., 2000 3. Brinker F. “Botanical Medicine Research Summaries,” from Eclectic Dispensatory of Botanical Therapeutics, vol. II. Eclectic Medical Pub., Sandy, Ore., 1995 4. Wichtl M (ed.). Herbal Drugs and Phytopharmaceuticals. CRC Press, Boca Raton, 1994 5. Felter HW, Lloyd JU. King’s American Dispensatory [1898]. Eclectic Medical Pub., Sandy, Ore., 1993 6. De Smet PAGM et al. (eds.). Adverse Effects of Herb Drugs 2. Springer-Verlag, Berlin, 1993 7. Lust J. The Herb Book. Bantam Books, New York, 1974 8. Boyd JR (ed.-in-chief). Facts and Comparisons. J.B. Lippincott Co., St. Louis, Miss., 1985 9. Ruddiman EA. Incompatibilities in Prescriptions. John Wiley & Sons, Inc., New York, 1925 10. Lewis WH, Elvin-Lewis MPF. Medical Botany. John Wiley & Sons, New York, 1977 11. Gibelli C. The hemostatic action of Equisetum. Arch. intern. pharmacodynamie, 41:419-429, 1931 (Chem. Abs. 26:6019) 12. Gutierrez RMP, Laguna GY, Walkowski, A. diuretic activity of Mexican Equisetum. J. Ethnopharm., 14:269- 272, 1985 13. Lepor H. Nonoperative management of benign prostatic hyperplasia. J. Urol., 141:1283-1289, 1989 14. Albert-Puleo M. Fennel and anise as estrogenic agents. J. Ethnopharm., 2:337-344, 1980 15. Albert-Puleo M. Mythobotany, pharmacology, and chemistry of thujone-containing plants and derivatives. Econ. Bot., 32:65-74, 1978 16. -

Front Matter
zpt0040800SPC1.qxd 3/11/08 10:55 AM Page 1 Volume 325 ■ Number 1 ■ April 2008 ■ ISSN 0022-3565 The Journal of PHARMACOLOGY And Experimental Therapeutics A Adaptations (Network Architecture) Can Create Unpredicted Therapeutic Actions Drug Predicted Effect Unexpected Effect B Complexity Creates Unpredicted Targets Predicted Effect Drug Target Unpredicted Target A Publication of the American Society for Pharmacology and Experimental Therapeutics Edited for the Society by Rick G. Schnellmann The Journal of PHARMACOLOGY And Experimental Therapeutics A Publication of the American Society for Pharmacology and Experimental Therapeutics April 2008 Vol. 325, No. 1 Contents PERSPECTIVES IN PHARMACOLOGY Exploiting Complexity and the Robustness of Network Marc K. Hellerstein 1 Architecture for Drug Discovery BEHAVIORAL PHARMACOLOGY Early Postnatal Stress Alters Place Conditioning to Both - and Clifford C. Michaels and Stephen G. Holtzman 313 -Opioid Agonists CARDIOVASCULAR □  S Design of Mutant 2 Subunits as Decoy Molecules to Reduce the Sabine Te´le´maque, Swapnil Sonkusare, 37 ,Expression of Functional Ca2؉ Channels in Cardiac Cells Terrie Grain, Sung W. Rhee, Joseph R. Stimers Nancy J. Rusch, and James D. Marsh Sphingosine 1-Phosphate Inhibits Nitric Oxide Production Takuji Machida, Yukihiro Hamaya, 200 Induced by Interleukin-1 in Rat Vascular Smooth Muscle Cells Sachiko Izumi, Yumika Hamaya, Kenji Iizuka, Yasuyuki Igarashi, Masaru Minami, Roberto Levi, and Masahiko Hirafuji Andrographolide Up-Regulates Cellular-Reduced Glutathione Anthony Y. H. Woo, Mary M. Y. Waye, 226 Level and Protects Cardiomyocytes against Stephen K. W. Tsui, Sandy T. W. Yeung, and Hypoxia/Reoxygenation Injury Christopher H. K. Cheng Orally Available Levosimendan Dose-Related Positive Inotropic Satoshi Masutani, Heng-Jie Cheng, 236 and Lusitropic Effect in Conscious Chronically Instrumented Minja Hyttila¨-Hopponen, Jouko Levijoki, Normal and Heart Failure Dogs Aira Heikkila¨, Arja Vuorela, William C. -

Treatment Protocol Copyright © 2018 Kostoff Et Al
Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al PREVENTION AND REVERSAL OF ALZHEIMER'S DISEASE: TREATMENT PROTOCOL by Ronald N. Kostoffa, Alan L. Porterb, Henry. A. Buchtelc (a) Research Affiliate, School of Public Policy, Georgia Institute of Technology, USA (b) Professor Emeritus, School of Public Policy, Georgia Institute of Technology, USA (c) Associate Professor, Department of Psychiatry, University of Michigan, USA KEYWORDS Alzheimer's Disease; Dementia; Text Mining; Literature-Based Discovery; Information Technology; Treatments Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al CITATION TO MONOGRAPH Kostoff RN, Porter AL, Buchtel HA. Prevention and reversal of Alzheimer's disease: treatment protocol. Georgia Institute of Technology. 2018. PDF. https://smartech.gatech.edu/handle/1853/59311 COPYRIGHT AND CREATIVE COMMONS LICENSE COPYRIGHT Copyright © 2018 by Ronald N. Kostoff, Alan L. Porter, Henry A. Buchtel Printed in the United States of America; First Printing, 2018 CREATIVE COMMONS LICENSE This work can be copied and redistributed in any medium or format provided that credit is given to the original author. For more details on the CC BY license, see: http://creativecommons.org/licenses/by/4.0/ This work is licensed under a Creative Commons Attribution 4.0 International License<http://creativecommons.org/licenses/by/4.0/>. DISCLAIMERS The views in this monograph are solely those of the authors, and do not represent the views of the Georgia Institute of Technology or the University of Michigan. This monograph is not intended as a substitute for the medical advice of physicians. The reader should regularly consult a physician in matters relating to his/her health and particularly with respect to any symptoms that may require diagnosis or medical attention. -

Tanibirumab (CUI C3490677) Add to Cart
5/17/2018 NCI Metathesaurus Contains Exact Match Begins With Name Code Property Relationship Source ALL Advanced Search NCIm Version: 201706 Version 2.8 (using LexEVS 6.5) Home | NCIt Hierarchy | Sources | Help Suggest changes to this concept Tanibirumab (CUI C3490677) Add to Cart Table of Contents Terms & Properties Synonym Details Relationships By Source Terms & Properties Concept Unique Identifier (CUI): C3490677 NCI Thesaurus Code: C102877 (see NCI Thesaurus info) Semantic Type: Immunologic Factor Semantic Type: Amino Acid, Peptide, or Protein Semantic Type: Pharmacologic Substance NCIt Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor tyrosine kinase expressed by endothelial cells, while VEGF is overexpressed in many tumors and is correlated to tumor progression. PDQ Definition: A fully human monoclonal antibody targeting the vascular endothelial growth factor receptor 2 (VEGFR2), with potential antiangiogenic activity. Upon administration, tanibirumab specifically binds to VEGFR2, thereby preventing the binding of its ligand VEGF. This may result in the inhibition of tumor angiogenesis and a decrease in tumor nutrient supply. VEGFR2 is a pro-angiogenic growth factor receptor -

Synthesis and Cytotoxicity Evaluation of Small
Synthesis and Cytotoxicity evaluation of small 1,4 - triazolic derivatives against B16 melanoma cell lines and a methodolgy study on the synthesis of propargyl ethers from their corresponding propargyl esters without catalyst and under microwave irradiations Shiva Kalhor Monfared To cite this version: Shiva Kalhor Monfared. Synthesis and Cytotoxicity evaluation of small 1,4 - triazolic derivatives against B16 melanoma cell lines and a methodolgy study on the synthesis of propargyl ethers from their corresponding propargyl esters without catalyst and under microwave irradiations. Organic chemistry. Université Pierre et Marie Curie - Paris VI, 2014. English. NNT : 2014PA066235. tel- 01133657 HAL Id: tel-01133657 https://tel.archives-ouvertes.fr/tel-01133657 Submitted on 20 Mar 2015 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THESE DE DOCTORAT DE L’UNIVERSITE PIERRE ET MARIE CURIE Spécialité Chimie Organique Ecole doctorale de Chimie Moléculaire Paris Centre Présentée par Mme Shiva Kalhor-Monfared Pour obtenir le grade de DOCTEUR de l’UNIVERSITÉ PIERRE ET MARIE CURIE Sujet de la thèse : Synthesis and Cytotoxicity evaluation of small 1,4-triazolic derivatives against B16 melanoma cell lines and a methodolgy study on the synthesis of propargyl ethers from their corresponding propargyl esters without catalyst and under microwave irradiations soutenue le 18 septembre 2014 devant le jury composé de : Mr F. -

