Focus On: Gingival Hyperplasia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -

Epidemiology and Indices of Gingival and Periodontal Disease Dr
PEDIATRIC DENTISTRY/Copyright ° 1981 by The American Academy of Pedodontics Vol. 3, Special Issue Epidemiology and indices of gingival and periodontal disease Dr. Poulsen Sven Poulsen, Dr Odont Abstract Validity of an index indicates to what extent the This paper reviews some of the commonly used indices index measures what it is intended to measure. Deter- for measurement of gingivitis and periodontal disease. mination of validity is dependent on the availability Periodontal disease should be measured using loss of of a so-called validating criterion. attachment, not pocket depth. The reliability of several of Pocket depth may not reflect loss of periodontal the indices has been tested. Calibration and training of attachment as a sign of periodontal disease. This is be- examiners seems to be an absolute requirement for a cause gingival swelling will increase the distance from satisfactory inter-examiner reliability. Gingival and periodontal disease is much more severe in several the gingival margin to the bottom of the clinical populations in the Far East than in Europe and North pocket (pseudo-pockets). Thus, depth of the periodon- America, and gingivitis seems to increase with age resulting tal pocket may not be a valid measurement for perio- in loss of periodontal attachment in approximately 40% of dontal disease. 15-year-old children. Apart from the validity and reliability of an index, important factors such as the purpose of the study, Introduction the level of disease in the population, the conditions under which the examinations are going to be per- Epidemiological data form the basis for planning formed etc., will have to enter into choice of an index. -
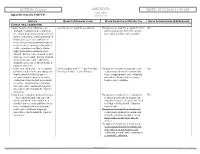
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Essential Dental (Pdf)
Dental Essential Plans 2 Plans1 for Individuals & Families with Optional Vision Benefits2 Table of Contents Optional Vision Benefits 5 Why Dental Essential? 2 Exclusions & Limitations 6 Dental Essential & Notice of Privacy Practices 10 Dental Essential Preferred 3 Wisconsin Outline of Coverage 14 Hearing Discounts 4 California Notices 18 Golden Rule Insurance Company is the underwriter of these plans. This product is administered by Dental Benefit Providers, Inc. Policy Forms GRI-DEN3-JR, -01 (AL), -02 (AZ), -03 (AR), -04 (CA), -05 (CO), -06 (CT), (DE), -08 (DC), -09 (FL), -10 (GA), -51 (HI), -12 (IL), -13 (IN), -14 (IA), -15 (KS), -16 (KY), -17 (LA), -19 (MD), -21 (MI), -22 (MN), -23 (MS), -24 (MO), -26 (NE), -28 (NH), -30 (NM), -32 (NC), -33 (ND), -35 (OK), -36 (OR), -37 (PA), -38 (RI), -39 (SC), -40 (SD), -41 (TN), -42 (TX), -43 (UT), -44 (VT), -45 (VA), -47 (WV), and -48 (WI); GRI-DEN3-JR-PB, -11 (ID), -34 (OH), -46 (WA); GRI-DEN3-JR-PBM, -11 (ID), -34 (OH), -46 (WA) 1 Essential Preferred is the only plan available in CO and MN. 2 The optional vision benefit is not available in MN, RI or WA. The ratio of incurred claims to earned premiums (loss-ratio) for total accident and health for Golden Rule Insurance Company in all states in 2019 was 62.4%. This is an outline only and is not intended to serve as a legal interpretation of benefits. Reasonable effort has been made to have this outline represent the intent of contract language. However, the contract language stands alone and the complete terms of the coverage will be determined by the policy. -

Gingival Recession – Etiology and Treatment
Preventive_V2N2_AUG11:Preventive 8/17/2011 12:54 PM Page 6 Gingival Recession – Etiology and Treatment Mark Nicolucci, D.D.S., M.S., cert. perio implant, F.R.C.D.(C) Murray Arlin, D.D.S., dip perio, F.R.C.D.(C) his article focuses on the recognition and reason is often a prophylactic one; that is we understanding of recession defects of the want to prevent the recession from getting T oral mucosa. Specifically, which cases are worse. This reasoning is also true for the esthetic treatable, how we treat these cases and why we and sensitivity scenarios as well. Severe chose certain treatments. Good evidence has recession is not only more difficult to treat, but suggested that the amount of height of keratinized can also be associated with food impaction, or attached gingiva is independent of the poor esthetics, gingival irritation, root sensitivity, progression of recession (Miyasato et al. 1977, difficult hygiene, increased root caries, loss of Dorfman et al. 1980, 1982, Kennedy et al. 1985, supporting bone and even tooth loss . To avoid Freedman et al. 1999, Wennstrom and Lindhe these complications we would want to treat even 1983). Such a discussion is an important the asymptomatic instances of recession if we consideration with recession defects but this article anticipate them to progress. However, non- will focus simply on a loss of marginal gingiva. progressing recession with no signs or Recession is not simply a loss of gingival symptoms does not need treatment. In order to tissue; it is a loss of clinical attachment and by know which cases need treatment, we need to necessity the supporting bone of the tooth that distinguish between non-progressing and was underneath the gingiva. -

Intrusion of Incisors to Facilitate Restoration: the Impact on the Periodontium
Note: This is a sample Eoster. Your EPoster does not need to use the same format style. For example your title slide does not need to have the title of your EPoster in a box surrounded with a pink border. Intrusion of Incisors to Facilitate Restoration: The Impact on the Periodontium Names of Investigators Date Background and Purpose This 60 year old male had severe attrition of his maxillary and mandibular incisors due to a protrusive bruxing habit. The patient’s restorative dentist could not restore the mandibular incisors without significant crown lengthening. However, with orthodontic intrusion of the incisors, the restorative dentist was able to restore these teeth without further incisal edge reduction, crown lengthening, or endodontic treatment. When teeth are intruded in adults, what is the impact on the periodontium? The purpose of this study was to determine the effect of adult incisor intrusion on the alveolar bone level and on root length. Materials and Methods We collected the orthodontic records of 43 consecutively treated adult patients (aged > 19 years) from four orthodontic practices. This project was approved by the IRB at our university. Records were selected based upon the following criteria: • incisor intrusion attempted to create interocclusal space for restorative treatment or correction of excessive anterior overbite • pre- and posttreatment periapical and cephalometric radiographs were available • no incisor extraction or restorative procedures affecting the cementoenamel junction during the treatment period pretreatment pretreatment Materials and Methods We used cephalometric and periapical radiographs to measure incisor intrusion. The radiographs were imported and the digital images were analyzed with Image J, a public-domain Java image processing program developed at the US National Institutes of Health. -

Hereditary Gingival Fibromatosis CASE REPORT
Richa et al.: Management of Hereditary Gingival Fibromatosis CASE REPORT Hereditary Gingival Fibromatosis and its management: A Rare Case of Homozygous Twins Richa1, Neeraj Kumar2, Krishan Gauba3, Debojyoti Chatterjee4 1-Tutor, Unit of Pedodontics and preventive dentistry, ESIC Dental College and Hospital, Rohini, Delhi. 2-Senior Resident, Unit of Pedodontics and preventive dentistry, Oral Health Sciences Centre, Post Correspondence to: Graduate Institute of Medical Education and Research , Chandigarh, India. 3-Professor and Head, Dr. Richa, Tutor, Unit of Pedodontics and Department of Oral Health Sciences Centre, Post Graduate Institute of Medical Education and preventive dentistry, ESIC Dental College and Research, Chandigarh, India. 4-Senior Resident, Department of Histopathology, Oral Health Sciences Hospital, Rohini, Delhi Centre, Post Graduate Institute of Medical Education and Research, Chandigarh, India. Contact Us: www.ijohmr.com ABSTRACT Hereditary gingival fibromatosis (HGF) is a rare condition which manifests itself by gingival overgrowth covering teeth to variable degree i.e. either isolated or as part of a syndrome. This paper presented two cases of generalized and severe HGF in siblings without any systemic illness. HGF was confirmed based on family history, clinical and histological examination. Management of both the cases was done conservatively. Quadrant wise gingivectomy using ledge and wedge method was adopted and followed for 12 months. The surgical procedure yielded functionally and esthetically satisfying results with no recurrence. KEYWORDS: Gingival enlargement, Hereditary, homozygous, Gingivectomy AA swollen gums. The patient gave a history of swelling of upper gums that started 2 years back which gradually aaaasasasss INTRODUCTION increased in size. The child’s mother denied prenatal Hereditary Gingival Enlargement, being a rare entity, is exposure to tobacco, alcohol, and drug. -

Vhi Dental Rules - Terms and Conditions
Vhi Dental Rules - Terms and Conditions Date of Issue: 1st January 2021 Introduction to Your Policy The purpose of this Policy is to provide an Insured Person with Dental Services as described below. Only the stated Treatments are covered. Maximum benefit limits and any applicable waiting periods are listed in Your Table of Benefits. In order to qualify for cover under this Policy all Treatments must be undertaken by a Dentist or a Dental Hygienist in a dental surgery, be clinically necessary, in line with usual, reasonable and customary charges for the area where the Treatment was undertaken, and must be received by the Insured Person during their Period of Cover. Definitions We have defined below words or phrases used throughout this Policy. To avoid repeating these definitions please note that where these words or phrases appear they have the precise meaning described below unless otherwise stated. Where words or phrases are not listed within this section, they will take on their usual meaning within the English language. Accident An unforeseen injury caused by direct impact outside of oral cavity to an Insured Person’s teeth and gums (this includes damage to dentures whilst being worn). Cancer A malignant tumour, tissues or cells, characterised by the uncontrolled growth and spread of malignant cells and invasion of tissue. Child/Children Your children, step-child/children, legally adopted child/children or child/children where you are their legal guardian provided that the child/children is under age 18 on the date they are first included under this Policy. Claims Administrator Vhi Dental Claims Department, Intana, IDA Business Park, Athlumney, Navan, Co. -

Gingivectomy Approaches: a Review
ISSN: 2469-5734 Peres et al. Int J Oral Dent Health 2019, 5:099 DOI: 10.23937/2469-5734/1510099 Volume 5 | Issue 3 International Journal of Open Access Oral and Dental Health REVIEW ARTICLE Gingivectomy Approaches: A Review Millena Mathias Peres1, Tais da Silva Lima¹, Idiberto José Zotarelli Filho1,2*, Igor Mariotto Beneti1,2, Marcelo Augusto Rudnik Gomes1,2 and Patrícia Garani Fernandes1,2 1University Center North Paulista (Unorp) Dental School, Brazil 2Department of Scientific Production, Post Graduate and Continuing Education (Unipos), Brazil Check for *Corresponding author: Prof. Idiberto José Zotarelli Filho, Department of Scientific Production, Post updates Graduate and Continuing Education (Unipos), Street Ipiranga, 3460, São José do Rio Preto SP, 15020-040, Brazil, Tel: +55-(17)-98166-6537 gingival tissue, and can be corrected with surgical tech- Abstract niques such as gingivectomy. Many patients seek dental offices for a beautiful, harmoni- ous smile to boost their self-esteem. At present, there is a Gingivectomy is a technique that is easy to carry great search for oral aesthetics, where the harmony of the out and is usually well accepted by patients, who, ac- smile is determined not only by the shape, position, and col- cording to the correct indications, can obtain satisfac- or of teeth but also by the gingival tissue. The present study aimed to establish the etiology and diagnosis of the gingi- tory results in dentogingival aesthetics and harmony val smile, with the alternative of correcting it with very safe [3]. surgical techniques such as gingivectomy. The procedure consists in the elimination of gingival deformities resulting The procedure consists in the removal of gingival de- in a better gingival contour. -

