Spontaneous Infarction of Superficial Lymph Nodes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Axillary Lymph Nodes in Breast Cancer Patients: Sonographic Evaluation*
Pinheiro DJPCArtigo et al. / deLinfonodos Revisão axilares – avaliação ultrassonográfica Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica* Axillary lymph nodes in breast cancer patients: sonographic evaluation Denise Joffily Pereira da Costa Pinheiro1, Simone Elias2, Afonso Celso Pinto Nazário3 Pinheiro DJPC, Elias S, Nazário ACP. Linfonodos axilares em pacientes com câncer de mama: avaliação ultrassonográfica. Radiol Bras. 2014 Jul/Ago; 47(4):240–244. Resumo O estadiamento axilar nas pacientes portadoras de câncer de mama inicial é fator essencial no planejamento terapêutico. Atualmente este é realizado durante o tratamento cirúrgico, mas há uma tendência em buscar técnicas pré-operatórias e de menor morbidade para avaliação dos linfonodos axilares. A ultrassonografia é um exame amplamente usado para esta finalidade e muitas vezes associado a punção aspirativa por agulha fina ou por agulha grossa. Entretanto, os critérios ultrassonográficos de suspeição para linfonodos axilares não apresentam valores preditivos significativos, gerando resultados discrepantes em estudos sobre sensibilidade e especificidade do método. O objetivo deste trabalho é realizar uma revisão na literatura médica sobre a ultrassonografia no estadiamento axilar e as principais alterações morfológicas do linfonodo metastático. Unitermos: Câncer de mama; Linfonodos axilares; Ultrassonografia; Aspectos morfológicos. Abstract Axillary staging of patients with early-stage breast cancer is essential in the treatment planning. Currently such staging is intraoperatively performed, but there is a tendency to seek a preoperative and less invasive technique to detect lymph node metastasis. Ultrasonography is widely utilized for this purpose, many times in association with fine-needle aspiration biopsy or core needle biopsy. However, the sonographic criteria for determining malignancy in axillary lymph nodes do not present significant predictive values, producing discrepant results in studies evaluating the sensitivity and specificity of this method. -
Impact of the Number of Dissected Axillary Lymph Nodes on Survival
ISSN: 2643-4563 Nabil et al. Int J Oncol Res 2019, 2:015 DOI: 10.23937/2643-4563/1710015 Volume 2 | Issue 1 International Journal of Open Access Oncology Research RESEARCH ARTICLE Impact of the Number of Dissected Axillary Lymph Nodes on Survival in Breast Cancer Patients Emad Eldin Nabil1, Ahmed M Maklad2,3, Ashraf Elyamany4,5*, Emad Gomaa6 and Moamen M Ali3,7 1Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 2Clinical Oncology and Nuclear Medicine Department, Sohag University Hospitals, Egypt 3King Fahad Medical City, Riyadh, KSA 4 Medical Oncology Department, SECI, Assiut University, Egypt Check for updates 5King Saud Medical City, Riyadh, KSA 6General Surgery Department, Sohag University Hospitals, Egypt 7Medical Physics, Radiation Oncology Department, SECI, Assiut University, Egypt *Corresponding author: Ashraf Elyamany, Medical Oncology Department, SECI, Assiut University, Egypt; King Saud Medical City, Riyadh, KSA Abstract regard median OS for patients having more than 10 LN excised was for N0, N1, N2, N3 5.57, 5.94, 4.97, 4.61 years Background: For patients with breast cancer, axillary dis- respectively while in the other group having less than 10 LN section was a standard treatment, especially with patient excised OS was 5.4, 5.14, 5.14 years respectively with P = with positive metastases in the sentinel nodes. For some 0.117. Regarding Lymphedema There was highly significant patients axillary dissection might be over-treatment, includ- difference between both arms p value 0.000, with higher ing those who have had a mastectomy. Especially with grades in arm I (moderate 17 cases and 6 cases severe the new trend of many radiation-therapy centers, provide edema). -

Microlymphatic Surgery for the Treatment of Iatrogenic Lymphedema
Microlymphatic Surgery for the Treatment of Iatrogenic Lymphedema Corinne Becker, MDa, Julie V. Vasile, MDb,*, Joshua L. Levine, MDb, Bernardo N. Batista, MDa, Rebecca M. Studinger, MDb, Constance M. Chen, MDb, Marc Riquet, MDc KEYWORDS Lymphedema Treatment Autologous lymph node transplantation (ALNT) Microsurgical vascularized lymph node transfer Iatrogenic Secondary Brachial plexus neuropathy Infection KEY POINTS Autologous lymph node transplant or microsurgical vascularized lymph node transfer (ALNT) is a surgical treatment option for lymphedema, which brings vascularized, VEGF-C producing tissue into the previously operated field to promote lymphangiogenesis and bridge the distal obstructed lymphatic system with the proximal lymphatic system. Additionally, lymph nodes with important immunologic function are brought into the fibrotic and damaged tissue. ALNT can cure lymphedema, reduce the risk of infection and cellulitis, and improve brachial plexus neuropathies. ALNT can also be combined with breast reconstruction flaps to be an elegant treatment for a breast cancer patient. OVERVIEW: NATURE OF THE PROBLEM Clinically, patients develop firm subcutaneous tissue, progressing to overgrowth and fibrosis. Lymphedema is a result of disruption to the Lymphedema is a common chronic and progres- lymphatic transport system, leading to accumula- sive condition that can occur after cancer treat- tion of protein-rich lymph fluid in the interstitial ment. The reported incidence of lymphedema space. The accumulation of edematous fluid mani- varies because of varying methods of assess- fests as soft and pitting edema seen in early ment,1–3 the long follow-up required for diagnosing lymphedema. Progression to nonpitting and irre- lymphedema, and the lack of patient education versible enlargement of the extremity is thought regarding lymphedema.4 In one 20-year follow-up to be the result of 2 mechanisms: of patients with breast cancer treated with mastec- 1. -

M. H. RATZLAFF: the Superficial Lymphatic System of the Cat 151
M. H. RATZLAFF: The Superficial Lymphatic System of the Cat 151 Summary Four examples of severe chylous lymph effusions into serous cavities are reported. In each case there was an associated lymphocytopenia. This resembled and confirmed the findings noted in experimental lymph drainage from cannulated thoracic ducts in which the subject invariably devdops lymphocytopenia as the lymph is permitted to drain. Each of these patients had com munications between the lymph structures and the serous cavities. In two instances actual leakage of the lymphography contrrult material was demonstrated. The performance of repeated thoracenteses and paracenteses in the presenc~ of communications between the lymph structures and serous cavities added to the effect of converting the. situation to one similar to thoracic duct drainage .The progressive immaturity of the lymphocytes which was noted in two patients lead to the problem of differentiating them from malignant cells. The explanation lay in the known progressive immaturity of lymphocytes which appear when lymph drainage persists. Thankful acknowledgement is made for permission to study patients from the services of Drs. H. J. Carroll, ]. Croco, and H. Sporn. The graphs were prepared in the Department of Medical Illustration and Photography, Dowristate Medical Center, Mr. Saturnino Viloapaz, illustrator. References I Beebe, D. S., C. A. Hubay, L. Persky: Thoracic duct 4 Iverson, ]. G.: Phytohemagglutinin rcspon•e of re urctcral shunt: A method for dccrcasingi circulating circulating and nonrecirculating rat lymphocytes. Exp. lymphocytes. Surg. Forum 18 (1967), 541-543 Cell Res. 56 (1969), 219-223 2 Gesner, B. M., J. L. Gowans: The output of lympho 5 Tilney, N. -

Lymphatic Drainage of the Breast: from Theory to Surgical Practice
Int. J. Morphol., 27(3):873-878, 2009. Lymphatic Drainage of the Breast: from Theory to Surgical Practice Drenaje Linfático de la Mama: desde la Teoría a la Práctica Quirúrgica *José Humberto Tavares Guerreiro Fregnani & **José Rafael Macéa FREGNANI, J. H. T. G. & MACÉA, J. R. Lymphatic drainage of the breast: from theory to surgical practice. Int. J. Morphol., 27(3):873-878, 2009. SUMMARY: Until recently, complete removal of axillary lymph nodes was performed as part of the treatment of breast cancer. Sentinel lymph node biopsy (SLNB) in selected cases has reduced the number of cases of wide axillary dissection and the related morbidity. Knowledge of breast lymphatic drainage is essential for understanding the principles behind SLNB and also for performing safe and correct axillary lymphonodectomy. This paper describes in detail the anatomical issues relating to breast lymphatic drainage and the correlated axillary and extra-axillary lymph nodes. In addition, it shows the application of this theoretical knowledge to surgical practice, especially with regard to SLNB and lymphonodectomy. The surgical nomenclature is compared with the current International Anatomical Terminology. KEY WORDS: Lymphatic drainage, Sentinel lymph node biopsy, Breast cancer. INTRODUCTION Breast cancer is the most frequent type of tumor changes to the sensitivity of the upper limb, posterior scapular among women, accounting for approximately one quarter dislocation (winged scapula syndrome), brachial plexus of all tumors in women. It has been estimated that more than lesions, axillary vessel thrombosis and lesions, skin necrosis one million new cases occur worldwide annually. Breast and pectoral muscle atrophy, among others (Torresan et al., cancer is responsible for significant morbidity and mortality 2002; Kim et al., 2006). -

Anatomy and Physiology in Relation to Compression of the Upper Limb and Thorax
Clinical REVIEW anatomy and physiology in relation to compression of the upper limb and thorax Colin Carati, Bren Gannon, Neil Piller An understanding of arterial, venous and lymphatic flow in the upper body in normal limbs and those at risk of, or with lymphoedema will greatly improve patient outcomes. However, there is much we do not know in this area, including the effects of compression upon lymphatic flow and drainage. Imaging and measuring capabilities are improving in this respect, but are often expensive and time-consuming. This, coupled with the unknown effects of individual, diurnal and seasonal variances on compression efficacy, means that future research should focus upon ways to monitor the pressure delivered by a garment, and its effects upon the fluids we are trying to control. More is known about the possible This paper will describe the vascular Key words effects of compression on the anatomy of the upper limb and axilla, pathophysiology of lymphoedema when and will outline current understanding of Anatomy used on the lower limbs (Partsch and normal and abnormal lymph drainage. It Physiology Junger, 2006). While some of these will also explain the mechanism of action Lymphatics principles can be applied to guide the use of compression garments and will detail Compression of compression on the upper body, it is the effects of compression on fluid important that the practitioner is movement. knowledgeable about the anatomy and physiology of the upper limb, axilla and Vascular drainage of the upper limb thorax, and of the anatomical and vascular It is helpful to have an understanding of Little evidence exists to support the differences that exist between the upper the vascular drainage of the upper limb, use of compression garments in the and lower limb, so that the effects of these since the lymphatic drainage follows a treatment of lymphoedema, particularly differences can be considered when using similar course (Figure 1). -

Patterns of Lymphatic Drainage in the Adultlaboratory
J. Anat. (1971), 109, 3, pp. 369-383 369 With 11 figures Printed in Great Britain Patterns of lymphatic drainage in the adult laboratory rat NICHOLAS L. TILNEY Department of Surgery, Peter Bent Brigham Hospital, and Harvard Medical School, Boston, Massachusetts (Accepted 27 April 1971) INTRODUCTION This study was undertaken to define and elucidate patterns of lymphatic drainage in the adult laboratory rat. The incentive for the work arose from investigations into the role of regional lymphatics in the sensitization of the host by skin allografts. It has become clear that the response of rats to antigens, investigated increasingly in the available inbred strains, requires an accurate knowledge of lymphoid anatomy and lymphatic drainage routes. Examinations of the lymphatics of specific body areas of the rat have appeared sporadically in the literature, but descriptions of regional drainage patterns, especially of peripheral sites, are unavailable. Previous investigations by Job (1919), Greene (1935) and Sanders & Florey (1940) have con- centrated primarily upon the location of the lymphoid tissues. Miotti (1965) has stressed visceral drainage, and Higgins (1925) has described the lymphatic system of the newborn rat. A more complete definition of both somatic and visceral lymphatic routes is presented. MATERIALS AND METHODS One hundred and thirty normal adult rats of both sexes, each weighing between 150 and 300 g, were studied. The animals came from five strains: each inbred - Oxford strains of the albino (AO), hooded (HO), agouti (DA), and F1 hybrid of the HO and DA strains - and 'stock' animals from a closed outbred albino colony. Under ether anaesthesia, the site for cutaneous injection was clipped or a serous cavity entered for visceral injection. -

