Clinical and Genetic Characterisation of Hereditary Motor Neuropathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

Blueprint Genetics Comprehensive Growth Disorders / Skeletal
Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel Test code: MA4301 Is a 374 gene panel that includes assessment of non-coding variants. This panel covers the majority of the genes listed in the Nosology 2015 (PMID: 26394607) and all genes in our Malformation category that cause growth retardation, short stature or skeletal dysplasia and is therefore a powerful diagnostic tool. It is ideal for patients suspected to have a syndromic or an isolated growth disorder or a skeletal dysplasia. About Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders This panel covers a broad spectrum of diseases associated with growth retardation, short stature or skeletal dysplasia. Many of these conditions have overlapping features which can make clinical diagnosis a challenge. Genetic diagnostics is therefore the most efficient way to subtype the diseases and enable individualized treatment and management decisions. Moreover, detection of causative mutations establishes the mode of inheritance in the family which is essential for informed genetic counseling. For additional information regarding the conditions tested on this panel, please refer to the National Organization for Rare Disorders and / or GeneReviews. Availability 4 weeks Gene Set Description Genes in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACAN# Spondyloepimetaphyseal dysplasia, aggrecan type, AD/AR 20 56 Spondyloepiphyseal dysplasia, Kimberley -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -
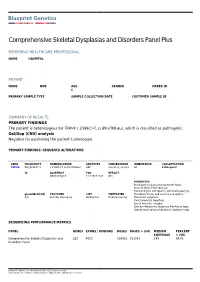
Report 99517
Comprehensive Skeletal Dysplasias and Disorders Panel Plus REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL PATIENT NAME DOB AGE GENDER ORDER ID 6 PRIMARY SAMPLE TYPE SAMPLE COLLECTION DATE CUSTOMER SAMPLE ID SUMMARY OF RESULTS PRIMARY FINDINGS The patient is heterozygous for TRPV4 c.2396C>T, p.(Pro799Leu), which is classified as pathogenic. Del/Dup (CNV) analysis Negative for explaining the patient’s phenotype. PRIMARY FINDINGS: SEQUENCE ALTERATIONS GENE TRANSCRIPT NOMENCLATURE GENOTYPE CONSEQUENCE INHERITANCE CLASSIFICATION TRPV4 NM_021625.4 c.2396C>T, p.(Pro799Leu) HET missense_variant AD Pathogenic ID ASSEMBLY POS REF/ALT GRCh37/hg19 12:110222183 G/A PHENOTYPE Brachyolmia (autosomal dominant type), Charcot-Marie-Tooth disease, Familial Digital arthropathy with brachydactyly, gnomAD AC/AN POLYPHEN SIFT MUTTASTER Hereditary motor and sensory neuropathy, 0/0 possibly damaging deleterious disease causing Metatropic dysplasia, Parastremmatic dwarfism, Spinal muscular atrophy, Spondyloepiphyseal dysplasia Maroteaux type, Spondylometaphyseal dysplasia Kozlowski type SEQUENCING PERFORMANCE METRICS PANEL GENES EXONS / REGIONS BASES BASES > 20X MEDIAN PERCENT COVERAGE > 20X Comprehensive Skeletal Dysplasias and 252 4053 816901 812241 199 99.43 Disorders Panel Blueprint Genetics Oy, Keilaranta 16 A-B, 02150 Espoo, Finland VAT number: FI22307900, CLIA ID Number: 99D2092375, CAP Number: 9257331 TARGET REGION AND GENE LIST The Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders Panel (version 4, Oct 19, 2019) Plus Analysis includes sequence -

Skeletal Dysplasias Precision Panel Overview Indications
Skeletal Dysplasias Precision Panel Overview Skeletal Dysplasias, also known as osteochondrodysplasias, are a clinically and phenotypically heterogeneous group of more than 450 inherited disorders characterized by abnormalities mainly of cartilage and bone growth although they can also affect muscle, tendons and ligaments, resulting in abnormal shape and size of the skeleton and disproportion of long bones, spine and head. They differ in natural histories, prognoses, inheritance patterns and physiopathologic mechanisms. They range in severity from those that are embryonically lethal to those with minimum morbidity. Approximately 5% of children with congenital birth defects have skeletal dysplasias. Until recently, the diagnosis of skeletal dysplasia relied almost exclusively on careful phenotyping, however, the advent of genomic tests has the potential to make a more accurate and definite diagnosis based on the suspected clinical diagnosis. The 4 most common skeletal dysplasias are thanatophoric dysplasia, achondroplasia, osteogenesis imperfecta and achondrogenesis. The inheritance pattern of skeletal dysplasias is variable and includes autosomal dominant, recessive and X-linked. The Igenomix Skeletal Dysplasias Precision Panel can be used to make a directed and accurate differential diagnosis of skeletal abnormalities ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum -

Whole Exome Sequencing Gene Package Skeletal Dysplasia, Version 2.1, 31-1-2020
Whole Exome Sequencing Gene package Skeletal Dysplasia, Version 2.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCC9 Atrial fibrillation, familial, 12, 614050 601439 65 100 100 95 Cardiomyopathy, dilated, 1O, 608569 Hypertrichotic osteochondrodysplasia, 239850 ACAN Short stature and advanced bone age, with or without early-onset osteoarthritis -

Download Sample Report
Sample report as of Nov 1st, 2020. Regional differences may apply. For complete and up-to-date test methodology description, please see your report in Nucleus online portal. Accreditation and certification information available at blueprintgenetics.com/certifications Comprehensive Skeletal Dysplasias and Disorders Panel Plus REFERRING HEALTHCARE PROFESSIONAL NAME HOSPITAL PATIENT NAME DOB AGE GENDER ORDER ID 6 PRIMARY SAMPLE TYPE SAMPLE COLLECTION DATE CUSTOMER SAMPLE ID SUMMARY OF RESULTS PRIMARY FINDINGS The patient is heterozygous for TRPV4 c.2396C>T, p.(Pro799Leu), which is classified as pathogenic. Del/Dup (CNV) analysis Negative for explaining the patient’s phenotype. PRIMARY FINDINGS: SEQUENCE ALTERATIONS GENE TRANSCRIPT NOMENCLATURE GENOTYPE CONSEQUENCE INHERITANCE CLASSIFICATION TRPV4 NM_021625.4 c.2396C>T, p.(Pro799Leu) HET missense_variant AD Pathogenic ID ASSEMBLY POS REF/ALT GRCh37/hg19 12:110222183 G/A PHENOTYPE Brachyolmia (autosomal dominant type), Charcot-Marie-Tooth disease, Familial Digital arthropathy with brachydactyly, gnomAD AC/AN POLYPHEN SIFT MUTTASTER Hereditary motor and sensory neuropathy, 0/0 possibly damaging deleterious disease causing Metatropic dysplasia, Parastremmatic dwarfism, Spinal muscular atrophy, Spondyloepiphyseal dysplasia Maroteaux type, Spondylometaphyseal dysplasia Kozlowski type SEQUENCING PERFORMANCE METRICS PANEL GENES EXONS / REGIONS BASES BASES > 20X MEDIAN PERCENT COVERAGE > 20X Comprehensive Skeletal Dysplasias and 252 4053 816901 812241 199 99.43 Disorders Panel Blueprint Genetics Oy, -

Joints Chapter 8
Chapter 8 Joints Alessandro Castriota-Scanderbeg, M.D. Joints develop secondarily in the mesenchyme com- Joint Contracture, Joint Stiffness prised between the developing ends of two adjacent bones (mesenchymal interpose) at about 5 1/2 weeks. ᭤ [Limitation (loss) of (active and passive) The mesenchyme is converted to form fibrous tissue, joint motion] hyaline cartilage, or fibrocartilage, depending on whether the developing joint is a fibrous joint, a syn- The issue discussed in the current section encom- chondrosis, or a symphysis, respectively.At the site of passes a heterogeneous group of conditions, both in- a synovial joint, while the primitive mesenchyme of herited and acquired, isolated and associated with the interzone undergoes liquefaction and cavitation, syndromic and nonsyndromic malformation spec- giving rise to the articular cavity, its peripheral con- tra, localized to one joint and generalized. An intro- densation results in formation of the joint capsule duction to the contractural abnormalities developing (Resnick et al.1995).This process is completed by ap- after birth is first provided, followed by a discussion proximately 7 weeks of fetal age, and by 8 weeks of the congenital forms, which represent the main fo- movements of the limbs about the joint are appear- cus of the section. ing. Motion is essential for the normal development Flexion contracture and joint stiffness may occur of joints and contiguous structures. As discussed in as late manifestations of conditions causing joint more detail in the following pages, congenital limita- and/or surrounding tissue infiltration (sarcoidosis, tion or loss of joint function may be caused by factors amyloidosis), hemorrhage (trauma, hemophilia), or that either are intrinsic to the joint, or are extrinsic inflammation (rheumatoid arthritis, systemic lupus but inhibit fetal movements. -
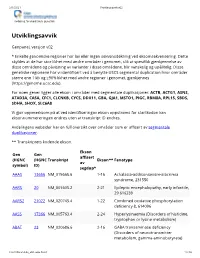
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Skeletal Dysplasia Panel Versie V2 (346 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, V2, in voege op 26/05/2020 Skeletal_dysplasia panel versie V2 (346 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Atrial fibrillation, familial, 12, 614050 (3), Autosomal dominant; ABCC9 601439 Cardiomyopathy, dilated, 1O, 608569 (3); Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant Congenital heart defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant; Leukemia, Philadelphia ABL1 189980 chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation Short stature and advanced bone age, with or without early-onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), ACAN 155760 Autosomal dominant; Spondyloepimetaphyseal dysplasia, aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, 607944 (3), ACP5 171640 Autosomal recessive ACVR1 102576 Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), Autosomal ADAMTS10 608990 recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), Autosomal ADAMTS17 607511 recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia punctata, -

Skeletal Dysplasia Panel Versie V3 (450 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, in voege op 02/06/2021 Skeletal_dysplasia panel versie v3 (450 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant; ?Atrial fibrillation, familial, 12, 614050 (3), ABCC9 601439 Autosomal dominant; Cardiomyopathy, dilated, 1O, 608569 (3), Autosomal dominant Leukemia, Philadelphia chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation; Congenital heart ABL1 189980 defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant Short stature and advanced bone age, with or without early- onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), Autosomal dominant; Spondyloepimetaphyseal dysplasia, ACAN 155760 aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, ACP5 171640 607944 (3), Autosomal recessive Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal ACVR1 102576 dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), ADAMTS10 608990 Autosomal recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), ADAMTS17 607511 Autosomal recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia -

CTGT Req Form 07302018.Pdf
Connective Tissue Gene Tests 6575 Snowdrift Road, Suite 106, Allentown, PA 18106 Phone: (484) 244-2900· Fax: (484) 244-2904 www.ctgt.net (CLIA # 39D1027912 · CAP# 7190738· NPI# 1891864997) LABORATORY TEST REQUISITION FORM 07302018 Please print clearly and provide all requested information. CTGT cannot initiate testing unless this information is provided. PATIENT / SPECIMEN INFORMATION PATIENT NAME – LAST, FIRST, MI M MRN DATE OF BIRTH (MM-DD-YYYY) F ADDRESS PHONE ETHNICITY CITY, STATE, ZIP NAME OF LEGAL GUARDIAN IF PATIENT IS A MINOR TYPE OF SPECIMEN DATE OF COLLECTION DATE AND TIME OF RECEIPT (TO BE COMPLETED BY CTGT) REPORTING INFORMATION REFERRAL SOURCE REFERRED BY NPI NUMBER GENETIC COUNSELOR INSTITUTION PHONE FAX ADDRESS E-MAIL CITY, STATE, ZIP SIGNATURE (REQUIRED – By signing, you agree to the Terms on page 10 of this form) ADDITIONAL REPORTS REFERRING LAB CONTACT PERSON ADDRESS PHONE FAX CITY, STATE, ZIP REFERRING LAB ID# PAYMENT INFORMATION INSTITUTIONAL BILLING FACILITY NAME CONTACT PERSON ADDRESS PHONE FAX CITY, STATE, ZIP E-MAIL SELF PAY (ALSO REQUIRED FOR ALL INSURANCE CASES – PLEASE SEE “INSURANCE” BELOW.) CHECK M.O. Please make check or money order payable to Connective Tissue Gene Tests. ACCOUNT NUMBER EXPIRATION DATE 3 DIGIT SECURITY CODE (on back of card) MC VISA The total cost of testing is $____________. I agree that Connective Tissue SIGNATURE OF CARDHOLDER (REQUIRED) Gene Tests, LLC. shall bill this amount to my credit card. INSURANCE - Important note to Patients: Connective Tissue Gene Tests (CTGT) does not participate with any health plan, and CANNOT guarantee that your plan will reimburse you or CTGT for our testing services.