Hand/Peripheral Nerve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Axillary Lymph Nodes in Breast Cancer Patients: Sonographic Evaluation*
Pinheiro DJPCArtigo et al. / deLinfonodos Revisão axilares – avaliação ultrassonográfica Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica* Axillary lymph nodes in breast cancer patients: sonographic evaluation Denise Joffily Pereira da Costa Pinheiro1, Simone Elias2, Afonso Celso Pinto Nazário3 Pinheiro DJPC, Elias S, Nazário ACP. Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica. Radiol Bras. 2014 Jul/Ago; 47(4):240–244. Resumo O estadiamento axilar nas pacientes portadoras de câncer de mama inicial é fator essencial no planejamento terapêutico. Atualmente este é realizado durante o tratamento cirúrgico, mas há uma tendência em buscar técnicas pré-operatórias e de menor morbidade para avaliação dos linfonodos axilares. A ultrassonografia é um exame amplamente usado para esta finalidade e muitas vezes associado a punção aspirativa por agulha fina ou por agulha grossa. Entretanto, os critérios ultrassonográficos de suspeição para linfonodos axilares não apresentam valores preditivos significativos, gerando resultados discrepantes em estudos sobre sensibilidade e especificidade do método. O objetivo deste trabalho é realizar uma revisão na literatura médica sobre a ultrassonografia no estadiamento axilar e as principais alterações morfológicas do linfonodo metastático. Unitermos: Câncer de mama; Linfonodos axilares; Ultrassonografia; Aspectos morfológicos. Abstract Axillary staging of patients with early-stage breast cancer is essential in the treatment planning. Currently such staging is intraoperatively performed, but there is a tendency to seek a preoperative and less invasive technique to detect lymph node metastasis. Ultrasonography is widely utilized for this purpose, many times in association with fine-needle aspiration biopsy or core needle biopsy. However, the sonographic criteria for determining malignancy in axillary lymph nodes do not present significant predictive values, producing discrepant results in studies evaluating the sensitivity and specificity of this method. -
Impact of the Number of Dissected Axillary Lymph Nodes on Survival
ISSN: 2643-4563 Nabil et al. Int J Oncol Res 2019, 2:015 DOI: 10.23937/2643-4563/1710015 Volume 2 | Issue 1 International Journal of Open Access Oncology Research RESEARCH ARTICLE Impact of the Number of Dissected Axillary Lymph Nodes on Survival in Breast Cancer Patients Emad Eldin Nabil1, Ahmed M Maklad2,3, Ashraf Elyamany4,5*, Emad Gomaa6 and Moamen M Ali3,7 1Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 2Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 3King Fahad Medical City, Riyadh, KSA 4 Medical Oncology Department, SECI, Assiut University, Egypt Check for updates 5King Saud Medical City, Riyadh, KSA 6General Surgery Department, Sohag University Hospitals, Egypt 7Medical Physics, Radiation Oncology Department, SECI, Assiut University, Egypt *Corresponding author: Ashraf Elyamany, Medical Oncology Department, SECI, Assiut University, Egypt; King Saud Medical City, Riyadh, KSA Abstract regard median OS for patients having more than 10 LN excised was for N0, N1, N2, N3 5.57, 5.94, 4.97, 4.61 years Background: For patients with breast cancer, axillary dis- respectively while in the other group having less than 10 LN section was a standard treatment, especially with patient excised OS was 5.4, 5.14, 5.14 years respectively with P = with positive metastases in the sentinel nodes. For some 0.117. Regarding Lymphedema There was highly significant patients axillary dissection might be over-treatment, includ- difference between both arms p value 0.000, with higher ing those who have had a mastectomy. Especially with grades in arm I (moderate 17 cases and 6 cases severe the new trend of many radiation-therapy centers, provide edema). -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -

Lymphatic Drainage of the Breast: from Theory to Surgical Practice
Int. J. Morphol., 27(3):873-878, 2009. Lymphatic Drainage of the Breast: from Theory to Surgical Practice Drenaje Linfático de la Mama: desde la Teoría a la Práctica Quirúrgica *José Humberto Tavares Guerreiro Fregnani & **José Rafael Macéa FREGNANI, J. H. T. G. & MACÉA, J. R. Lymphatic drainage of the breast: from theory to surgical practice. Int. J. Morphol., 27(3):873-878, 2009. SUMMARY: Until recently, complete removal of axillary lymph nodes was performed as part of the treatment of breast cancer. Sentinel lymph node biopsy (SLNB) in selected cases has reduced the number of cases of wide axillary dissection and the related morbidity. Knowledge of breast lymphatic drainage is essential for understanding the principles behind SLNB and also for performing safe and correct axillary lymphonodectomy. This paper describes in detail the anatomical issues relating to breast lymphatic drainage and the correlated axillary and extra-axillary lymph nodes. In addition, it shows the application of this theoretical knowledge to surgical practice, especially with regard to SLNB and lymphonodectomy. The surgical nomenclature is compared with the current International Anatomical Terminology. KEY WORDS: Lymphatic drainage, Sentinel lymph node biopsy, Breast cancer. INTRODUCTION Breast cancer is the most frequent type of tumor changes to the sensitivity of the upper limb, posterior scapular among women, accounting for approximately one quarter dislocation (winged scapula syndrome), brachial plexus of all tumors in women. It has been estimated that more than lesions, axillary vessel thrombosis and lesions, skin necrosis one million new cases occur worldwide annually. Breast and pectoral muscle atrophy, among others (Torresan et al., cancer is responsible for significant morbidity and mortality 2002; Kim et al., 2006). -

Anatomy and Physiology in Relation to Compression of the Upper Limb and Thorax
Clinical REVIEW anatomy and physiology in relation to compression of the upper limb and thorax Colin Carati, Bren Gannon, Neil Piller An understanding of arterial, venous and lymphatic flow in the upper body in normal limbs and those at risk of, or with lymphoedema will greatly improve patient outcomes. However, there is much we do not know in this area, including the effects of compression upon lymphatic flow and drainage. Imaging and measuring capabilities are improving in this respect, but are often expensive and time-consuming. This, coupled with the unknown effects of individual, diurnal and seasonal variances on compression efficacy, means that future research should focus upon ways to monitor the pressure delivered by a garment, and its effects upon the fluids we are trying to control. More is known about the possible This paper will describe the vascular Key words effects of compression on the anatomy of the upper limb and axilla, pathophysiology of lymphoedema when and will outline current understanding of Anatomy used on the lower limbs (Partsch and normal and abnormal lymph drainage. It Physiology Junger, 2006). While some of these will also explain the mechanism of action Lymphatics principles can be applied to guide the use of compression garments and will detail Compression of compression on the upper body, it is the effects of compression on fluid important that the practitioner is movement. knowledgeable about the anatomy and physiology of the upper limb, axilla and Vascular drainage of the upper limb thorax, and of the anatomical and vascular It is helpful to have an understanding of Little evidence exists to support the differences that exist between the upper the vascular drainage of the upper limb, use of compression garments in the and lower limb, so that the effects of these since the lymphatic drainage follows a treatment of lymphoedema, particularly differences can be considered when using similar course (Figure 1). -
Hand and Arm Guidelines After Your Axillary Lymph Node Dissection
PATIENT & CAREGIVER EDUCATION Hand and Arm Guidelines After Your Axillary Lymph Node Dissection This information describes how to prevent infection and reduce swelling in your hand and arm after your axillary lymph node dissection surgery. Following these guidelines may help prevent lymphedema. About Your Lymphatic System Figure 1. Normal lymph drainage Figure 1. Normal lymph drainage Your lymphatic system has 2 jobs: It helps fight infection. It helps drain fluid from areas of your body. Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1). Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products. Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes. Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases. Axillary lymph nodes are a group of lymph nodes in your armpit (axilla) that drain the lymph fluid from your breast and arm. Everyone has a different number of axillary lymph nodes. An axillary lymph node dissection is a surgery to remove a group of axillary lymph nodes. Hand and Arm Guidelines After Your Axillary Lymph Node Dissection 1/5 About Lymphedema Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema. -