Extension of Cervical Cancer to the Superficial Inguinal Lymph Nodes
5 Junie 1965 S.A. TYDSKRIF VIR OBSTETRIE E GINEKOLOGIE 23 assessed and controlled. Adequate control in patients with REFERENCES 1. Kirk. H. H. (1958): J. Obstet. Gynaec. Brit. Emp.. 6S. 387. Addison's disease appears (a) to enhance the fertility, (b) 2. Fitzpatrick. K. G. (1922): Surg. Gynec. Obstet., 35, 72. to reduce the risk at the time of delivery and (c) to im 3. Brent. F. (1950): Amer. J. Surg.. 79. 645. 4. Rolland. C. F .. Matthews. J. D. and Matthew. G. D. (1953): J. prove the prospects of successful breast feeding. Obstet. Gynaec. Brit. Emp.. 60. 57. 5. Francis. H. H. and Forster. J. C. (1958): Proc. Roy. Soc. Med.. SI. 513. SUMMARY 6. Browne. F. J. and Browne. J. C. McClure (1963): Briris" Obstetric Practice, 3rd ed.. p. 484. London: Heinemann. 7. O·Sullivan. D. (1954): J. Irish Med. Assoc.. 36, 315. A case is presented of a 26-year-old patient known to have 8. Sluder. H. M. (1959): Amer. J. Obstet. Gynec.. 78, 808. Addison's disease who became pregnant. 9. Allahbadia. N. K. (1960): J. Obstet. Gynaec. Brit. Emp.. 67, 641. 10. Papper. E. M. and Cahill. G. F. (1952): J. Amer. Med. Assoc., Careful antenatal and intrapartum supervision by both 148. 174. 11. Jailer. J. W. and Knowlton. A. I. (1950): J. Clin. Invest.. 29, 1430. physician and obstetrician ensures that the patient has the 12. Moore. F. H. and Freedman. J. R. (1956): Amer. J. Obstet. Gynec.. best chance of a successful outcome. 72. 1340. 13. Gabrilove. J. L. and Schval. -
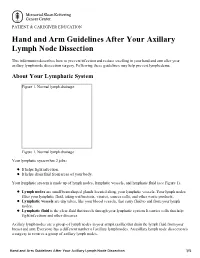
Hand and Arm Guidelines After Your Axillary Lymph Node Dissection
PATIENT & CAREGIVER EDUCATION Hand and Arm Guidelines After Your Axillary Lymph Node Dissection This information describes how to prevent infection and reduce swelling in your hand and arm after your axillary lymph node dissection surgery. Following these guidelines may help prevent lymphedema. About Your Lymphatic System Figure 1. Normal lymph drainage Figure 1. Normal lymph drainage Your lymphatic system has 2 jobs: It helps fight infection. It helps drain fluid from areas of your body. Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1). Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products. Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes. Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases. Axillary lymph nodes are a group of lymph nodes in your armpit (axilla) that drain the lymph fluid from your breast and arm. Everyone has a different number of axillary lymph nodes. An axillary lymph node dissection is a surgery to remove a group of axillary lymph nodes. Hand and Arm Guidelines After Your Axillary Lymph Node Dissection 1/5 About Lymphedema Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema. -

Analysis of Lymphatic Drainage in Various Forms of Leg Edema Using Two Compartment Lymphoscintigraphy
43 Lymphology 31 (1998) 43-55 ANALYSIS OF LYMPHATIC DRAINAGE IN VARIOUS FORMS OF LEG EDEMA USING TWO COMPARTMENT LYMPHOSCINTIGRAPHY P. Brautigam, E. FOldi, I. Schaiper, T. Krause, W. Vanscheidt, E. Moser Abteilung Nuklearmedizin, Radiol. University Klinik Freiburg (PB,TK,EM), FOldiklinik, Fachklinik ftir lymphologische Erkrankungen, Hinterzarten (EF), Zentrum ftir Nuklearmedizin, Paracelsus- Klinik Osnabrtick (IS), and Universitats-Hautklinik, Freiburg (WV), Germany ABSTRACT was reduced. Patients with lipedema (obesity) scintigraphically showed no alteration in The anatomical and functional status lymphatic transport. of the epifascial and subfascial lymphatic This study demonstrates that lymphatic compartments was analyzed using two drainage is notably affected (except in obesity compartment lymphoscintigraphy in five termed lipedema) in various edemas of the leg. groups of patients (total 55) with various Lymphatic drainage varied depending on the forms of edema of the lower extremities. specific compartment and the pathophysiologic Digital whole body scintigraphy enabled mechanism accounting for the edema. Two semiquantitative estimation of radio tracer compartment lymphoscintigraphy is a valuable transport with comparison of lymphatic diagnostic tool for accurate assessment of leg drainage between those individuals without edema of known and unknown origin. (normal) and those with leg edema by calculating the uptake of the radiopharma- The lymphatic system is deranged in ceutical transported to regional lymph nodes. various forms of leg edema of both lymphatic A visual assessment of the lymphatic drainage and non-lymphatic origin including venous- pathways of the legs was also performed. lymphedema, cyclic idiopathic edema, and In patients with cyclic idiopathic edema, lipedema (obesity) (1,2). As no discrete an accelerated rate of lymphatic transport differences exist on clinical grounds among was detected (high lymph volume overload or the various edema syndromes, differential dynamic insufficiency). -

Lymph Flow in Human Leg Kiyoshi Seki
Lymphology 12 (I 979) 2- 3 Lymph Flow in Human Leg Kiyoshi Seki 3rd Dept. Internal Medicine, Toho University, Tokyo, Japan Summary Clearance rate of subcutaneously injected A little bit of RJSA (0.01 - 0.02 ml) was injected into RJSA was rapid in cardiac, nephrotic and he a lymphatic at t11e back of a human foot in supine patic edema and slow in lymphedema (2, 3). and/or sitting position, and U1e radioactivity curves From this it was assumed that lymph flow were obtained at the inguinal and/or at the middle of U1e thigh. Radioactivity curves at the inguinal region was rapid or increased in cardiac edema as in showed stepwise rise with the frequency of about nephrotic and hepatic edema. I /min. in subjects without edema and steep rise without staircase in patients with cardiac edema. ln tissue clearance of RISA, the subjects are Radioactivity curves at the middle of the thigh showed hospitalized and kept in bed as quiet as many spiky waves with the frequency of about 1/min. possible. However, as the observations are in supine subjects without edema, which were increased carried out 2 to 3 days long, effect of the in frequency, duration and/or height in sitting subjects without edema and also in supine and sitting patients movement of the subjects on the lymph flow with cardiac edema. may not be neglibly small. Therefore, it may Therefore, it may be said that there are rhythmic lymph be difficult to compare the results by dye Oows in lower leg of subjects without edema and of injection method with those by tissue clearan patients with cardiac edema not only in supine but ce of RJSA. -
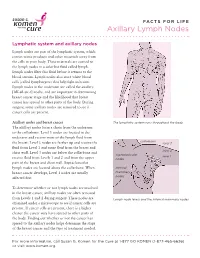
Axillary Lymph Nodes
FACTS FOR LIFE Axillary Lymph Nodes Lymphatic system and axillary nodes Lymph nodes are part of the lymphatic system, which carries waste products and other materials away from the cells in your body. These materials are carried to the lymph nodes in a colorless fluid called lymph. Lymph nodes filter this fluid before it returns to the blood stream. Lymph nodes also store white blood cells (called lymphocytes) that help fight infection. Lymph nodes in the underarm are called the axillary [AK-sil-air-e] nodes, and are important in determining breast cancer stage and the likelihood that breast cancer has spread to other parts of the body. During surgery, some axillary nodes are removed to see if cancer cells are present. Axillary nodes and breast cancer The lymphatic system runs throughout the body. The axillary nodes form a chain from the underarm to the collarbone. Level 1 nodes are located in the underarm and receive most of the lymph fluid from collarbone the breast. Level 2 nodes are farther up and receive the level 3 fluid from Level 1 and some fluid from the breast and level 2 chest wall. Level 3 nodes are below the collarbone and supraclavicular level 1 receive fluid from Levels 1 and 2 and from the upper nodes part of the breast and chest wall. Supraclavicular lymph nodes are located above the collarbone. When internal breast cancer develops, Level 1 nodes are usually mammary affected first. nodes To determine whether or not lymph nodes are involved in the breast cancer, axillary nodes are often removed from Levels 1 and 2 during surgery.