WO 2011/089216 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date t 28 July 2011 (28.07.2011) WO 2011/089216 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 47/48 (2006.01) C07K 1/13 (2006.01) kind of national protection available): AE, AG, AL, AM, C07K 1/1 07 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) Number: International Application DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/EP201 1/050821 HN, HR, HU, ID, J , IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 2 1 January 201 1 (21 .01 .201 1) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, (26) Publication Language: English TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 1015 1465. 1 22 January 2010 (22.01 .2010) EP kind of regional protection available): ARIPO (BW, GH, GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, (71) Applicant (for all designated States except US): AS- ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, CENDIS PHARMA AS [DK/DK]; Tuborg Boulevard TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, 12, DK-2900 Hellerup (DK). -

The Role of Calcium and Mitochondria in the Etiology and Treatment of Three Different Disease Paradigms
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Sciences The Role of Calcium and Mitochondria in the Etiology and Treatment of Three Different Disease Paradigms Submitted by: Christine Brink In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Sciences Examination Committee Major Advisor: David Giovannucci, Ph.D. Academic Linda Dokas, Ph.D. Advisory Committee: Joseph Margiotta, Ph.D. Andrew Beavis, Ph.D. Ana Marie Oyarce, Ph.D. L. John Greenfield, M.D., Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: December 7, 2007 The Role of Calcium and Mitochondria in the Etiology and Treatment of Three Different Disease Paradigms Christine A. Brink University of Toledo, Health Science Campus 2007 Acknowledgements First, I would like to thank my advisor, Dr. David Giovannucci, for his encouragement and support throughout my graduate training. His advice and understanding have been essential to my success over the past 5 years. I will always be grateful for the education he has provided to me, and the compassion he has shown toward me. Next, I would like to thank Jenny Giovannucci for her illustrations and encouragement. I would also like to thank Rebecca Pierson for providing the primary cortical neuronal cultures, and countless words of advice. Additionally, I would like to thank Christian Peters for his counsel and assistance throughout our training. In addition, I would like to thank my committee members, Dr. Greenfield, Dr. Dokas, Dr. Margiotta, Dr. Beavis, and Dr. Oyarce, for their contributions and guidance. -

Ca Signalling in Endothelial Progenitor Cells
Send Orders for Reprints to [email protected] Current Vascular Pharmacology, 2014, 12, 87-105 87 Ca2+ Signalling in Endothelial Progenitor Cells: A Novel Means to Improve Cell-Based Therapy and Impair Tumour Vascularisation Francesco Moccia1,*, Francesco Lodola1, Silvia Dragoni1, Elisa Bonetti2, Cinzia Bottino3, Germano Guerra4, Umberto Laforenza3, Vittorio Rosti2 and Franco Tanzi1 1Department of Biology and Biotechnology “Lazzaro Spallanzani”, Laboratory of Physiology, University of Pavia, via Forlanini 6, 27100 Pavia, Italy; 2Unit of Clinical Epidemiology, Fondazione IRCCS Policlinico San Matteo, 27100 Pavia, Italy; 3Department of Molecular Medicine, University of Pavia, via Forlanini 6, 27100 Pavia, Italy; 4Department of Health Sciences, University of Molise, Via F. De Santis, 86100 Campobasso, Italy Abstract: Endothelial progenitor cells (EPCs) have recently been employed in cell-based therapy (CBT) to promote re- generation of ischemic organs, such as heart and limbs. Furthermore, EPCs may sustain tumour vascularisation and pro- vide an additional target for anticancer therapies. CBT is limited by the paucity of cells harvested from peripheral blood and suffers from several pitfalls, including the low rate of engrafted EPCs, whereas classic antiangiogenic treatments manifest a number of side effects and may induce resistance into the patients. CBT will benefit of a better understanding of the signal transduction pathway(s) which drive(s) EPC proliferation, trafficking, and incorporation into injured tissues. At the same time, this information might outline alternative molecular targets to impair tumor neovascularisation and im- prove the therapeutic outcome of antiangiogenic strategies. An increase in intracellular Ca2+ concentration is the key sig- nal in the regulation of cellular replication, migration, and differentiation. -