Spontaneous Infarction of Superficial Lymph Nodes
J Clin Pathol: first published as 10.1136/jcp.25.8.689 on 1 August 1972. Downloaded from J. clin. Path., 1972, 25, 689-696 Spontaneous infarction of superficial lymph nodes J. DOUGLAS DAVIES AND A. G. STANSFELD' From the Department of Histopathology, St Bartholomew's Hospital, London SYNOPSIS Five cases of extensive infarction of lymph nodes were traced in just over 16 years' surgical material. All presented with painful swelling in a superficial lymph node chain. None was diagnosed clinically; two were interpreted as fibroadenoma of the axillary tail of the breast, and two as a femoral hernia. Microscopically the lymph nodes in the first three weeks after infarction were characterized by extensive necrosis of medullary and cortical lymphoid cells, but the central reticulin architecture and a narrow, incomplete rim of viable subcapsular lymphoid tissue were preserved. Reactive perinodal inflammation and the formation of granulation tissue resembled the reaction to myocardial infarction. The late stage of the lesion was characterized by incomplete regeneration of lymphoid tissue in the lymph nodes. The lesions appeared attributable to thrombosis of veins within the substance and the hila of the nodes. Though experimental infarction of lymph nodes has were stained by Harris' haematoxylin and eosin, and been produced in dogs (Holman and Self, 1938; Gordon and Sweet's method for reticulin. When Tilak and Howard, 1964; Kister, Conklin, and appropriate PAS, Gram, or Ziehl-Neelsen prepara- copyright. Habif, 1965) and rabbits (Osogoe and Courtice, tions were examined. 1968), spontaneous infarction of previously normal lymph nodes in man has rarely been recorded Case Reports (Holman and Self, 1938). -
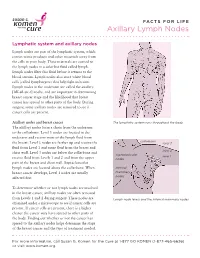
Axillary Lymph Nodes
FACTS FOR LIFE Axillary Lymph Nodes Lymphatic system and axillary nodes Lymph nodes are part of the lymphatic system, which carries waste products and other materials away from the cells in your body. These materials are carried to the lymph nodes in a colorless fluid called lymph. Lymph nodes filter this fluid before it returns to the blood stream. Lymph nodes also store white blood cells (called lymphocytes) that help fight infection. Lymph nodes in the underarm are called the axillary [AK-sil-air-e] nodes, and are important in determining breast cancer stage and the likelihood that breast cancer has spread to other parts of the body. During surgery, some axillary nodes are removed to see if cancer cells are present. Axillary nodes and breast cancer The lymphatic system runs throughout the body. The axillary nodes form a chain from the underarm to the collarbone. Level 1 nodes are located in the underarm and receive most of the lymph fluid from collarbone the breast. Level 2 nodes are farther up and receive the level 3 fluid from Level 1 and some fluid from the breast and level 2 chest wall. Level 3 nodes are below the collarbone and supraclavicular level 1 receive fluid from Levels 1 and 2 and from the upper nodes part of the breast and chest wall. Supraclavicular lymph nodes are located above the collarbone. When internal breast cancer develops, Level 1 nodes are usually mammary affected first. nodes To determine whether or not lymph nodes are involved in the breast cancer, axillary nodes are often removed from Levels 1 and 2 during surgery. -

Axillary Lymph Nodes and Breast Cancer
AXILLARY LYMPH NODES Lymphatic system and axillary nodes The lymphatic system runs through the body. It carries lymph from tissues and organs to lymph nodes. Lymph nodes are small clumps of immune cells that act as filters for the lymphatic system. They also store white blood cells that help fight illness. The lymph nodes in the underarm are called axillary lymph nodes. If breast cancer spreads, this is the first place it’s likely to go. During breast surgery, some axillary nodes may be removed to see if they contain cancer. This helps determine breast cancer stage and guide treatment. Lymph node status is related to tumor size. The larger the tumor, the more likely it is the breast cancer has spread to the lymph nodes (lymph node-positive). Sentinel node biopsy To see if cancer has spread to the axillary lymph nodes, The lymphatic system runs through the body. most people have a sentinel node biopsy. Before or during the procedure, a radioactive substance (called a tracer) and/ or a blue dye is injected into the breast. The first lymph supraclavicular nodes nodes to absorb the tracer or dye are called the sentinel nodes. These are also the first lymph nodes where breast cancer is likely to spread. internal mammary The surgeon removes the sentinel nodes and sends them nodes to the lab. When the surgeon removes the sentinel nodes, it doesn’t mean there’s cancer in the nodes. It means a pathologist needs to check the nodes for cancer. If the nodes contain cancer, more lymph nodes may be removed. -

Reactive Axillary Lymphadenopathy to COVID-19 Vaccination on F18-FDG PET/CT
J of Nuclear Medicine Technology, first published online April 5, 2021 as doi:10.2967/jnmt.121.262008 Reactive Axillary Lymphadenopathy to COVID-19 Vaccination on F18-FDG PET/CT Mathew V. Smith, M.D., Ming Yang, M.D.* Department of Radiology, Mayo Clinic Arizona. *Corresponding Author: Ming Yang, MD Department of Radiology Mayo Clinic Arizona 13400 E Shea BLVD Scottsdale, AZ 85259 E-mail: Yang.ming#mayo.edu Tel: 480-342-0988 Disclosure: Neither author has interest conflict. Grant support: None Number of words: 742 Immediate Open Access: Creative Commons Attribution 4.0 International License (CC BY) allows users to share and adapt with attribution, excluding materials credited to previous publications. License: https://creativecommons.org/licenses/by/4.0/. Details: https://jnm.snmjournals.org/page/permissions. Abstract: In this report, we present F18-FDG PET/CT findings of reactive left axillary and supraclavicular hypermetabolic lymphadenopathy, as well as ipsilateral delta muscle injection site radiotracer uptake related to recent COVID-19 vaccination in a patient with osteosarcoma. With growing number of patients receiving COVID-19 vaccine, recognition of benign characteristic F18-FDG PET/CT image findings will ensure staging/restaging accuracy and avoid unnecessary biopsy. Keywords: COVID-19; Vaccination, Lymphadenopathy Running title: Reactive Axillary Lymphadenopathy to Vaccination Introduction: Reactive lymphadenopathy is a recognized side effect related to vaccination. With mRNA based COVID-19 vaccines, efficacy depends on the activation of dendritic cells after administration. These activated antigen presenting cells must then migrate to the draining lymph nodes and present the translated protein to the nodal based B and T cells in order to create robust humoral and cell mediated adaptive immunity (1). -

Bilateral Axillary Lymphadenopathy: Differential Diagnosis and Management
CASE REPORT https://doi.org/10.29289/25945394202020200036 Bilateral axillary lymphadenopathy: differential diagnosis and management Paula Clarke1* , Carolina Nazareth Valadares1 , Débora Balabram1,2 , Douglas de Miranda Pires1 ABSTRACT Lymphonodopathy is an increase in volume and/or changes in the characteristics of lymph nodes, and it can be caused by benign or malignant diseases. Appropriate physical examination should define their clinical characteristics, and, if needed, complementary imaging or anatomopathological tests should be performed for diagnostic definition. In the present article, we report the case of a female patient, with sarcoidosis, who presented axillary lymph node disease, and the exams that followed until the diagnostic conclusion. KEYWORDS: sarcoidosis; lymphadenopathy; lymph nodes; breast diseases; tuberculosis, lymph node. INTRODUCTION investigation, as well as histological aspects and clinical infor- Axillary lymphadenopathy is characterized by an increase in vol- mation on the most frequent differential diagnoses. ume or changes in lymph node morphology.1 It can be detected with palpation on physical examination or alteration in imaging tests. Normal lymph nodes on a mammogram (MMG) are usu- CASE REPORT ally oval or reniform and have a radiolucent center, represent- This is a case report of a patient attended at the Medical Specialties ing hilar fat. On ultrasound (US) imaging, the cortex is usually Center of Santa Casa de Belo Horizonte (SCBH). A bibliographic hypoechoic or even imperceptible, and the medulla is hyperechoic. review was carried out on the PubMed database using the descrip- Once compromised, either by benign or malignant diseases, the tors “axilla”, “lymphadenopathy”, “granulomatous lymphadeni- lymph node changes its shape and structure, showing different tis”, “breast sarcoidosis”, “sarcoidosis” and “occult breast cancer”. -

Axillary Lymphadenectomy
CHAPTER 3 Axillary Lymphadenectomy CRITICAL ELEMENTS O Identifi cation of Anatomical Structures for Level I and II Axillary Dissection O Removal of Level III Nodes O Removal of Rotter Nodes O Removal of a Suffi cient Number of Lymph Nodes for Axillary Staging O Identifi cation and Preservation of the Long Thoracic, Thoracodorsal, and Medial Pectoral Nerves O Identifi cation and Preservation of the Second and Third Intercostobrachial Nerves O Drain Placement 1A. IDENTIFICATION OF ANATOMICAL STRUCTURES FOR LEVEL I AND II AXILLARY DISSECTION Recommendation:Recomm Identifi cation of the axillary vein and latissimus dorsi, pecto- ralis major, pectoralis minor, serratus anterior, and subscapularis muscles is essential for the resection of suffi cient level I and II axillary nodes for breast cancer staging and adjuvant treatment planning. TypeType ofof Data: Retrospective case series . StrengthStreng of Recommendation: The consensus of the group supports this guideline based on historic evidence. Rationale Breast cancer typically spreads to the axillary lymph nodes fi rst, and axillary dissec- tion is important for both local control and treatment planning. The anatomic borders of the axilla must be identifi ed to adequately resect level I and II axillary lymph nodes (see Fig. 3-1). The axilla is a triangular space that is delineated by the axillary vein 49 Copyright © 2015 Wolters Kluwer Health, Inc. Unauthorized reproduction of the article is prohibited. 004_ACS_Ch03.indd4_ACS_Ch03.indd 4499 44/3/15/3/15 22:41:41 AAMM 50 SECTION I | BREAST Pectoralis