Benign Inclusions in Lymph Nodes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Axillary Lymph Nodes in Breast Cancer Patients: Sonographic Evaluation*
Pinheiro DJPCArtigo et al. / deLinfonodos Revisão axilares – avaliação ultrassonográfica Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica* Axillary lymph nodes in breast cancer patients: sonographic evaluation Denise Joffily Pereira da Costa Pinheiro1, Simone Elias2, Afonso Celso Pinto Nazário3 Pinheiro DJPC, Elias S, Nazário ACP. Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica. Radiol Bras. 2014 Jul/Ago; 47(4):240–244. Resumo O estadiamento axilar nas pacientes portadoras de câncer de mama inicial é fator essencial no planejamento terapêutico. Atualmente este é realizado durante o tratamento cirúrgico, mas há uma tendência em buscar técnicas pré-operatórias e de menor morbidade para avaliação dos linfonodos axilares. A ultrassonografia é um exame amplamente usado para esta finalidade e muitas vezes associado a punção aspirativa por agulha fina ou por agulha grossa. Entretanto, os critérios ultrassonográficos de suspeição para linfonodos axilares não apresentam valores preditivos significativos, gerando resultados discrepantes em estudos sobre sensibilidade e especificidade do método. O objetivo deste trabalho é realizar uma revisão na literatura médica sobre a ultrassonografia no estadiamento axilar e as principais alterações morfológicas do linfonodo metastático. Unitermos: Câncer de mama; Linfonodos axilares; Ultrassonografia; Aspectos morfológicos. Abstract Axillary staging of patients with early-stage breast cancer is essential in the treatment planning. Currently such staging is intraoperatively performed, but there is a tendency to seek a preoperative and less invasive technique to detect lymph node metastasis. Ultrasonography is widely utilized for this purpose, many times in association with fine-needle aspiration biopsy or core needle biopsy. However, the sonographic criteria for determining malignancy in axillary lymph nodes do not present significant predictive values, producing discrepant results in studies evaluating the sensitivity and specificity of this method. -
Impact of the Number of Dissected Axillary Lymph Nodes on Survival
ISSN: 2643-4563 Nabil et al. Int J Oncol Res 2019, 2:015 DOI: 10.23937/2643-4563/1710015 Volume 2 | Issue 1 International Journal of Open Access Oncology Research RESEARCH ARTICLE Impact of the Number of Dissected Axillary Lymph Nodes on Survival in Breast Cancer Patients Emad Eldin Nabil1, Ahmed M Maklad2,3, Ashraf Elyamany4,5*, Emad Gomaa6 and Moamen M Ali3,7 1Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 2Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 3King Fahad Medical City, Riyadh, KSA 4 Medical Oncology Department, SECI, Assiut University, Egypt Check for updates 5King Saud Medical City, Riyadh, KSA 6General Surgery Department, Sohag University Hospitals, Egypt 7Medical Physics, Radiation Oncology Department, SECI, Assiut University, Egypt *Corresponding author: Ashraf Elyamany, Medical Oncology Department, SECI, Assiut University, Egypt; King Saud Medical City, Riyadh, KSA Abstract regard median OS for patients having more than 10 LN excised was for N0, N1, N2, N3 5.57, 5.94, 4.97, 4.61 years Background: For patients with breast cancer, axillary dis- respectively while in the other group having less than 10 LN section was a standard treatment, especially with patient excised OS was 5.4, 5.14, 5.14 years respectively with P = with positive metastases in the sentinel nodes. For some 0.117. Regarding Lymphedema There was highly significant patients axillary dissection might be over-treatment, includ- difference between both arms p value 0.000, with higher ing those who have had a mastectomy. Especially with grades in arm I (moderate 17 cases and 6 cases severe the new trend of many radiation-therapy centers, provide edema). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -

Epithelial Tissue
Epithelial Tissue Epithelial Tissue Tissues - Introduction · a group of similar cells specialized to carry on a particular function · tissue = cells + extracellular matrix nonliving portion of a tissue that supports cells · 4 types epithelial - protection, secretion, absorption connective - support soft body parts and bind structures together muscle - movement nervous - conducts impulses used to help control and coordinate body activities Epithelial Tissues Characteristics Epithelial Classifications · free surface open to the outside or an open · classified based on shape and # of cell layers internal space (apical surface) · shape · basement membrane anchors epithelium to squamous - thin, flat cells underlying connective tissue cuboidal - cube-shaped cells columnar - tall, elongated