(12) Patent Application Publication (10) Pub. No.: US 2008/0081074 A1 Gu Et Al
US 20080081074A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0081074 A1 Gu et al. (43) Pub. Date: Apr. 3, 2008 (54) POLYMERS FOR FUNCTIONAL PARTICLES (52) U.S. Cl. .......................... 424/489: 424/94.1; 506/23; 5147772.4 (75) Inventors: Frank X. Gu, Cambridge, MA (US); Benjamin A. Teply, Omaha, NE (US); Robert S. Langer, Newton, MA (US); (57) ABSTRACT Omid C. Farokhzad, Chestnut Hill, MA (US) The present invention generally relates to polymers and macromolecules, in particular, to block polymers useful in Correspondence Address: particles Such as nanoparticles. One aspect of the invention WOLF GREENFIELD & SACKS, P.C. is directed to a method of developing nanoparticles with 6OO ATLANTIC AVENUE desired properties. In one set of embodiments, the method BOSTON, MA 02210-2206 (US) includes producing libraries of nanoparticles having highly controlled properties, which can be formed by mixing (73) Assignees: Massachusetts Institute of Technology, together two or more macromolecules in different ratios. Cambridge, MA: The Brigham & Wom One or more of the macromolecules may be a polymeric en's Hospital, Inc., Boston, MA conjugate of a moiety to a biocompatible polymer. In some cases, the nanoparticle may contain a drug. The moiety, in (21) Appl. No.: 11/803,843 Some embodiments, may have a molecular weight greater than about 1000 Da; for example, the moiety may include a (22) Filed: May 15, 2007 polypeptide or a polynucleotide. Such as an aptamer. The moiety may also be a targeting moiety, an imaging moiety, Related U.S. Application Data a chelating moiety, a charged moiety, or a therapeutic (60) Provisional application No. -