Classifications for Gingival Recession: a Mini Review
Galore International Journal of Health Sciences and Research Vol.3; Issue: 1; Jan.-March 2018 Website: www.gijhsr.com Review Article P-ISSN: 2456-9321 Classifications for Gingival Recession: A Mini Review Dr Amit Mani1, Dr. Rosiline James2 1Professor and HOD, Dept. of Periodontics, 2Post graduate student, Pravara Institute of Medical Sciences, Loni, India Corresponding Author: Rosiline James _____________________________________________________________________________________________________ ABSTRACT the treatment. The following are the classifications for gingival recession. Gingival Recession is a common problem 1. Sullivan and Atkins (1968) associated with or without Periodontitis. It can The basis for the classification was depth be associated with many etiological factors. The and width of the defect. one of the common factor is faulty tooth The four categories were: brushing trauma. There are other factors too which contribute to the gingival recession. Not Deep wide only Gingival Recession causes an esthetic Shallow wide problem but also causes hypersensitivity and Deep narrow associated caries. This paper reviews the various Shallow narrow. classifications for gingival recession which can This classification though simple is be useful for the proper diagnosis and treatment. subjected to open interpretation of the examiner and inter examiner variability and Keywords: Gingival Recession, Classification is therefore not reproducible. [3] for Gingival Recession, Palatal recession INTRODUCTION Gingival recession is defined as an apical shift of the gingival margin (GM) from its position 1 mm coronal to or at the level of the cemento-enamel junction (CEJ) with exposure of the root surface to the oral environment. [1] The displacement of marginal tissue apical to the cemento- enamel junction (CEJ). [2] The term “marginal tissue recession” has been considered to be more accurate than “gingival recession,” since the marginal Figure 1: Sullivan & Atkins Classification tissue may have been what is known as alveolar mucosa. -

External Root Resorption of Young Premolar Teeth in Dentition With
10.5005/jp-journals-10015-1236 KapilaORIGINAL Arambawatta RESEARCH et al External Root Resorption of Young Premolar Teeth in Dentition with Crowding Kapila Arambawatta, Roshan Peiris, Dhammika Ihalagedara, Anushka Abeysundara, Deepthi Nanayakkara ABSTRACT least understood type of root resorption, characterized by its The present study was conducted to investigate the prevalence FHUYLFDOORFDWLRQDQGLQYDVLYHQDWXUH7KLVUHVRUSWLYHSURFHVV of external cervical resorption (ECR) in different tooth surfaces which leads to prRJUHVVLYHDQGXVXDOO\GHVWUXFWLYHORVVRI RIPD[LOODU\¿UVWSUHPRODUVLQD6UL/DQNDQSRSXODWLRQ tooth structure has been a source of interest to clinicians A sample of 59 (15 males, 44 females) permanent maxillary 2-5 ¿UVWSUHPRODUV DJHUDQJH\HDUV ZHUHXVHG7KHWHHWK DQGUHVHDUFKHUVIRURYHUDFHQWXU\ 7KHH[DFWFDXVHRI had been extracted for orthodontic reasons and were stored (&5LVSRRUO\XQGHUVWRRG$OWKRXJKWKHHWLRORJ\DQG LQIRUPDOLQ0RUSKRORJLFDOO\VRXQGWHHWKZHUHVHOHFWHG SDWKRJHQHVLVUHPDLQREVFXUHVHYHUDOSRWHQWLDOSUHGLVSRVLQJ IRUWKHVWXG\7KHWHHWKZHUHVWDLQHGZLWKFDUEROIXFKVLQ7KH IDFWRUVKDYHEHHQSXWIRUZDUGDQGRIWKHVHWKHLQWUDFRURQDO cervical regions of the stained teeth were observed under 10× 6 PDJQL¿FDWLRQV XVLQJ D GLVVHFWLQJ PLFURVFRSH 2O\PSXV 6= bleaching has been the most widely documented factor. In WRLGHQWLI\DQ\UHVRUSWLRQDUHDV7KHUHVRUSWLRQDUHDVSUHVHQW addition, dental trauma, orthodontic treatment, periodontal on buccal, lingual, mesial and distal aspects of all teeth were WUHDWPHQWVXUJHU\LQYROYLQJWKHFHPHQWRHQDPHOMXQFWLRQ UHFRUGHG DQGLGLRSDWKLFHWLRORJ\KDYHDOVREHHQGHVFULEHG2,7-11