cells · lack blood vessels · number · readily divide (ex. skin healing) simple - single layer · tightly packed with little extracellular space stratified - 2 or more layers Epithelial Locations Simple Squamous Epithelium · a single layer of thin, flattened cells · cover body surfaces, cover and line internal organs, and compose glands looks like a fried egg · easily damaged skin cells, cells that line the stomach and small intestine, inside your mouth · common at sites of filtration, diffusion, osmosis; cover surfaces · air sacs of the lungs, walls of capillaries, linings cheek cells of blood and lymph vessels intestines skin Epithelial Tissue Simple Cuboidal Epithelium Simple Columnar Epithelium · single layer of cube-shaped cells · single layer of cells -

Lymphatic Drainage of the Breast: from Theory to Surgical Practice
Int. J. Morphol., 27(3):873-878, 2009. Lymphatic Drainage of the Breast: from Theory to Surgical Practice Drenaje Linfático de la Mama: desde la Teoría a la Práctica Quirúrgica *José Humberto Tavares Guerreiro Fregnani & **José Rafael Macéa FREGNANI, J. H. T. G. & MACÉA, J. R. Lymphatic drainage of the breast: from theory to surgical practice. Int. J. Morphol., 27(3):873-878, 2009. SUMMARY: Until recently, complete removal of axillary lymph nodes was performed as part of the treatment of breast cancer. Sentinel lymph node biopsy (SLNB) in selected cases has reduced the number of cases of wide axillary dissection and the related morbidity. Knowledge of breast lymphatic drainage is essential for understanding the principles behind SLNB and also for performing safe and correct axillary lymphonodectomy. This paper describes in detail the anatomical issues relating to breast lymphatic drainage and the correlated axillary and extra-axillary lymph nodes. In addition, it shows the application of this theoretical knowledge to surgical practice, especially with regard to SLNB and lymphonodectomy. The surgical nomenclature is compared with the current International Anatomical Terminology. KEY WORDS: Lymphatic drainage, Sentinel lymph node biopsy, Breast cancer. INTRODUCTION Breast cancer is the most frequent type of tumor changes to the sensitivity of the upper limb, posterior scapular among women, accounting for approximately one quarter dislocation (winged scapula syndrome), brachial plexus of all tumors in women. It has been estimated that more than lesions, axillary vessel thrombosis and lesions, skin necrosis one million new cases occur worldwide annually. Breast and pectoral muscle atrophy, among others (Torresan et al., cancer is responsible for significant morbidity and mortality 2002; Kim et al., 2006). -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Anatomy and Physiology in Relation to Compression of the Upper Limb and Thorax
Clinical REVIEW anatomy and physiology in relation to compression of the upper limb and thorax Colin Carati, Bren Gannon, Neil Piller An understanding of arterial, venous and lymphatic flow in the upper body in normal limbs and those at risk of, or with lymphoedema will greatly improve patient outcomes. However, there is much we do not know in this area, including the effects of compression upon lymphatic flow and drainage. Imaging and measuring capabilities are improving in this respect, but are often expensive and time-consuming. This, coupled with the unknown effects of individual, diurnal and seasonal variances on compression efficacy, means that future research should focus upon ways to monitor the pressure delivered by a garment, and its effects upon the fluids we are trying to control. More is known about the possible This paper will describe the vascular Key words effects of compression on the anatomy of the upper limb and axilla, pathophysiology of lymphoedema when and will outline current understanding of Anatomy used on the lower limbs (Partsch and normal and abnormal lymph drainage. It Physiology Junger, 2006). While some of these will also explain the mechanism of action Lymphatics principles can be applied to guide the use of compression garments and will detail Compression of compression on the upper body, it is the effects of compression on fluid important that the practitioner is movement. knowledgeable about the anatomy and physiology of the upper limb, axilla and Vascular drainage of the upper limb thorax, and of the anatomical and vascular It is helpful to have an understanding of Little evidence exists to support the differences that exist between the upper the vascular drainage of the upper limb, use of compression garments in the and lower limb, so that the effects of these since the lymphatic drainage follows a treatment of lymphoedema, particularly differences can be considered when using similar course (Figure 1). -

