CTGT Req Form 07302018.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CADASIL Testing
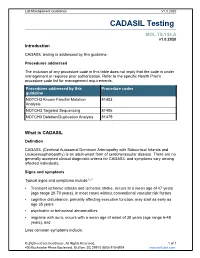
Lab Management Guidelines V1.0.2020 CADASIL Testing MOL.TS.144.A v1.0.2020 Introduction CADASIL testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline NOTCH3 Known Familial Mutation 81403 Analysis NOTCH3 Targeted Sequencing 81406 NOTCH3 Deletion/Duplication Analysis 81479 What is CADASIL Definition CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy) is an adult-onset form of cerebrovascular disease. There are no generally accepted clinical diagnostic criteria for CADASIL and symptoms vary among affected individuals. Signs and symptoms Typical signs and symptoms include1,2,3 Transient ischemic attacks and ischemic stroke, occurs at a mean age of 47 years (age range 20-70 years), in most cases without conventional vascular risk factors cognitive disturbance, primarily affecting executive function, may start as early as age 35 years psychiatric or behavioral abnormalities migraine with aura, occurs with a mean age of onset of 30 years (age range 6-48 years), and Less common symptoms include: © 2020 eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 recurrent seizures with onset in middle age, usually secondary to stroke acute encephalopathy, with a mean age of onset of 42 years Life expectancy for men with CADASIL is reduced by approximately five years and for women by 1 to 2 years.4 Diagnosis Brain Magnetic Resonance Imaging (MRI) findings include T2-signal-abnormalities in the white matter of the temporal pole and T2-signal-abnormalities in the external capsule and corpus callosum.1,2 CADASIL is suspected in an individual with the clinical signs and MRI findings. -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

Clinical and Genetic Characterisation of Hereditary Motor Neuropathies
Clinical and genetic characterisation of hereditary motor neuropathies Boglarka Bansagi Institute of Genetic Medicine January 2017 A Thesis submitted for the degree of Doctor of Philosophy at Newcastle University 'I dare do all that may become a man; who dares do more is none.' (Shakespeare) „Szívet vagy mundért cserélhet az is, ki házat, hazát holtig nem cserél, de hű maradhat idegenben is, kiben népe mostoha sorsa él.” (Tollas Tibor) Author’s declaration This Thesis is submitted to Newcastle University for the degree of Doctor of Philosophy at Newcastle University. I, Boglarka Bansagi, confirm that the work presented in this Thesis is my own. Where information has been derived from other sources, it has been indicated in the Thesis. I can confirm that none of the material offered in this Thesis has been previously submitted by me for a degree or qualification in this or any other university. Abstract Inherited peripheral neuropathies or Charcot-Marie-Tooth disease (CMT) are common neuromuscular conditions, characterised by distal motor atrophy and weakness with variable range of sensory impairment and classified according to demyelinating (CMT1) or axonal (CMT2) pathology. The number of genes causing CMT has rapidly increased due to improved genetic testing technology, even though gene identification has remained challenging in some subgroups of CMT. Hereditary motor neuropathies (HMN) encompass heterogeneous groups of disorders caused by motor axon and neuron pathology. The distal hereditary motor neuropathies (dHMN) are rare length-dependent conditions, which show significant clinical and genetic overlap with motor neuron diseases. Several (>30) causative genes have been identified for ~20% of dHMN patients, which predicts extreme genetic heterogeneity in this group. -

Ursodeoxycholic Acid in Advanced Polycystic Liver Disease: a Phase 2 Multicenter Randomized Controlled Trial
Research Article Ursodeoxycholic acid in advanced polycystic liver disease: A phase 2 multicenter randomized controlled trial Hedwig M.A. D’Agnolo1, Wietske Kievit2, R. Bart Takkenberg3, Ioana Riaño4, Luis Bujanda4, ⇑ Myrte K. Neijenhuis1, Ellen J.L. Brunenberg5, Ulrich Beuers3, Jesus M. Banales4, Joost P.H. Drenth1, 1Department of Gastroenterology and Hepatology, Radboud University Medical Center, Nijmegen, The Netherlands; 2Radboud University Medical Center, Radboud Institute for Health Sciences, Nijmegen, The Netherlands; 3Department of Gastroenterology and Hepatology, Amsterdam Medical Center, Amsterdam, The Netherlands; 4Department of Liver and Gastrointestinal Diseases, Biodonostia Research Institute – Donostia University Hospital, University of the Basque Country (UPV/EHU), IKERBASQUE, CIBERehd, San Sebastián, Spain; 5Department of Radiation Oncology, Radboud University Medical Center, Nijmegen, The Netherlands Background & Aims: Ursodeoxycholic acid (UDCA) inhibits pro- (p = 0.493). LCV was not different after 24 weeks between con- liferation of polycystic human cholangiocytes in vitro and hepatic trols and UDCA treated patients (p = 0.848). However, UDCA cystogenesis in a rat model of polycystic liver disease (PLD) inhibited LCV growth in ADPKD patients compared to ADPKD in vivo. Our aim was to test whether UDCA may beneficially affect controls (p = 0.049). liver volume in patients with advanced PLD. Conclusions: UDCA administration for 24 weeks did not reduce Methods: We conducted an international, multicenter, random- TLV in advanced PLD, but UDCA reduced LCV growth in ADPKD ized controlled trial in symptomatic PLD patients from three ter- patients. Future studies might explore whether ADPKD and tiary referral centers. Patients with PLD and total liver volume ADPLD patients respond differently to UDCA treatment. (TLV) P2500 ml were randomly assigned to UDCA treatment Lay summary: Current therapies for polycystic liver disease are (15–20 mg/kg/day) for 24 weeks, or to no treatment. -

Cadasil Pathogenesis, Clinical and Radiological Findings and Treatment
View and review Arq Neuropsiquiatr 2010;68(2):287-299 Cadasil Pathogenesis, clinical and radiological findings and treatment Charles André ABSTRACT Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is the most common genetic cause of ischemic strokes and a most important model for the study of subcortical vascular dementia. This unrelentlessly progressive disease affects many hundreds of families all over the world but is not well studied in Brazil. This manuscript reviews pathogenetic, clinical, radiological and therapeutic features of CADASIL. The causal mutations are now very well known, but the same can not be said about its intimate pathogenetic mechanisms. The variable clinical presentation should lead physicians to actively pursue the diagnosis in many settings and to more thouroughly investigate family history in first degree relatives. A rational approach to genetic testing is however needed. Treatment of CADASIL is still largely empiric. High- quality therapeutic studies involving medications and cognitive interventions are strongly needed in CADASIL. Key words: CADASIL, etiology, genetics, diagnosis, therapeutics. CADASIL: patogênese, achados clínicos e radiológicos e tratamento RESUMO CADASIL é a causa genética mais freqüente de infartos cerebrais e constitui modelo importante de estudo de demências vasculares subcorticais. De natureza inexoravelmente progressiva, afeta milhares de pessoas em todo o mundo. Sua importância é pouco reconhecida entre nós, o que nos levou à presente revisão dos principais aspectos patogenéticos, clínicos, neuroradiológicos e terapêuticos da doença. As mutações causais são hoje bem conhecidas, mas os mecanismos patogenéticos íntimos ainda permanecem misteriosos. A apresentação clínica variável deve fazer com que os médicos considerem o diagnóstico em vários contextos clínicos e investiguem de forma mais extensa que o usual a história familial deparentes de primeiro grau. -

Saethre-Chotzen Syndrome
Saethre-Chotzen syndrome Authors: Professor L. Clauser1 and Doctor M. Galié Creation Date: June 2002 Update: July 2004 Scientific Editor: Professor Raoul CM. Hennekam 1Department of craniomaxillofacial surgery, St. Anna Hospital and University, Corso Giovecca, 203, 44100 Ferrara, Italy. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Definition Prevalence Management including treatment Etiology Diagnostic methods Genetic counseling Antenatal diagnosis Unresolved questions References Abstract Saethre-Chotzen Syndrome (SCS) is an inherited craniosynostotic condition, with both premature fusion of cranial sutures (craniostenosis) and limb abnormalities. The most common clinical features, present in more than a third of patients, consist of coronal synostosis, brachycephaly, low frontal hairline, facial asymmetry, hypertelorism, broad halluces, and clinodactyly. The estimated birth incidence is 1/25,000 to 1/50,000 but because the phenotype can be very mild, the entity is likely to be underdiagnosed. SCS is inherited as an autosomal dominant trait with a high penetrance and variable expression. The TWIST gene located at chromosome 7p21-p22, is responsible for SCS and encodes a transcription factor regulating head mesenchyme cell development during cranial tube formation. Some patients with an overlapping SCS phenotype have mutations in the FGFR3 (fibroblast growth factor receptor 3) gene; especially the Pro250Arg mutation in FGFR3 (Muenke syndrome) can resemble SCS to a great extent. Significant intrafamilial -

Article Pansomatostatin Agonist Pasireotide Long-Acting Release
CJASN ePress. Published on August 25, 2020 as doi: 10.2215/CJN.13661119 Article Pansomatostatin Agonist Pasireotide Long-Acting Release for Patients with Autosomal Dominant Polycystic Kidney or Liver Disease with Severe Liver Involvement A Randomized Clinical Trial 1Division of Nephrology and 1 1 2 1 1 1 Marie C. Hogan , Julie A. Chamberlin, Lisa E. Vaughan, Angela L. Waits, Carly Banks, Kathleen Leistikow, Hypertension, Mayo Troy Oftsie,1 Chuck Madsen,1 Marie Edwards,1,3 James Glockner,4 Walter K. Kremers,2 Peter C. Harris,1 Clinic College of Nicholas F. LaRusso,5 Vicente E. Torres ,1 and Tatyana V. Masyuk5 Medicine, Rochester, Minnesota 2Division of Abstract Biomedical Statistics Background and objectives We assessed safety and efficacy of another somatostatin receptor analog, pasireotide and Informatics, Mayo long-acting release, in severe polycystic liver disease and autosomal dominant polycystic kidney disease. Clinic College of Pasireotide long-acting release, with its broader binding profile and higher affinity to known somatostatin Medicine, Rochester, fi Minnesota receptors, has potential for greater ef cacy. 3Biomedical Imaging Research Core Facility, Design, setting, participants, & measurements Individuals with severe polycystic liver disease were assigned in a PKD Translational 2:1 ratio in a 1-year, double-blind, randomized trial to receive pasireotide long-acting release or placebo. Primary Research Center, Mayo Clinic College of outcome was change in total liver volume; secondary outcomes were change in total kidney volume, eGFR, and Medicine, Rochester, quality of life. Minnesota 4Department of Results Of 48 subjects randomized, 41 completed total liver volume measurements (n529 pasireotide long-acting Radiology, Mayo release and n512 placebo). -

MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics
MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics University of Michigan Health Systems (734) 763-6767 1500 E. Medical Center Drive (734) 763-6561 (fax) D5240 MPB Ann Arbor, MI 48109-5718 Biochemical Genetics Goals and Objectives Director: Drs. Ayesha Ahmad and Shane C. Quinonez The goals and objectives of the Biochemical Genetics Clinic rotation in the Medical Genetics Residency Program are to provide the resident with exposure to all aspects of care of metabolic disease and counseling in accordance with the Residency Review Committee for Medical Genetics expectations and to fulfill criteria for board eligibility by the American Board of Medical Genetics. Patient Care The resident will become familiar with the evaluation, diagnosis and management of urea cycle disorders, organic acidemias, disorders of carbohydrate and lipid metabolism and numerous other inborn errors of metabolism (IEMs). Residents will gain exposure in performing and expertise in interpreting biochemical analyses relevant to the diagnosis and management of human genetic diseases. By the end of the rotation the resident should be able to identify signs and symptoms of IEMs, formulate a differential diagnosis, order appropriate tests and recognize normal variants and complex patterns of metabolites. Residents will be able to manage acute metabolic crises and provide chronic management of patients with an IEM. Residents should be able to interpret NBS results, collaborate with the primary provider to act upon results in a timely manner, develop a differential diagnosis and order appropriate confirmatory testing and communicate results to families. Medical Knowledge Through coursework and didactic sessions with attending physicians, residents will become familiar with fundamental concepts, molecular biology and biochemistry relevant to IEMs. -

Instelling Naam Expertise Centrum Cluster Van / Specifieke Aandoening Toelichting Erkenning
Instelling Naam Expertise Centrum Cluster van / Specifieke aandoening Toelichting erkenning AMC Amsterdam Lysosome Center Gaucher disease ("Sphinx") Fabry disease Niemann-Pick disease type A Niemann-Pick disease type B Niemann-Pick disease type C Mucopolysaccharidosis type 1 Mucopolysaccharidosis type 3 Mucopolysaccharidosis type 4 Lysosomal Disease Cholesteryl ester storage disease AMC Dutch Centre for Peroxisomal Peroxisome biogenesis disorder-Zellweger syndrome spectrum disorders Disorder of peroxisomal alpha- - beta- and omega-oxidation Rhizomelic chondrodysplasia punctata Non-syndromic pontocerebellar hypoplasia AMC Expertise center Vascular medicine Homozygous familial hypercholesterolemia Familial lipoprotein lipase deficiency Tangier disease AMC Centre for Genetic Metabolic Disorder of galactose metabolism Diseases Amsterdam Disorder of phenylalanine metabolism AMC Centre for Neuromuscular Diseases Neuromuscular disease Motor neuron disease; amyotrophic lateral sclerosis, primary sclerosis and progressive muscular atrophy Idiopathic inflammatory myopathy, incl dermatomyositis, polymyositis, necrotizing autoimmune myopathy and inclusion body myositis Poliomyelitis Hereditary motor and sensory neuropathy Chronic inflammatory demyelinating polyneuropathy, incl. Guillain_Barre syndrome, CIDP, MMN AMC Centre for rare thyroid diseases Congenital hypothyroidism AMC Centre for gastroenteropancreatic Gastroenteropancreatic endocrine tumor neuroendocrine tumors AMC Centre for rare hypothalamic and Rare hypothalamic or pituitary disease pituitary -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic