Saethre-Chotzen Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hallux Valgus
MedicalContinuing Education Building Your FOOTWEAR PRACTICE Objectives 1) To be able to identify and evaluate the hallux abductovalgus deformity and associated pedal conditions 2) To know the current theory of etiology and pathomechanics of hallux valgus. 3) To know the results of recent Hallux Valgus empirical studies of the manage- ment of hallux valgus. Assessment and 4) To be aware of the role of conservative management, faulty footwear in the develop- ment of hallux valgus deformity. and the role of faulty footwear. 5) To know the pedorthic man- agement of hallux valgus and to be cognizant of the 10 rules for proper shoe fit. 6) To be familiar with all aspects of non-surgical management of hallux valgus and associated de- formities. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Continu- ing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $15 per topic) or 2) per year, for the special introductory rate of $99 (you save $51). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. In the near future, you may be able to submit via the Internet. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. -

Angular Limb Deformities in Foals: Treatment and Prognosis*
Article #4 CE Angular Limb Deformities in Foals: Treatment and Prognosis* Nicolai Jansson, DVM, PhD, DECVS Skara Equine Hospital Skara, Sweden Norm G. Ducharme, DVM, MSc, DACVS Cornell University ABSTRACT: This article presents an overview of the clinical management of foals with angular limb deformities. Both conservative and surgical treatment options exist; the choice of which to use should be based on the type, severity, and location of the deformity as well as the age of the foal. Conservative measures include controlled exercise, rigid external limb support, and corrective hoof trimming. Surgical treatment modalities comprise tech- niques for manipulating physeal growth and, after physeal closure, various corrective osteotomy or ostectomy methods. The prognosis is generally good if treatment is initi- ated well in advance of physeal closure. ngular limb deformities and their treat- Conservative Treatment ment in foals and young horses constitute In most foals born with mild to moderate a significant part of the orthopedic prob- angular deformities, spontaneous resolution A 2 lems that veterinarians must manage. This article occurs within the first 2 to 4 weeks of life. In discusses the clinical management and prognosis newborn foals, periarticular laxity is the most of these postural deformities. likely cause, and these foals require no special treatment other than a short period of con- TREATMENT trolled exercise. In our opinion, mildly and The absence of controlled studies has moderately affected foals should not be confined impaired the accumulation of scientific data to a stall because exercise is important for nor- guiding the management of angular limb defor- mal muscular development and resolution of the mities in foals (Table 1). -

MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics
MEDICAL GENETICS RESIDENCY PROGRAM Department of Pediatrics University of Michigan Health Systems (734) 763-6767 1500 E. Medical Center Drive (734) 763-6561 (fax) D5240 MPB Ann Arbor, MI 48109-5718 Biochemical Genetics Goals and Objectives Director: Drs. Ayesha Ahmad and Shane C. Quinonez The goals and objectives of the Biochemical Genetics Clinic rotation in the Medical Genetics Residency Program are to provide the resident with exposure to all aspects of care of metabolic disease and counseling in accordance with the Residency Review Committee for Medical Genetics expectations and to fulfill criteria for board eligibility by the American Board of Medical Genetics. Patient Care The resident will become familiar with the evaluation, diagnosis and management of urea cycle disorders, organic acidemias, disorders of carbohydrate and lipid metabolism and numerous other inborn errors of metabolism (IEMs). Residents