The World Bank
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Crystal Reports
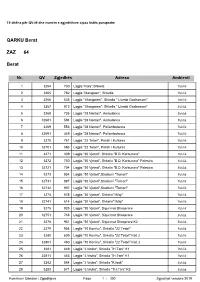
Të dhëna për QV-të dhe numrin e zgjedhësve sipas listës paraprake QARKU Berat ZAZ 64 Berat Nr. QV Zgjedhës Adresa Ambienti 1 3264 730 Lagjia "Kala",Shkolla Publik 2 3265 782 Lagjia "Mangalen", Shkolla Publik 3 3266 535 Lagjia " Mangalem", Shkolla " Llambi Goxhomani" Publik 4 3267 813 Lagjia " Mangalem", Shkolla " Llambi Goxhomani" Publik 5 3268 735 Lagjia "28 Nentori", Ambulanca Publik 6 32681 594 Lagjia "28 Nentori", Ambulanca Publik 7 3269 553 Lagjia "28 Nentori", Poliambulanca Publik 8 32691 449 Lagjia "28 Nentori", Poliambulanca Publik 9 3270 751 Lagjia "22 Tetori", Pallati I Kultures Publik 10 32701 593 Lagjia "22 Tetori", Pallati I Kultures Publik 11 3271 409 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Publik 12 3272 750 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Palestra Publik 13 32721 704 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Palestra Publik 14 3273 854 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 15 32731 887 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 16 32732 907 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 17 3274 578 Lagjia "30 Vjetori", Shkolla"1Maji" Publik 18 32741 614 Lagjia "30 Vjetori", Shkolla"1Maji" Publik 19 3275 925 Lagjia "30 Vjetori", Sigurimet Shoqerore Publik 20 32751 748 Lagjia "30 Vjetori", Sigurimet Shoqerore Publik 21 3276 951 Lagjia "30 Vjetori", Sigurimet Shoqerore K2 Publik 22 3279 954 Lagjia "10 Korriku", Shkolla "22 Tetori" Publik 23 3280 509 Lagjia "10 Korriku", Shkolla "22 Tetori" Kati 2 Publik 24 32801 450 Lagjia "10 Korriku", Shkolla "22 Tetori" Kati 2 Publik 25 3281 649 Lagjia "J.Vruho", -

Inventory of Tourist Facilities and Capacities in Lake Skadar-Shkodra Area
Inventory of tourist facilities and capacities in Lake Skadar-Shkodra area INVENTORY OF TOURIST FACILITIES AND CAPACITIES IN LAKE SKADAR-SHKODRA AREA Prepared by LAKE SKADAR-SHKODRA INTEGRATED ECOSYSTEM MANAGEMENT PROJECT July 2011 1 Inventory of tourist facilities and capacities in Lake Skadar-Shkodra area INTRODUCTION Lake Skadar-Shkodra is the largest lake in the Balkan Peninsula shared between Montenegro and Albania. The Montenegrin part of the lake and its surrounding area were declared a national park in 1983 and in Albania a Managed Nature Reserve. In 1996 in Montenegro and in 2006 in Albania, Skadar-Shkodra Lake was included in the Ramsar list of wetlands of international importance. Lake Skadar is a wonderful place with mirrored waters, rocky shores and wetlands full of wildlife with more than 270 species of birds, plenty of natural herbs, traditional fishing villages, numerous islet monasteries and cultural heritage sites, fascinating beaches surrounded by karst mountains, various amusing, social and cultutral events. Lake Skadar area is where some of the best wines and organic food in Montenegro can be found, cultivated by the local producers especially in Crmnica and Godinje valleys in Montenegro and Shtoj village in Albania. There are also numerous accomodation facilities, restaurants and shopping centers, on the Montenegrin and Labanian sides of the lake that make this area attractive to hiome and foreign tourists. Being a tourist attraction with all these natural and cultural resources the aim of this inventory is to prepare a joint Montenegrin and Albanian inventory on tourist facilities and capacities of Lake Shkodra area, to promote Lake Skadar-Shkodra as a joint tourist attraction internally and internationally. -

The City of Drisht in the Middle Ages Keywords: Drishti, Albania, the Republic of Venice, George II Strazimir, Balsha III, Stefan Lazarevic, George Brankoviq
Volume 5, issue 11, 2016 e-ISSN: 1857-8187 p-ISSN: 1857-8179 Research Article History The City of Drisht in the Middle Ages Keywords: Drishti, Albania, the Republic of Venice, George II Strazimir, Balsha III, Stefan Lazarevic, George Brankoviq. Departament of Medieval Studies, Institute of History “Ali Hadri” Teuta Shala-Peli Prishtina, Republic of Kosova. Abstract The topic "Drishti in the Middle Ages”, includes a period characterized by significant development in the social, economic, cultural and political sphere, not only in the city,but also in Albania in general during the Middle Ages. Drishti as many cities of Albania was founded during the Middle Ages, reaching a high development state whichplaced the city among the ranks of other medieval cities not only in Albania, buteven further in the region. As evidence of these developments are the achievements in the field of legislation, the developments in the economic, social, religious and cultural life. During the Middle Ages, the city of Drisht had reached a significant development in terms of economic, strategic, political, cultural aspect and in many other aspects, playing an important role in the development of important events and processes that characterized medieval Albanian history. In the late XIV century and early XVcentury, Albania and in this case the city of Drisht, entered a new phase due to political changes and developments taking place all over the region. In this period the city was confronted with the efforts of the Republic of Venice to put it under its rule, while facing successive attacks of the Ottoman army. The medieval city of Drisht had reached a high municipal organization alongside the other cities of the time. -

Republika E Shqipërisë Bashkia Shkodër Këshilli Bashkiak
REPUBLIKA E SHQIPËRISË BASHKIA SHKODËR KËSHILLI BASHKIAK N J O F T I M për këshillim me publikun Në mbështetje dhe zbatim të nenit 18 dhe nenit 54 shkronja “k“ të ligjit Nr. 139/2015 “Për vetëqeverisjen vendore“, Këshilli Bashkiak Shkodër njofton zhvillimin e seancës së këshillimit me publikun/ banorë të njësive administrative: Velipojë, Guri i Zi, Bërdicë, Ana Malit, Dajç, për diskutimin e projekt aktit : 1. Për miratimin e Plan veprimit për përmirsimin e shërbimit të kullimit në Bashkinë Shkodër. Takimi do të zhvillohet: në Bashkinë Shkodër ditën e Premte, datë 24 Nëntor 2017, ora 12.30. Bashkëngjitur mund të konsultoni materialin. Jeni të ftuar të merrni pjesë. Duke ju falenderuar. Suel Hadri Sekretar i Këshillit _____________________________________________________________________________________________________________________ Adresa: Rr. 13 Dhjetori, Nr.1 Shkodër, web: www.bashkiashkoder.gov.al, e-mail: [email protected],, BASHKIA SHKODER MIRATOI KRYETAR Voltana Ademi PLANI I VEPRIMIT PER PERMIRESIMIN E SHERBIMIT TE KULLIMI T MENAXHIMI I PERFORMANCES NEPERMJET PERFSHIRJES SE QYTETAREVE NE PROCESIN E KONSULTIMIT, ADVOKIMIT DHE MONITORIMIT ASISTUAR NGA LEVIZ ALBANIA NEPERMJET I.S.D.C SHKODER 2017 1 | P a g e BASHKIA SHKODER 2 | P a g e BASHKIA SHKODER "...Decentralizimi, apo qeverisja e decentralizuar, i referohet ristrukturimit ose riorganizimit të autoritetit në mënyrë që të ketë një sistem të bashkë- përgjegjësisë ndërmjet institucioneve të qeverisjes në nivel qendror, rajonal dhe vendor në përputhje me parimin -

The Genetic Structure of the Population of the Koplik Municipality Calculated by the Isonomy
Journal of Natural Sciences Research www.iiste.org ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.4, No.10, 2014 The Genetic Structure of the Population of the Koplik Municipality Calculated by the Isonomy Ermira Hoxhaj ¹* Zyri Bajrami ¹·² ¹ Departament of Biology – Chemistry,University of Shkodra,Shkodra,Albania. *E-mail:[email protected] ² Departament of Biology,Universiyt of Tirana,Bulevardi Zogu I,Tirana,Albania E-mail:[email protected] Abstract The main focus of this study is the human population of the Municipality of Koplik,in Albania. The city of Koplik is situated 17 km at the North of Shkodra city,in Albania. The genetic structure and connections among the inhabitants of Koplik, have been studied according to the distribution of the surnames of 18831 individuals, identified by 652 surnames, which resulted from the compilation of the genealogical trees.The coefficient of kinship was calculated, because of the isonomy of the case, along with evaluations of the α of Fisher as indicator of the surname variety, evaluations of Fst inbreeding coefficients and evaluations of the Karlin-McGregor`s coefficient. The surname distribution has been calculated based on the logarithm of the surname number and the number of the times such surname is identified. All these parameters have been calculated by means of the data extracted from the genealogical trees in three different methods, based on the surnames inherited from the father, from the mother and a another one, based on casual distribution of the surnames of the same persons,but without considering the genealogical relationship.All these methods show a high value of kinship, but when the three methods are compared, the results have obvious differences. -

(Self) Fashioning of an Ottoman Christian Prince
Amanda Danielle Giammanco (SELF) FASHIONING OF AN OTTOMAN CHRISTIAN PRINCE: JACHIA IBN MEHMED IN CONFESSIONAL DIPLOMACY OF THE EARLY SEVENTEENTH-CENTURY MA Thesis in Comparative History, with a specialization in Interdisciplinary Medieval Studies. Central European University Budapest CEU eTD Collection May 2015 (SELF) FASHIONING OF AN OTTOMAN CHRISTIAN PRINCE: JACHIA IBN MEHMED IN CONFESSIONAL DIPLOMACY OF THE EARLY SEVENTEENTH-CENTURY by Amanda Danielle Giammanco (United States of America) Thesis submitted to the Department of Medieval Studies, Central European University, Budapest, in partial fulfillment of the requirements of the Master of Arts degree in Comparative History, with a specialization in Interdisciplinary Medieval Studies. Accepted in conformance with the standards of the CEU. ____________________________________________ Chair, Examination Committee ____________________________________________ Thesis Supervisor ____________________________________________ Examiner CEU eTD Collection ____________________________________________ Examiner Budapest May 2015 (SELF) FASHIONING OF AN OTTOMAN CHRISTIAN PRINCE: JACHIA IBN MEHMED IN CONFESSIONAL DIPLOMACY OF THE EARLY SEVENTEENTH-CENTURY by Amanda Danielle Giammanco (United States of America) Thesis submitted to the Department of Medieval Studies, Central European University, Budapest, in partial fulfillment of the requirements of the Master of Arts degree in Comparative History, with a specialization in Interdisciplinary Medieval Studies. Accepted in conformance with the standards -

Plani I Zhvillimit Të Sektorit 3 2.6.9 Nënmavriq - Niveli II
AUTORËSIA DHE KONTRIBUTET Ky dokument u hartua në kuadër të projektit "Përgatitja e masterplanit dhe studimeve të fizibilitetit për projekte infrastrukturore në zonën e Alpeve të Shqipërisë" të zbatuar nga Fondi Shqiptar i Zhvillimit, me mbështetjen financiare të Fondit të Përbashkët Evropian të Ballkanit Perëndimor nën kornizën e investimeve në rajon, përfituar nëpërmjet Bankës për Zhvillim të Këshillit të Evropës. Opinionet, gjetjet, konkluzionet dhe rekomandimet e shprehura në këtë dokument janë të autor-it/ve (konsorciumi që përbëhet nga PM Group, Archidata, Globaldit, Instituti i Politikave Publike e Private IP3, Seda) dhe nuk përfaqësojnë domosdoshmërisht ato të kontribuesve në Fondin e Përbashkët Evropian të Ballkanit Perëndimor, të EBRD, si bashkë-menaxher i Fondit të Përbashkët për Ballkanin Perëndimor, apo Bankës për Zhvillim të Këshillit të Evropës si institucion financiar kryesor në lidhje me projektin. EKSPERTËT KRYESORË (KEY EXPERTs) Gabriele Bonafede, udhëheqësi i grupit; Manfred Kojan, ekspert për marketimin dhe turizmin; Max Haberstroh, ekspert i turizmit; David Lyth, ekspert mjedisi; Fredrik Pitzner-Jorgensen, ekonomist për investimet; Ariela Kushi, ekspert i planifikimit urban; Romina Sahiti, ekspert i planifikimit urban; Endri Noçka, ekonomist urban; Gent Nechwatal, ekspert i transportit; Luan Mlloja, ekspert për ujësjellës-kanalizime; Bukurosh Onuzi, ekspert i turizmit; Genc Metohu, ekspert i turizmit; Abdulla Diku, ekspert mjedisi; Artur Galanxhi; ekspert i bujqësisë; Erin Mlloja, ekspert GIS. EKSPERTËT MBËSHTETËS (Non-KEY EXPERTs) Iva Tavanxhiu, ekspert i planifikimit urban; Orinda Biba, ekspert mjedisi; Kreshnik Bajraktari, ekspert transporti; Besmira Vishe, ekspert ligjor. 2 Alpet e Shqipërisë, 2031 P ËRMbAJTJA 1. HYRJE ............................................................................................................................. 8 1.1 ZONA NË STUDIM DHE POZICIONI RAJONAL .......................................................... 9 1.2 KONSIDERATA NGA PPK DHE STRATEGJIA KOMbËTARE E TURIZMIT ................. -

“Talk” on Albanian Territories (1392–1402)
Doctoral Dissertation A Model to Decode Venetian Senate Deliberations: Pregadi “Talk” on Albanian Territories (1392–1402) By: Grabiela Rojas Molina Supervisors: Gerhard Jaritz and Katalin Szende Submitted to the Medieval Studies Department Central European University, Budapest In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Medieval Studies, Budapest, Hungary 2020 CEU eTD Collection To my parents CEU eTD Collection Table of Contents Acknowledgments .................................................................................................................................. 1 List of Maps, Charts and Tables .......................................................................................................... 2 Introduction ............................................................................................................................................ 3 A Survey of the Scholarship ........................................................................................................................... 8 a) The Myth of Venice ........................................................................................................................... 8 b) The Humanistic Outlook .................................................................................................................. 11 c) Chronicles, Histories and Diaries ..................................................................................................... 14 d) Albania as a Field of Study ............................................................................................................. -

GEF/UNDP/GWP-MED Projetc “Enabling Transboundary Cooperation and Integrated Water Resources Management in the Extended Drin River Basin”
GEF/UNDP/GWP-MED Projetc “Enabling Transboundary Cooperation and Integrated Water Resources Management in the Extended Drin River Basin” In the framework of the Memorandum of Understanding for the Management of the Extended Transboundary Drin Basin Pilot activity “Preparation of Wastewater Management Decision Support Tool” Wastewater management solutions in the Shkodra city Shtojcë 3: ITUN qendror apo ITUN të vegjël për vendbanimet përqark liqenit të Shkodrës 1 The Coordinated Action for the implementation of the Memorandum of Understanding for the management of the Drin basin (Drin CORDA) is supported by the GEF Drin Project. Thus, the latter constitutes an institutional project implemented by the United Nations Development Programme (UNDP) and executed by the Global Water Partnership (GWP) through GWP-Mediterranean (GWP- Med), in cooperation with the United Nations Economic Commission for Europe (UNECE). The Drin Core Group (DCG), being the multilateral body responsible for the implementation of the Memorandum of Understanding serves as the Steering Committee of the Project. GWP-Med serves as the Secretariat of the DCG. Disclaimer: The document adheres to the UN rules and policies regarding the names and international status of countries and/or other geographical areas etc. The use of characterizations, names, maps or other geographical statements in this document in no way implies any political view or positions of the Parties which are executing and implementing the Project. 2 PËRMBAJTJA PËRMBAJTJA......................................................................................................................................... -

P9. Arsimi Parauniversitar Dhe Edukimi
P9. Arsimi parauniversitar dhe edukimi "Mbështetja e veprimit administrativ dhe komunitar për të promovuar dhe mbrojtur qytetarët, duke u dhënë mundësi për formim kulturor e profesional, për t’u marrë me sport e argëtime, për t’u kujdesur për veten e mjedisin, për cilësi më të mirë të jetesës.” P9. Arsimi parauniversitar dhe edukimi 3 1. Hyrje 3 2. Politikat e zhvillimit 3 3. Funksionet: 4 3.1. F1. Ndërtimin, rehabilitimin dhe mirëmbajtjen e ndërtesave arsimore të sistemit shkollor parauniversitar; 4 3.1.1. Aktivitetet dhe projektet që planifikohen në përmbushje të objektivit P9.F1.O1 4 3.1.2. Aktivitetet dhe projektet që planifikohen në përmbushje të objektivit P9.F1.O2 11 3.2. F2. Administrimi dhe rregullimi i sistemit arsimor parashkollor në kopshte. 11 3.2.1. Aktivitetet dhe projektet që planifikohen në përmbushje të objektivit F2.O1: 12 3.2.2. Aktivitetet dhe projektet që planifikohen në përmbushje të objektivit F2.O2: 13 3.3. F3. Organizimin e aktiviteteve kulturore dhe promovimin e identitetit kombëtar e lokal, si dhe administrimin e objekteve që lidhen me ushtrimin e këtyre funksioneve. 13 3.3.1. Aktivitetet dhe projektet që planifikohen në përmbushje të objektivit P9.F3.O1 14 4. Buxhetimi i programit Arsimi parauniversitar dhe edukimi. 14 5. Projektet dhe aktivitetet e planifikuara për Arsimi parauniversitar dhe Kopshtet. 16 P9. Arsimi parauniversitar dhe edukimi 1. Hyrje Sistemi arsimor ka rëndësi të madhe në rritjen e zhvillimit ekonomik dhe social të komunitetit tonë. Shkolla duhet t’i mundësojë çdo fëmijë që të ketë rezultate të kënaqshme në mësime, të jetë i sigurtë, i shëndetshëm dhe aktiv në jetën komunitare. -

Paketa Fiskale
BASHKIA SHKODËR Paketa Fiskale Paketa fiskale do të paraqitet për miratim pas bashkëpunimit, propozimeve dhe sugjerimeve te marra me të gjithë grupet e interesit të përfshira në kete proces. Ajo harmonizon dhe mundëson trajtimin e drejtë me taksa dhe tarifa për gjithë gamën e larmishme të bizneseve e familjeve, me aktivitete dhe vendodhje në zona me funksione të ndryshme, duke siguruar njëkohësisht të ardhurat për plotësimin e misioneve të bashkise ndaj qytetarëve të saj. Prioritetet e saj kryesore janë: nivele minimale taksash për bizneset dhe familjet, tarifa të ulëta dhe të referuara drejt kostos së shërbimit të dhënë, shpërndarje e drejtë e ngarkesës fiskale, pagesa të shpejta dhe sa më pranë taksapaguesit, fatura të thjeshta dhe të kuptueshme, transparencë dhe shërbim cilësor. Aprovimi i saj mundëson përmirësimin e mëtejshëm të shërbimeve që ofron bashkia ndaj qytetarëve të saj, si dhe realizimin e objektivave madhorë ne funksion të zhvillimit të qëndrueshëm të gjithë zonës. Prioritete Bashkia Shkoder ka në fokus: Ruajtjen e klimes se mire te biznesit (konkurrences e ndershme, uljen e evazionit fiskal, shpërndarjes së drejtë të tarifave) Trajtimit te biznesit si partner Lehtesirave per bizneset prodhuese dhe me rendesi te veçante strategjike Shërbimit sa me prane te tatimpaguesit Lehtesimin dhe thjeshtimin e proçedurave dhe tarifave Shperndarjen sa më fair te taksave dhe tarifave Rritje e transparencës dhe bashkëpunimit me tatimpaguesit. Sqarim: Në këtë Paketë Fiskale: Njësi Administrative Shkodër quhet zona urbane qe zinte Bashkia Shkodër përpara ndarjes territoriale sipas Ligjit Nr. 115/2014 "Për ndarjen administrativo-territoriale të njësive të qeverisjes vendore në Republikën e Shqipërisë. Njësi Administrative të tjera quhen zonat sipas tabelës së mëposhtme që ishin komuna përpara ndarjes territoriale sipas Ligjit Nr. -

Berat ZAZ 64 QARKU Berat
Të dhëna për QV-të dhe numrin e zgjedhësve sipas listës paraprake QARKU Berat ZAZ 64 Berat Nr. QV Zgjedhës Adresa Ambienti 1 3264 730 Lagjia "Kala",Shkolla Publik 2 3265 782 Lagjia "Mangalen", Shkolla Publik 3 3266 535 Lagjia " Mangalem", Shkolla " Llambi Goxhomani" Publik 4 3267 813 Lagjia " Mangalem", Shkolla " Llambi Goxhomani" Publik 5 3268 735 Lagjia "28 Nentori", Ambulanca Publik 6 32681 594 Lagjia "28 Nentori", Ambulanca Publik 7 3269 553 Lagjia "28 Nentori", Poliambulanca Publik 8 32691 449 Lagjia "28 Nentori", Poliambulanca Publik 9 3270 751 Lagjia "22 Tetori", Pallati I Kultures Publik 10 32701 593 Lagjia "22 Tetori", Pallati I Kultures Publik 11 3271 409 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Publik 12 3272 750 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Palestra Publik 13 32721 704 Lagjia "30 Vjetori", Shkolla "B.D. Karbunara" Palestra Publik 14 3273 854 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 15 32731 887 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 16 32732 907 Lagjia "30 Vjetori",Stadiumi "Tomori" Publik 17 3274 578 Lagjia "30 Vjetori", Shkolla"1Maji" Publik 18 32741 614 Lagjia "30 Vjetori", Shkolla"1Maji" Publik 19 3275 925 Lagjia "30 Vjetori", Sigurimet Shoqerore Publik 20 32751 748 Lagjia "30 Vjetori", Sigurimet Shoqerore Publik 21 3276 951 Lagjia "30 Vjetori", Sigurimet Shoqerore K2 Publik 22 3279 954 Lagjia "10 Korriku", Shkolla "22 Tetori" Publik 23 3280 509 Lagjia "10 Korriku", Shkolla "22 Tetori" Kati 2 Publik 24 32801 450 Lagjia "10 Korriku", Shkolla "22 Tetori" Kati 2 Publik 25 3281 649 Lagjia "J.Vruho",