Versatility and Importance of Bichat's Fat Pad in Dentistry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

29360-Oral Cavity Dr. Alexandra Borges.Pdf
ORAL CAVITY: ANATOMY AND PATHOLOGIES Alexandra Borges, MD COI Disclosure Instituto Português de Oncologia de Lisboa I have nothing to disclose Champalimaud Foundation Lisbon, Portugal ECHNNR 2021 ECHNNR 2021 MR ANATOMY LEARNING OBJECTIVES • Become familiar with OC anatomy and the importance of using adequate terminology when reporting OC studies NASOPHARYNX NASAL CAVITY • Learn how to tailor imaging studies • Understand the different patterns of malignant tumor spread according to the different tumor subsites OROPHARYNX ORAL CAVITY HYPOPHARYNX BOUNDARIES CONTENTS: ORAL TONGUE Superior: • hard palate • superior alveolar ridge Inferior: • floor of the mouth • inferior alveolar ridge ITM Laterally: • cheeks and buccal mucosaosa Anterior: • Lips Posterior: • oropharynx ORAL TONGUE: Extrinsic tongue muscles EM: Styloglossus tongue retraction and elevation Styloglossus Palatoglossus Hyoglossus SG Geniglossus HG GG CN XII CN X EM: Palatoglossus elevation of the tongue EM: Hyoglossus tongue depression and retraction EM: Genioglossus tongue protrusion ORAL TONGUE: Extrinsic muscles GG GH TONGUE INNERVATION ORAL CAVITY IX sensitive and Spatial subdivision taste CN X Motor • Mucosal area • Tongue root • Sublingual space CN XII Motor • Submandibular space Lingual nerve: Sensitive (branch of V3) • Buccomasseteric region Taste (chorda tympani) ORAL MUCOSAL SPACE ROOT OF THE TONGUE 1. Lips 2. Gengiva (sup. alveolar ridge) 3. Gengiva (inf. alveolar ridge) 4. Buccal 5. Palatal 6. Sublingual/FOM 7. Retromolar trigone GG 8. Tongue ROT BOT Vestibule GH Mucosa -

Head and Neck
DEFINITION OF ANATOMIC SITES WITHIN THE HEAD AND NECK adapted from the Summary Staging Guide 1977 published by the SEER Program, and the AJCC Cancer Staging Manual Fifth Edition published by the American Joint Committee on Cancer Staging. Note: Not all sites in the lip, oral cavity, pharynx and salivary glands are listed below. All sites to which a Summary Stage scheme applies are listed at the begining of the scheme. ORAL CAVITY AND ORAL PHARYNX (in ICD-O-3 sequence) The oral cavity extends from the skin-vermilion junction of the lips to the junction of the hard and soft palate above and to the line of circumvallate papillae below. The oral pharynx (oropharynx) is that portion of the continuity of the pharynx extending from the plane of the inferior surface of the soft palate to the plane of the superior surface of the hyoid bone (or floor of the vallecula) and includes the base of tongue, inferior surface of the soft palate and the uvula, the anterior and posterior tonsillar pillars, the glossotonsillar sulci, the pharyngeal tonsils, and the lateral and posterior walls. The oral cavity and oral pharynx are divided into the following specific areas: LIPS (C00._; vermilion surface, mucosal lip, labial mucosa) upper and lower, form the upper and lower anterior wall of the oral cavity. They consist of an exposed surface of modified epider- mis beginning at the junction of the vermilion border with the skin and including only the vermilion surface or that portion of the lip that comes into contact with the opposing lip. -

Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone Tissue Engineering
Adipose Stem Cells from Buccal Fat Pad and Abdominal Adipose Tissue for Bone tissue Engineering Elisabet Farré Guasch Dipòsit Legal: B-25086-2011 ISBN: 978-90-5335-394-3 http://hdl.handle.net/10803/31987 ADVERTIMENT. La consulta d’aquesta tesi queda condicionada a l’acceptació de les següents condicions d'ús: La difusió d’aquesta tesi per mitjà del servei TDX (www.tesisenxarxa.net) ha estat autoritzada pels titulars dels drets de propietat intel·lectual únicament per a usos privats emmarcats en activitats d’investigació i docència. No s’autoritza la seva reproducció amb finalitats de lucre ni la seva difusió i posada a disposició des d’un lloc aliè al servei TDX. No s’autoritza la presentació del seu contingut en una finestra o marc aliè a TDX (framing). Aquesta reserva de drets afecta tant al resum de presentació de la tesi com als seus continguts. En la utilització o cita de parts de la tesi és obligat indicar el nom de la persona autora. ADVERTENCIA. La consulta de esta tesis queda condicionada a la aceptación de las siguientes condiciones de uso: La difusión de esta tesis por medio del servicio TDR (www.tesisenred.net) ha sido autorizada por los titulares de los derechos de propiedad intelectual únicamente para usos privados enmarcados en actividades de investigación y docencia. No se autoriza su reproducción con finalidades de lucro ni su difusión y puesta a disposición desde un sitio ajeno al servicio TDR. No se autoriza la presentación de su contenido en una ventana o marco ajeno a TDR (framing). -

Basic Histology (23 Questions): Oral Histology (16 Questions
Board Question Breakdown (Anatomic Sciences section) The Anatomic Sciences portion of part I of the Dental Board exams consists of 100 test items. They are broken up into the following distribution: Gross Anatomy (50 questions): Head - 28 questions broken down in this fashion: - Oral cavity - 6 questions - Extraoral structures - 12 questions - Osteology - 6 questions - TMJ and muscles of mastication - 4 questions Neck - 5 questions Upper Limb - 3 questions Thoracic cavity - 5 questions Abdominopelvic cavity - 2 questions Neuroanatomy (CNS, ANS +) - 7 questions Basic Histology (23 questions): Ultrastructure (cell organelles) - 4 questions Basic tissues - 4 questions Bone, cartilage & joints - 3 questions Lymphatic & circulatory systems - 3 questions Endocrine system - 2 questions Respiratory system - 1 question Gastrointestinal system - 3 questions Genitouirinary systems - (reproductive & urinary) 2 questions Integument - 1 question Oral Histology (16 questions): Tooth & supporting structures - 9 questions Soft oral tissues (including dentin) - 5 questions Temporomandibular joint - 2 questions Developmental Biology (11 questions): Osteogenesis (bone formation) - 2 questions Tooth development, eruption & movement - 4 questions General embryology - 2 questions 2 National Board Part 1: Review questions for histology/oral histology (Answers follow at the end) 1. Normally most of the circulating white blood cells are a. basophilic leukocytes b. monocytes c. lymphocytes d. eosinophilic leukocytes e. neutrophilic leukocytes 2. Blood platelets are products of a. osteoclasts b. basophils c. red blood cells d. plasma cells e. megakaryocytes 3. Bacteria are frequently ingested by a. neutrophilic leukocytes b. basophilic leukocytes c. mast cells d. small lymphocytes e. fibrocytes 4. It is believed that worn out red cells are normally destroyed in the spleen by a. neutrophils b. -

Salivary Glands; the Parotid Submandibular and Sublingual Functions of Saliva
Lecture series Gastrointestinal tract Professor Shraddha Singh, Department of Physiology, KGMU, Lucknow Various secretions from GIT First secretion from GIT that encounter the food is SALIVARY SECRETIONS What is saliva • Saliva is the mixed glandular secretion which constantly bathes the teeth and the oral mucosa • First secretion encounter the food • It is vital for oral health • It is constituted by the secretions of the three paired major salivary glands; The Parotid Submandibular and Sublingual Functions of saliva 1. Defense: a. Antibacterial b. Antifungal c.Immunological 2. Digestive function: a. Digestive enzymes – ptyalin, lipase b. Formation of bolus c. Taste 3. Protective function: a. Protective coating for hard tissues-teeth b. Protective coating for soft tissues 4. Lubricative function: a.Keeps the oral cavity moist b.Facilitates speech c.Helps in mastication and swallowing 5. Buffering function Salivary glands Structure of Salivary Gland Parotid gland • Parotid is large accounts for 50% secretion of saliva • Situated in front of ear behind the ramus of mandible • Gland drain in to oral cavity opposite to second molar tooth • Secretions are basically serous Submandibular and Sub lingual gland • The submandibular gland is about half the size of the parotid gland • It lies above the mylohyoid in the floor of the mouth. It opens into the floor of the mouth underneath the anterior part of the tongue • The sublingual is the smallest of the paired major salivary glands, being about one fifth the size of the submandibular. • It -

The Buccal Fat Pad: Importance and Function
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 6 Ver. XIII (June. 2016), PP 79-81 www.iosrjournals.org The Buccal Fat Pad: Importance And Function Ulduz Zamani Ahari1, Hosein Eslami2, Parisa Falsafi*2, Aila Bahramian2, Saleh Maleki1 1. Post Graduate Student Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. 2.Department Of Oral Medicine, Dental Faculty, Tabriz University Of Medical Science, Tabriz, Iran. ●Corresponding Author Email:[email protected] Abstract: The buccal fat is an important anatomic structure intimately related to the masticatory muscles, facial nerve , and parotid duct.while anatomically complex , an understanding of its boundaries will allow the surgeon to safely manipulate this structure in reconstructive and aesthetic procedures . Technically, the buccal fat pad is easily accessed and moblized . It is does not cause any noticeable defect in the cheek or mouth, and it can be performed in a very short time and without causing complication for the patient. The pedicled BFP graft is more resistant to infection than other kinds of free graft and will result in very success. The buccal fat pad has a satisfactory vascular supply , This property of graft and other properties will allow for the closure of defects that cannot be repaired by conventional procedures. The buccal fat pad exposed through an intraoral and buccal incision , has several clinical application including aesthetic improvement , close of oroantral and Oroantral defects reconstruction of surgical defects and palatal cleft defects and palatal cleft defects , reconstruction of maxilla and palatal defects. -

Oral & Maxillofacial Surgery Removal of Parotid Salivary Gland
Oxford University Hospitals NHS Trust Oral & Maxillofacial Surgery Removal of parotid salivary gland Information for patients This leaflet will help you understand your treatment and should answer many of the questions patients commonly ask before surgery for the removal of a parotid gland. A member of staff will be available if you would like further explanation and to answer any other questions that the leaflet does not cover. What is the parotid gland? The parotid gland lies in front of and below the earlobe. It produces saliva. Saliva drains from the parotid gland through a tube that opens on the inside of the cheek, opposite the upper back teeth. Why do I need my gland removed? The most common reason for removing a parotid gland (or part of the gland) is because a lump has been found inside it. There are also other reasons which your surgeon will discuss with you. What happens before the operation? Pre-assessment clinic – You will be asked to attend an appointment at this clinic. Nursing and/or medical staff will go through some important checks and make certain all relevant investigations have been completed well in advance of the operation date. Admission – You will normally be asked to come to Theatre Direct Admissions or Litchfield Day Surgery Unit on the morning of your operation. The anaesthetist will see you to explain the anaesthetic and answer any questions you may have. They will also be able to advise you about pain relief available after the operation. The surgeon will explain the details of the operation and discuss the possible risks, before asking you to sign a consent form (this may be done at the pre-assessment appointment). -

The Oromaxillofacial Rehabilitation in Orthodontic-Surgical Protocols
DOI: 10.1051/odfen/2015044 J Dentofacial Anom Orthod 2016;19:203 © The authors The oromaxillofacial rehabilitation in orthodontic-surgical protocols Th. Gouzland1,2, M. Fournier1 1 Kinesiologist, specializing in oromaxillofacial rehabilitation 2 Educator SUMMARY Oro-maxillo-facial rehabilitation is an ancient practice that has developed over recent years through research and integration with physiotherapists in multidisciplinary teams, as is the case with orthodontic- surgical procedures. At the same time, the progress made in orthognathic and orthodontic surgery over the last 20 years encourages more and more patients to undergo surgery. Preoperative treatment is based on early assessment and preparation for optimal surgical conditions to come up with a functional plan. A short stay in a hospital, focusing on rehabilitation, is recommended. During the postoperative phase, the key objectives are to ensure the muscles and arteries all function perfectly, acceptance of the new face, and the immediate correction of any orofacial dyspraxia that has occurred during myofunc- tional therapy. The various specialists in this multidisciplinary team must constantly be in communication. The importance of postoperative physiotherapy will be illustrated by a study consisting of 35 cases of maxillomandibular osteotomy with orthodontic preparation and monitoring. The purpose of this study is to show occurrence of suboccipital and cervical muscle tensions as well as masticatory muscles. Then we will be able to see the importance of these practices, the impact on recovery, the impact on posture and how best to treat. KEYWORDS Physiotherapy, orthognathic surgery, orthodontic, myofunctional therapy, muscles, posture INTRODUCTION The progress made in the techniques and comfortable recovery. This fits into and the results obtained by coupling the current social view where one’s orthognathic surgery with orthodontics image is given greater importance. -
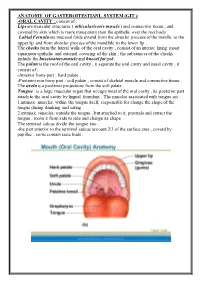
ANATOMY of GASTEROITESTIANL SYSTEM (GIT ): Consist of : ORAL CAVITY
ANATOMY OF GASTEROITESTIANL SYSTEM (GIT ): -ORAL CAVITY : consist of : Lips are muscular structures ( orbicularis oris muscle ) and connective tissue , and covered by skin which is more transparent than the epithelia over the rest body . Labial Fernula are mucosal folds extend from the alveolar process of the maxilla to the upper lip and from alveolar process of the mandible to the lower lip . The cheeks form the lateral walls of the oral cavity , consist of an interior lining moist squamous epithelia and external covering of the skin , the substances of the cheeks include the buccinators muscle and buccal fat pad. The palate is the roof of the oral cavity , it separate the oral cavity and nasal cavity , it consist of : -Anterior bony part : hard palate . -Posterior non bony part : soft palate , consist of skeletal muscle and connective tissue . The uvela is a posterior projections from the soft palate . Tongue : is a large muscular organ that occupy most of the oral cavity , its posterior part attach to the oral cavity by lingual frenulum . The muscles associated with tongue are : 1.intrinsic muscles: within the tongue itself, responsible for change the shape of the tongue during drinking and eating . 2.extrinsic muscles: outside the tongue , but attached to it, protrude and retract the tongue , move it from side to side and change its shape . The terminal sulcus divide the tongue into : -the part anterior to the terminal sulcus account 2/3 of the surface area , coverd by papillae , some contain taste buds . -the posterior one third is devoid of papillae , has few scattered taste buds , it has few small glands and lymphatic tissue (lingual tissue ) Teeth : adults have 32 teeth distributed in two dental arches, the maxillary arch , and the mandibular arch . -

Wayne County Community College District
Wayne County Community College District COURSE SYLLABUS DHY 111 Histology and Oral Embryology CREDIT HOURS: 3.00 CONTACT HOURS: 45.00 COURSE DESCRIPTION: Basic principles of histology and embryology are reviewed with emphasis on tissues of the oral cavity and contiguous structures. Histology and embryology encompasses the development of the oral facial complex including the formation of the enamel, dentin and pulp, root formation, the attachment apparatus and the eruption and shedding of teeth. PREREQUISITES: DHY 101, DHY 110, DHY 120 EXPECTED COMPETENCIES: Upon completion of this course, the student will be familiar with: • Name the four basic tissues in the body and give an example of where each type is found. • List and give the relative size of various subdivisions of the meter down to the angstrom and give the range of human cell sizes. • Give the function of the following cell parts and organelles. • Relate the structures of the oral cavity with their description or label: • Describe normal gingival including its component parts. • Name the structure that lies under the sublingual fold. • Discuss why dentin formation can continue throughout life but enamel cannot. • List and discuss the types of dentin and cementum. • Describe the functions of cementum. • State the functions of the pulp. • Label the parts of the pulp cavity. • Describe an odontoblast, cementocyte and cemento last. • Name, identify and locate in the body the various types of epithelia both simple and stratified, and pseudostralified. • Name, define and give examples of the various epithelial glands. • Name, describe, compare and locate in the body the various connective tissues. • Name, describe, compare and locate in the body the various types of cartilage. -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

Rare Coexistence of Sialolithiasis and Actinomycosis in the Submandibular Gland
Case Report ENT Updates 2016;6(3):148–151 doi:10.2399/jmu.2016003010 Rare coexistence of sialolithiasis and actinomycosis in the submandibular gland O¤uzhan Dikici1, Nuray Bayar Muluk2 1Department of Otorhinolaryngology, fievket Y›lmaz Training and Research Hospital, Bursa, Turkey 2Department of Otorhinolaryngology, Faculty of Medicine, K›r›kkale University, K›r›kkale, Turkey Abstract Özet: Submandibüler bezde siyalolityaz ve aktinomikozun seyrek görülen birlikteli¤i Sialolithiasis is a condition characterized by the obstruction of salivary Siyalolityaz, tükürük bezi veya boflalt›m kanal›n›n bir tafl veya siyalolit gland or its excretory duct by a calculus or sialolith. This condition pro- ile t›kanmas› ile karakterizedir. Bu durum etkilenmifl bezin fliflmesi, a¤- vokes swelling, pain, and infection of affected gland leading to salivary ecta- r›mas› ve enfeksiyonunu teflvik ederek tükürük bezi ektazisine, hatta da- sia and even causing the subsequent dilatation of the salivary gland. The ha sonra tükürük bezinin dilatasyonuna neden olmaktad›r. Bu olgu ra- aim of this case report is to present a rare condition of sialolithiasis of the porunun amac› submandibüler bezde siyalolitle birlikte aktinomikozun submandibular gland with actinomycosis. In this report, we presented a 35- görüldü¤ü nadir bir siyalolityaz olgusunu sunmakt›r. Bu raporda sub- year-old male patient having coexistence of submandibular sialolithiasis mandibüler siyalolit ve aktinomikozu olan 35 yafl›nda erkek hasta litera- and actinomycosis with a literature review. Patient underwent excision of tür taramas› eflli¤inde raporlanm›flt›r. Siyalolityaz nedeniyle sa¤ sub- the right submandibular gland due to siaololithiasis. Pathologic examina- mandibüler bez eksize edilmifltir. Patolojik incelemede gözlemlenen tion revealed chronic sialadenitis, sialolithiasis, actinomyces which all kronik siyaladenit, siyalolityaz ve aktinomiçes nedeniyle çap› 1.5 cm tafl- necessitate the excision of right submandibular gland with stones with 1.5 larla dolu sa¤ submandibüler bezin eksizyonunun gerekti¤i görülmüfl- cm in diameter.