will gain exposure in performing and expertise in interpreting biochemical analyses relevant to the diagnosis and management of human genetic diseases. By the end of the rotation the resident should be able to identify signs and symptoms of IEMs, formulate a differential diagnosis, order appropriate tests and recognize normal variants and complex patterns of metabolites. Residents will be able to manage acute metabolic crises and provide chronic management of patients with an IEM. Residents should be able to interpret NBS results, collaborate with the primary provider to act upon results in a timely manner, develop a differential diagnosis and order appropriate confirmatory testing and communicate results to families. Medical Knowledge Through coursework and didactic sessions with attending physicians, residents will become familiar with fundamental concepts, molecular biology and biochemistry relevant to IEMs. -

Conformational Limb Abnormalities and Corrective Farriery for Foals
Conformational Limb Abnormalities and Corrective Farriery for Foals For the past couple of years the general public has questioned the horse industry, and one of the questions is “Are we breeding horses more prone to breakdown with injuries”? It seems that we hear more often now that there are more leg and foot problems than ever before. Is it that we are more aware of conformational deficits and limb deviations, or are there some underlying factors that make our horses prone to injury? To improve, or even just maintain the breed, racing should prove soundness as well as speed and stamina. 1 The male side is usually removed from the bloodline if unable to produce good results at the racetrack. However, the female may have such poor conformation that she never even gets into training, but yet she enters the broodmare band. The generational effect of this must surely lead to an increase in the number of conformational deficits in our foals and yearlings.1 Something that we hear quite often is “Whoever saw the perfect horse”? and “There are plenty of horses with poor conformation that win races”. That doesn’t mean we should not continue to attempt to produce horses with good conformation. There is an acceptable range of deviation from the ideal, and therefore these deformities have to be accepted if it does not jeopardize the overall athletic soundness of the horse. Although mild conformational deficits may not significantly impact soundness, more significant limb deformities cause abnormal limb loading, lameness, gait abnormalities, and interference issues. 2 Developmental deformities of the limb include angular, flexural, and rotational limb deformities. -

Oral Surgery Procedures in a Patient with Hajdu-Cheney Syndrome Treated with Denosumab—A Rare Case Report
International Journal of Environmental Research and Public Health Article Oral Surgery Procedures in a Patient with Hajdu-Cheney Syndrome Treated with Denosumab—A Rare Case Report Magdalena Kaczoruk-Wieremczuk 1,†, Paulina Adamska 1,† , Łukasz Jan Adamski 1, Piotr Wychowa ´nski 2 , Barbara Alicja Jereczek-Fossa 3,4 and Anna Starzy ´nska 1,* 1 Department of Oral Surgery, Medical University of Gda´nsk,7 D˛ebinkiStreet, 80-211 Gda´nsk,Poland; [email protected] (M.K.-W.); [email protected] (P.A.); [email protected] (Ł.J.A.) 2 Department of Oral Surgery, Medical University of Warsaw, 6 St. Binieckiego Street, 02-097 Warsaw, Poland; [email protected] 3 Department of Oncology and Hemato-Oncology, University of Milan, 7 Festa del Perdono Street, 20-112 Milan, Italy; [email protected] 4 Division of Radiotherapy, IEO European Institute of Oncology, IRCCS, 435 Ripamonti Street, 20-141 Milan, Italy * Correspondence: [email protected] † Co-first author, these authors contributed equally to this work. Abstract: Background: Hajdu-Cheney syndrome (HCS) is a very rare autosomal-dominant congenital disease associated with mutations in the NOTCH2 gene. This disorder affects the connective tissue and is characterized by severe bone resorption. Hajdu-Cheney syndrome most frequently affects Citation: Kaczoruk-Wieremczuk, M.; the head and feet bones (acroosteolysis). Case report: We present an extremely rare case of a 34- Adamska, P.; Adamski, Ł.J.; Wychowa´nski,P.; Jereczek-Fossa, year-old male with Hajdu-Cheney syndrome. The patient was admitted to the Department of Oral B.A.; Starzy´nska,A. Oral Surgery Surgery, Medical University of Gda´nsk,in order to perform the extraction of three teeth. -
Peds Ortho: What Is Normal, What Is Not, and When to Refer
Peds Ortho: What is normal, what is not, and when to refer Future of Pedatrics June 10, 2015 Matthew E. Oetgen Benjamin D. Martin Division of Orthopaedic Surgery AGENDA • Definitions • Lower Extremity Deformity • Spinal Alignment • Back Pain LOWER EXTREMITY ALIGNMENT DEFINITIONS coxa = hip genu = knee cubitus = elbow pes = foot varus valgus “bow-legged” “knock-knee” apex away from midline apex toward midline normal varus hip (coxa vara) varus humerus valgus ankle valgus hip (coxa valga) Genu varum (bow-legged) Genu valgum (knock knee) bow legs and in toeing often together Normal Limb alignment NORMAL < 2 yo physiologic = reassurance, reevaluate @ 2 yo Bow legged 7° knock knee normal Knock knee physiologic = reassurance, reevaluate in future 4 yo abnormal 10 13 yo abnormal + pain 11 Follow-up is essential! 12 Intoeing 1. Femoral anteversion 2. Tibial torsion 3. Metatarsus adductus MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE! BRACES ARE HISTORY! Femoral Anteversion “W” sitters Internal rotation >> External rotation knee caps point in MOST LIKELY PHYSIOLOGIC AND MAY RESOLVE! Internal Tibial Torsion Thigh foot angle MOST LIKELY PHYSIOLOGIC AND WILL RESOLVE BY SCHOOL AGE Foot is rotated inward Internal Tibial Torsion (Fuchs 1996) Metatarsus Adductus • Flexible = correctible • Observe vs. casting CURVED LATERAL BORDER toes point in NOT TO BE CONFUSED WITH… Clubfoot talipes equinovarus adductus internal varus rotation equinus CAN’T DORSIFLEX cavus Clubfoot START19 CASTING JUST AFTER BIRTH Calcaneovalgus Foot • Intrauterine positioning • Resolve -

SKELETAL DYSPLASIA Dr Vasu Pai
SKELETAL DYSPLASIA Dr Vasu Pai Skeletal dysplasia are the result of a defective growth and development of the skeleton. Dysplastic conditions are suspected on the basis of abnormal stature, disproportion, dysmorphism, or deformity. Diagnosis requires Simple measurement of height and calculation of proportionality [<60 inches: consideration of dysplasia is appropriate] Dysmorphic features of the face, hands, feet or deformity A complete physical examination Radiographs: Extremities and spine, skull, Pelvis, Hand Genetics: the risk of the recurrence of the condition in the family; Family evaluation. Dwarf: Proportional: constitutional or endocrine or malnutrition Disproportion [Trunk: Extremity] a. Height < 42” Diastrophic Dwarfism < 48” Achondroplasia 52” Hypochondroplasia b. Trunk-extremity ratio May have a normal trunk and short limbs (achondroplasia), Short trunk and limbs of normal length (e.g., spondylo-epiphyseal dysplasia tarda) Long trunk and long limbs (e.g., Marfan’s syndrome). c. Limb-segment ratio Normal: Radius-Humerus ratio 75% Tibia-Femur 82% Rhizomelia [short proximal segments as in Achondroplastics] Mesomelia: Dynschondrosteosis] Acromelia [short hands and feet] RUBIN CLASSIFICATION 1. Hypoplastic epiphysis ACHONDROPLASTIC Autosomal Dominant: 80%; 0.5-1.5/10000 births Most common disproportionate dwarfism. Prenatal diagnosis: 18 weeks by measuring femoral and humeral lengths. Abnormal endochondral bone formation: zone of hypertrophy. Gene defect FGFR fibroblast growth factor receptor 3 . chromosome 4 Rhizomelic pattern, with the humerus and femur affected more than the distal extremities; Facies: Frontal bossing; Macrocephaly; Saddle nose Maxillary hypoplasia, Mandibular prognathism Spine: Lumbar lordosis and Thoracolumbar kyphosis Progressive genu varum and coxa valga Wedge shaped gaps between 3rd and 4th fingers (trident hands) Trident hand 50%, joint laxity Pathology Lack of columnation Bony plate from lack of growth Disorganized metaphysis Orthopaedics 1. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Arthrogryposis Multiplex Congenita Part 1: Clinical and Electromyographic Aspects
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.35.4.425 on 1 August 1972. Downloaded from Journal ofNeurology, Neurosurgery, anid Psychiatry, 1972, 35, 425-434 Arthrogryposis multiplex congenita Part 1: Clinical and electromyographic aspects E. P. BHARUCHA, S. S. PANDYA, AND DARAB K. DASTUR From the Children's Orthopaedic Hospital, and the Neuropathology Unit, J.J. Group of Hospitals, Bombay-8, India SUMMARY Sixteen cases with arthrogryposis multiplex congenita were examined clinically and electromyographically; three of them were re-examined later. Joint deformities were present in all extremities in 13 of the cases; in eight there was some degree of mental retardation. In two cases, there was clinical and electromyographic evidence of a myopathic disorder. In the majority, the appearances of the shoulder-neck region suggested a developmental defect. At the same time, selective weakness of muscles innervated by C5-C6 segments suggested a neuropathic disturbance. EMG revealed, in eight of 13 cases, clear evidence of denervation of muscles, but without any regenerative activity. The non-progressive nature of this disorder and capacity for improvement in muscle bulk and power suggest that denervation alone cannot explain the process. Re-examination of three patients after two to three years revealed persistence of the major deformities and muscle Protected by copyright. weakness noted earlier, with no appreciable deterioration. Otto (1841) appears to have been the first to ventricles, have been described (Adams, Denny- recognize this condition. Decades later, Magnus Brown, and Pearson, 1953; Fowler, 1959), in (1903) described it as multiple congenital con- addition to the spinal cord changes. -

Bilateral Both Bone Leg Fracture in a Case of Hereditary Multiple Exostoses with Bilateral Proximal and Distal Tibiofibular Synostosis
JMSCR Volume||2 ||Issue||5||Pages 1054-1058||May 2014 2014 www.jmscr.igmpublication.org Impact Factor-1.1147 ISSN (e)-2347-176x Bilateral Both Bone Leg Fracture in a Case of Hereditary Multiple Exostoses with Bilateral Proximal and Distal Tibiofibular Synostosis Authors Ganesh Singh1, Anshuman Vijay Roy2, Shailendra Singh Bhandari3, Pankaj Singh4 Author / Corresponding author Dr . Ganesh Singh M.S. (Orthopaedics) Assistant Professor , Department of Orthopaedics Room # 25 , New Resident Hostel , Medical Campus Government Medical College , Haldwani ( Uttarakhand ) . PIN -263139 Mobile no – 91-9319616456 , E mail – [email protected] Co –Authors Dr . Anshuman Vijay Roy M.S. (Orthopaedics ) Assistant Professor , Department of Orthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9927973777 E mail - [email protected] Dr Shailendra Singh Bhandari M.S.(Orthopaedics) Associatet Professor , Department of Orthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9837251168 E mail – [email protected] Dr . Pankaj Singh M.S. (Orthopaedics ) Professor , Department ofOrthopaedics Government Medical College , Haldwani ( Uttarakhand ). PIN – 263139 Mobile no. – 91-9927973777 E mail – [email protected] Ganesh Singh et al JMSCR Volume 2 Issue 5 May 2014 Page 1054 JMSCR Volume||2 ||Issue||5||Pages 1054-1058||May 2014 2014 Abstract The Hereditary Multiple Exostoses ( HME) is a neoplastic disorder affecting multiple skeletal sites in the form of bony protuberances of varying sizes and shapes . The clinical features are site specific and mostly relate to the effect of swelling on the adjacent tissues . Associated abnormalities like bowing deformities of bones, shortening and mechanical axes deviations may lead to increased risk of stresses over the bones . -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface. -
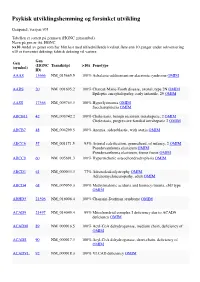
Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD