STANDARDIZED PROCEDURE HIGH RESOLUTION ANOSCOPY (HRA) (Adults, Peds)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -

Lower Gastrointestinal Tract
Lower Gastrointestinal Tract Hemorrhoids—Office Management and Review for Gastroenterologists Mitchel Guttenplan, MD, FACS 1 and Robert A Ganz, MD, FASGE 2 1. Medical Director, CRH Medical Corp; 2. Minnesota Gastroenterology, Chief of Gastroenterology, Abbott-Northwestern Hospital, Associate Professor of Medicine, University of Minnesota Abstract symptomatic hemorrhoids and anal fissures are very common problems. This article provides a review of the anatomy and physiology of the anorectum along with a discussion of the diagnosis and treatment of hemorrhoids and the commonly associated matters of anal sphincter spasm and fissures. The various office treatment modalities for hemorrhoids are discussed, as are the specifics of rubber band ligation (rBL), and a strategy for the office treatment of these problems by the gastroenterologist is given. The crh o’regan system™ is a technology available to the gastroenterologist that provides a safe, effective, and efficient option for the non-surgical treatment of hemorrhoids in the office setting. Keywords hemorrhoids, anal fissure, rubber band ligation, crh o’regan system™ Disclosure: Mitchel guttenplan is Medical Director of crh Medical Products corporation, the manufacturer of the crh o’regan system™. robert A ganz is a consultant to and holds equity in crh Medical Products corporation. Received: 2 november 2011 Accepted: 30 november 2011 Citation: Touchgastroentorology.com ; December, 2011. Correspondence: Mitchel guttenplan, MD, fAcs, 3000 old Alabama rd, suite 119 #183, Alpharetta, gA 30022-8555, us. e: [email protected] Diseases of the anorectum, including hemorrhoids and anal fissures, are experience also makes it clear that hemorrhoid sufferers frequently very common. The care of these entities is typically left to general and have additional anorectal issues that may both confuse the diagnosis colorectal surgeons. -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -
Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -
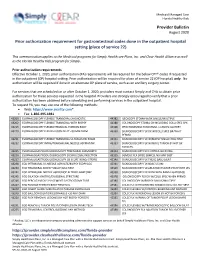
Provider Bulletin Prior Authorization Requirement for Gastrointestinal
Medicaid Managed Care Florida Healthy Kids Provider Bulletin August 2020 Prior authorization requirement for gastrointestinal codes done in the outpatient hospital setting (place of service 22) This communication applies to the Medicaid programs for Simply Healthcare Plans, Inc. and Clear Health Alliance as well as the Florida Healthy Kids program for Simply. Prior authorization requirements Effective October 1, 2020, prior authorization (PA) requirements will be required for the below CPT® codes if requested in the outpatient (OP) hospital setting. Prior authorization will be required for place of service 22 (OP hospital) only. No authorization will be required if done in an alternate OP place of service, such as an ancillary surgery center. For services that are scheduled on or after October 1, 2020, providers must contact Simply and CHA to obtain prior authorization for these services requested in the hospital. Providers are strongly encouraged to verify that a prior authorization has been obtained before scheduling and performing services in the outpatient hospital. To request PA, you may use one of the following methods: Web: https://www.availity.com* Fax: 1-866-495-1981 43200 ESOPHAGOSCOPY FLEXIBLE TRANSORAL DIAGNOSTIC 44382 ILEOSCOPY STOMA W/BX SINGLE/MULTIPLE 43202 ESOPHAGOSCOPY FLEXIBLE TRANSORAL WITH BIOPSY 44388 COLONOSCOPY STOMA DX INCLUDING COLLJ SPEC SPX 43215 ESOPHAGOSCOPY FLEXIBLE REMOVAL FOREIGN BODY 45308 PROCTOSGMDSC RIGID RMVL 1 LESION CAUTERY 43220 ESOPHAGOSCOPY FLEX BALLOON DILAT <30 MM DIAM 45330 SIGMOIDOSCOPY -

APG Regulations
FINAL as of 8/22/08 Pursuant to the authority vested in the Commissioner of Health by Section 2807(2-a) of the Public Health Law, Part 86 of Title 10 of the Official Compilation of Codes, Rules and Regulations of the State of New York, is amended by adding a new Subpart 86-8, to be effective upon filing with the Secretary of State, to read as follows: SUBPART 86-8 OUTPATIENT SERVICES: AMBULATORY PATIENT GROUP (Statutory authority: Public Health Law § 2807(2-a)(e)) Sec. 86-8.1 Scope 86-8.2 Definitions 86-8.3 Record keeping, reports and audits 86-8.4 Capital reimbursement 86-8.5 Administrative rate appeals 86-8.6 Rates for new facilities during the transition period 86-8.7 APGs and relative weights 86-8.8 Base rates 86-8.9 Diagnostic coding and rate computation 86-8.10 Exclusions from payment 86-8.11 System updating 86-8.12 Payments for extended hours of operation § 86-8.1 Scope (a) This Subpart shall govern Medicaid rates of payments for ambulatory care services provided in the following categories of facilities for the following periods: (1) outpatient services provided by general hospitals on and after December 1, 2008; (2) emergency department services provided by general hospitals on and after January 1, 2009; (3) ambulatory surgery services provided by general hospitals on and after December 1, 2008; (4) ambulatory services provided by diagnostic and treatment centers on and after March 1, 2009; and (5) ambulatory surgery services provided by free-standing ambulatory surgery centers on and after March 1, 2009. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

The Cutting Edge Fall 2008
DOSNL-FALL08b 11/12/08 9:46 PM Page 1 At the Cutting Edge of Surgical Excellence t is my great pleasure to introduce department has taken a leading role in the Ithe first issue of At the Cutting Edge application to general surgery of robotic — newsletter for the Department of technologies, already widely used in urology Surgery at the University of Illinois at and gynecology. Currently a true revolution Chicago. As the new Head of the is taking place at UIC. Complex procedures Department of Surgery, I am partic- such as hepatectomy, Whipple’s, lung resec- ularly proud to share with you the tion, mediastinal tumor excision, and gastric recent achievements of our surgical staff. The resection are routinely done in a minimally department has some of the most talented invasive fashion thanks to the genius of surgeons in the country, in line with a Professor Giulianotti and the most advanced remarkable tradition of excellence. robotic technology. The opening of the The Department of Surgery at the “Advanced Robotic Training Center” will University of Illinois was brought to the fore- allow Professor Giulianotti and his team to front by Warren H. Cole, who was the contribute to the robotic training of other Department Head between 1936 and 1966. faculties and our surgical residents. An In those years, the Department of Surgery impressive number of surgical leaders from was ranked within the top five in the country. the USA, Europe and Asia are currently com- His successor was Lloyd M. Nyhus, Head of ing to Chicago to learn from the best in the Department of Surgery from 1967 to robotic surgery. -

CRS Case Log Coding
CODE DESCRIPTION Procedure Category Defined Case Category 46288 Fistula, advancement flap repair, skin or mucosal Anorectal Procedures Endorectal Advancement Flap Fistulotomy, fistula repair 46020 Fistula, seton placement only Anorectal Procedures Fistulotomy, fistula repair 46030 Fistula, seton/drain removal Anorectal Procedures Fistulotomy, fistula repair 46045 Fistulotomy, LIFT Anorectal Procedures Fistulotomy, fistula repair 46280 Fistulotomy, primary, secondary, + seton, NOS Anorectal Procedures Fistulotomy, fistula repair 46706 Fistula, repair, fibrin glue Anorectal Procedures Fistulotomy, fistula repair 46707 Fistula, repair, plug Anorectal Procedures Fistulotomy, fistula repair 46710 Fistula, repair, ileoanal anastomosis, perineal any Anorectal Procedures Fistulotomy, fistula repair 46712 Fistula, repair, ileoanal anastomosis, abdomino-perineal Anorectal Procedures Fistulotomy, fistula repair 57300 Fistula, rectovaginal repair, transanal or transvaginal Anorectal Procedures Fistulotomy, fistula repair 57305 Fistula, rectovaginal repair, abdominal Anorectal Procedures Fistulotomy, fistula repair 57307 Fistula, rectovaginal repair, abdominal, ostomy Anorectal Procedures Fistulotomy, fistula repair 46221 Hemorrhoids, internal, rubberband ligation RBL Anorectal Procedures Hemorrhoidectomy-excisional any kind, PPH 46250 Hemorrhoidectomy, external, simple Anorectal Procedures Hemorrhoidectomy-excisional any kind, PPH 46260 Hemorrhoidectomy, internal Anorectal Procedures Hemorrhoidectomy-excisional any kind, PPH 46320 Hemorrhoidectomy, -

Anal Cancer Early Detection, Diagnosis, and Staging Detection and Diagnosis
cancer.org | 1.800.227.2345 Anal Cancer Early Detection, Diagnosis, and Staging Detection and Diagnosis Finding cancer early often allows for more treatment options. Some early cancers may cause signs and symptoms that can be noticed, but that's not always the case. ● Can Anal Cancer Be Found Early? ● Signs and Symptoms of Anal Cancer ● Tests for Anal Cancer Staging After a cancer diagnosis, staging provides important information about the extent of cancer in the body and anticipated response to treatment. ● Anal Cancer Stages ● Anal Cancer Survival Rates Questions to Ask About Anal Cancer Here are some questions you can ask your cancer care team to help you better understand your cancer diagnosis and treatment options. ● Questions to Ask About Anal Cancer 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Can Anal Cancer Be Found Early? Many anal cancers can be found early. Early anal cancers often have signs and symptoms that lead people to see a doctor. Unfortunately, some anal cancers may not cause symptoms until they reach an advanced stage. Other anal cancers can cause symptoms like those of diseases other than cancer. This may delay their diagnosis. Anal cancers develop in a part of the digestive tract that your doctor can easily see and get to. A digital rectal exam (DRE) can find some cases of anal cancer early. In this exam, the doctor inserts a gloved, lubricated finger into the anus to feel for unusual lumps or growths. This test is sometimes used to look for prostate cancer in men (because the prostate gland can be felt through the rectum). -
Evaluation and Management of Common Anorectal Complaints
Thomas Jefferson University Jefferson Digital Commons Department of Family & Community Medicine Presentations and Grand Rounds Department of Family & Community Medicine 8-20-2020 Evaluation and Management of Common Anorectal Complaints Krys Foster, MD, MPH Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/fmlectures Part of the Family Medicine Commons, and the Primary Care Commons Let us know how access to this document benefits ouy Recommended Citation Foster, MD, MPH, Krys, "Evaluation and Management of Common Anorectal Complaints" (2020). Department of Family & Community Medicine Presentations and Grand Rounds. Paper 438. https://jdc.jefferson.edu/fmlectures/438 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Family & Community Medicine Presentations and Grand Rounds by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Evaluation and Management of Common Anorectal -

Acute Lower Gastrointestinal Bleeding
The new england journal of medicine Clinical Practice Caren G. Solomon, M.D., M.P.H., Editor Acute Lower Gastrointestinal Bleeding Ian M. Gralnek, M.D., M.S.H.S., Ziv Neeman, M.D., and Lisa L. Strate, M.D., M.P.H. This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the authors’ clinical recommendations. From the Institute of Gastroenterology A 71-year-old woman with hypertension, hypercholesterolemia, and ischemic heart and Hepatology (I.M.G.) and Medical disease, who had a cardiac stent placed 4 months earlier, presents to the emergency Imaging Institute (Z.N.), Emek Medical Center, Afula, and Rappaport Faculty of department with multiple episodes of red or maroon-colored stool mixed with clots Medicine, Technion–Israel Institute of Tech during the preceding 24 hours. Current medications include atenolol, atorvastatin, nology, Haifa (I.M.G.) — both in Israel; aspirin (81 mg daily), and clopidogrel. On physical examination, the patient is dia- and the Department of Medicine, Divi sion of Gastroenterology, University of phoretic. While she is in a supine position, the heart rate is 91 beats per minute and Washington School of Medicine, Seattle the blood pressure is 106/61 mm Hg; while she is sitting, the heart rate is 107 beats (L.L.S.). Address reprint requests to Dr. per minute and the blood pressure is 92/52 mm Hg. The remainder of the examina- Gralnek at the Institute of Gastroenterol ogy and Hepatology, Emek Medical Cen tion is unremarkable, except for maroon-colored stool on digital rectal examination.