Calcium Channel Ca2+ Channels;Ca Channels
Calcium Channel Ca2+ channels;Ca channels Calcium channel is an ion channel which displays selective permeability to calcium ions. It is sometimes synonymous as voltage-dependent calcium channel, although there are also ligand-gated calcium channels. Voltage-gated calcium (CaV) channels catalyse rapid, highly selective influx of Ca 2+ into cells despite a 70-fold higher extracellular concentration of Na +. Some calcium channel blockers have the added benefit of slowing your heart rate, which can further reduce blood pressure, relieve chest pain (angina) and control an irregular heartbeat. www.MedChemExpress.com 1 Calcium Channel Inhibitors & Modulators (+)-Kavain ABT-639 Cat. No.: HY-B1671 Cat. No.: HY-19721 Bioactivity: (+)-Kavain, a main kavalactone extracted from Piper Bioactivity: ABT-639 is a novel, peripherally acting, selective T-type methysticum, has anticonvulsive properties, attenuating Ca2+ channel blocker. vascular smooth muscle contraction through interactions with voltage-dependent Na + and Ca 2+ channels [1]. (+)-Kav… Purity: 99.98% Purity: 99.15% Clinical Data: No Development Reported Clinical Data: Phase 2 Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 5 mg, 10 mg 1 mg, 5 mg, 10 mg, 50 mg, 100 mg ABT-639 hydrochloride Acetylcholine chloride Cat. No.: HY-101616 (Ach; ACh chloride) Cat. No.: HY-B0282 Bioactivity: ABT-639 hydrochloride is a novel, peripherally acting, Bioactivity: Acetylcholine (chloride) is a common neurotransmitter found selective T-type Ca2+ channel blocker. in the central and peripheral nerve system. Purity: >98% Purity: 98.0% Clinical Data: No Development Reported Clinical Data: Launched Size: 1 mg, 5 mg, 10 mg, 20 mg Size: 10mM x 1mL in DMSO, 1 g, 5 g ACT-709478 AE0047 Hydrochloride Cat. -
Calcium Channel Ca2+ Channels; Ca Channels
Calcium Channel Ca2+ channels; Ca channels Calcium channel is an ion channel which displays selective permeability to calcium ions. It is sometimes synonymous as voltage-dependent calcium channel, although there are also ligand-gated calcium channels. Voltage-gated calcium (CaV) channels catalyse rapid, highly selective influx of Ca2+ into cells despite a 70-fold higher extracellular concentration of Na+. Some calcium channel blockers have the added benefit of slowing your heart rate, which can further reduce blood pressure, relieve chest pain (angina) and control an irregular heartbeat. www.MedChemExpress.com 1 Calcium Channel Inhibitors, Antagonists, Activators, Agonists & Modulators (+)-Kavain (2R/S)-6-PNG Cat. No.: HY-B1671 (6-Prenylnaringenin) Cat. No.: HY-115681 (+)-Kavain, a main kavalactone extracted from Piper (2R/S)-6-PNG (6-Prenylnaringenin) is a Cav3.2 2+ methysticum, has anticonvulsive properties, (T-type) Ca channel blocker (IC50=991 nM). attenuating vascular smooth muscle contraction (2R/S)-6-PNG suppresses neuropathic allodynia in through interactions with voltage-dependent Na+ mouse pain models. and Ca2+ channels. Purity: 99.98% Purity: ≥99.0% Clinical Data: Launched Clinical Data: Phase 1 Size: 10 mM × 1 mL, 5 mg, 10 mg Size: 5 mg (R)-(+)-Bay-K-8644 (R)-Lercanidipine D3 hydrochloride Cat. No.: HY-15125 Cat. No.: HY-B0612DS (R)-(+)-Bay-K-8644 is a calcium channel (R)-lercanidipine D3 (hydrochloride) is a inhibitor. (R)-(+)-Bay-K-8644 inhibits Ba2+ deuterium labeled (R)-Lercanidipine hydrochloride. currents (IBa) (IC50=975 nM). (R)-Lercanidipine D3 (hydrochloride), the R-enantiomer of Lercanidipine, is a calcium channel blocker. Purity: 99.69% Purity: >98% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 10 mM × 1 mL, 5 mg, 10 mg, 25 mg, 50 mg, 100 mg Size: 1 mg, 5 mg (R)-Lercanidipine hydrochloride (Rac)-MEM 1003 Cat. -

Store-Dependent Ca Entry in Endothelial Progenitor Cells As A
Send Orders of Reprints at [email protected] 5802 Current Medicinal Chemistry, 2012, 19, 5802-5818 Store-Dependent Ca2+ Entry in Endothelial Progenitor Cells As a Perspective Tool to Enhance Cell-Based Therapy and Adverse Tumour Vascularization F. Mocciaa, S. Dragonia, F. Lodolaa, E. Bonettib, C. Bottinoa, G. Guerrac, U. Laforenzaa, V. Rostib and F. Tanzia aDepartment of Physiology, University of Pavia, via Forlanini 6, 27100 Pavia, Italy; bUnit of Clinical Epidemiology, Fondazione IRCCS Policlinico San Matteo, 27100 Pavia, Italy; cDepartment of Health Sciences, University of Molise, Via F. De Santis, 86100 Campobasso, Italy Abstract: Endothelial progenitor cells (EPCs) have recently been employed in cell-based therapy (CBT) to promote neovascularization and regeneration of ischemic organs, such as heart and limbs. Furthermore, EPCs may be recruited from bone marrow by growing tumors to drive the angiogenic switch through physical engrafting into the lumen of nascent vessels or paracrine release of pro-angiogenic fac- tors. CBT is hampered by the paucity of EPCs harvested from peripheral blood and suffered from several pitfalls, including the differen- tiation outcome of transplanted cells and low percentage of engrafted cells. Therefore, CBT will benefit from a better understanding of the signal transduction pathway(s) which govern(s) EPC homing, proliferation and incorporation into injured tissues. At the same time, this information might outline alternative molecular targets to combat tumoral neovascularization. We have recently found that store- operated Ca2+ entry, a Ca2+-permeable membrane pathway that is activated upon depletion of the inositol-1,4,5-trisphosphate-sensitive Ca2+ pool, is recruited by vascular endothelial growth factor to support proliferation and tubulogenesis in human circulating endothelial colony forming cells (ECFCs).