Squamous Epithelium in the Human Thyroid Gland
J Clin Pathol: first published as 10.1136/jcp.19.4.384 on 1 July 1966. Downloaded from J. clin. Path. (1966), 19, 384. Squamous epithelium in the human thyroid gland J. N. HARCOURT-WEBSTER1 From the Department ofPathology, University ofEdinburgh SYNOPSIS Four cases are reported in each of which squamous epithelium was an incidental finding in surgically excised thyroid gland tissue. The occasional thyroid cyst lined throughout by squamous cells probably represents a persistent ultimo-branchial body, but the evidence indicates that the usual source of such cells in this gland is metaplasia of the follicular epithelium. An explanation is offered for the infrequency of this transformation in the thyroid, despite the frequent occurrence of the changes which predispose to epithelial metaplasia at other sites. There is no evidence to suggest that squamous cells arising in this gland by either of these means have any sinister significance. Squamous epithelium was first described in a human iodine uptake studies were normal but serological anti- thyroid gland by Nicholson (1922); he attributed body tests were positive (ADT: +ve on second day; this finding to metaplasia of the follicular epithelium TCH: 1/250,000; CFT: 1/250). The provisional diagnosis was Hashimoto's disease; a biopsy was taken from the induced by severe chronic inflammatory and fibrotic right lobe with a wedge resection of the isthmus. changes in the gland. Epithelial metaplasia occurs in Histology Sections of the rock-hard, pale fawn tissue response to altered function or at least as the result show abundant, interwoven, thick bands of hyaline col- of altered environment (Boyd, 1961). -

Mixed Type Adrenal Cyst: a Case Report
Eastern Journal of Medicine 20 (2015) 163-166 Case Report Mixed type adrenal cyst: A case report Gulay Buluta,*, Mehmet Deniz Bulutb, Deniz Yilmaza, Sebahattin Celikc, Nursen Toprakb aDepartment of Pathology, Yuzuncu Yil University Faculty of Medicine, Van, Turkey bDepartment of Radiology, Van Research and Training Hospital, Van, Turkey cDepartment of General Surgery, Van Research and Training Hospital, Van, Turkey Abstract. Adrenal cysts are rare lesions that usually progress asymptomatically. They are often determined post- mortem. Our case was a 50-year old-male who had presented to our clinic with upper right quadrant pain. The computed tomography demonstrated a cystic mass in the adrenal gland. No abnormalities were determined in the laboratory tests. According to the histopathological and immunohistochemical examination, the cyst was evaluated as a mixed-type adrenal cyst, the wall of which was covered with endothelium, mesothelium and cubic epithelium. We believed that the case was worth presenting, since it was the first diagnosed mixed-type adrenal cyst in the literature. Key words: Mixed-type adrenal cyst, endothelial cyst, epithelial cyst, mesothelial cyst pain. There was no history of hypertension or 1. Introduction trauma in the past. Per abdominal examination Adrenal cysts are rarely encountered clinical showed a soft abdomen; no mass was felt. entities. Their incidence has been reported from Haemogram was normal. A complete endocrine 0.06%-0.18% in autopsy series (1). In 1966, workup including the estimation of urinary Foster put forth a classification based on the metanephrines, vanillylmandelic acid and free histopathology of 220 adrenal cysts into parasitic cortisol did not show any hormonal cysts (7%), epithelial cysts (9%), pseudocysts hypersecretion. -
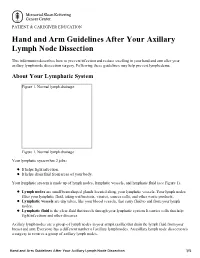
Hand and Arm Guidelines After Your Axillary Lymph Node Dissection
PATIENT & CAREGIVER EDUCATION Hand and Arm Guidelines After Your Axillary Lymph Node Dissection This information describes how to prevent infection and reduce swelling in your hand and arm after your axillary lymph node dissection surgery. Following these guidelines may help prevent lymphedema. About Your Lymphatic System Figure 1. Normal lymph drainage Figure 1. Normal lymph drainage Your lymphatic system has 2 jobs: It helps fight infection. It helps drain fluid from areas of your body. Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1). Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products. Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes. Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases. Axillary lymph nodes are a group of lymph nodes in your armpit (axilla) that drain the lymph fluid from your breast and arm. Everyone has a different number of axillary lymph nodes. An axillary lymph node dissection is a surgery to remove a group of axillary lymph nodes. Hand and Arm Guidelines After Your Axillary Lymph Node Dissection 1/5 About Lymphedema Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema.