Hallux Valgus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ankylosing Spondylitis
Page 1 of 4 Ankylosing Spondylitis Ankylosing spondylitis (AS) is a form of arthritis. It mainly affects the lower back. Other joints and other parts of the body are sometimes affected. Treatment includes regular exercise and anti-inflammatory drugs. The severity of AS varies from mild to severe. It is mild or moderate in most cases. What is ankylosing spondylitis? Spondylitis means inflammation of the spine. Ankylosing is a word that describes bones that tend to join together (fuse) across a joint. In ankylosing spondylitis (AS), the discs and ligaments of the lower spine become inflamed. The discs and ligaments are the strong tissues that connect the spinal bones (vertebrae) together. The joints between the lower spine and the pelvis (the sacro-iliac joints), and the small facet joints between the vertebrae are also commonly affected. Inflammation around the lower spine that persists long-term can cause scarring. This may, over time, cause some of the vertebrae in the spine to fuse together. In some cases, inflammation occurs in other joints and in other parts of the body outside of the spine (detailed below). Who gets ankylosing spondylitis? AS usually develops in teenagers or young adults. It rarely first develops after the age of 40. It is three times more common in men than women. There may be a family history with two or more members of a family being affected. About 1 in 1000 people in the UK have AS. What causes ankylosing spondylitis? The cause of AS is not known. There is a strong genetic (hereditary) part. Something may 'trigger' AS to develop in people who have an inherited tendency to have it. -
Bunion Basics
WHAT IS A BUNION? A bunion is a “bump” on the outer edge of your big toe and forms when the bone or tissue at the big toe joint moves out of place. You may have a bunion if this area of your foot is red, swollen, or painful. BUNION BASICS WHY DO I HAVE A BUNION? Blame your genetics first, but your footwear next! Bunions tend to run in families, specifically among those who have the foot type prone to developing a bunion. If you have flat feet, low arches, arthritis, or inflammatory joint disease, you can develop a bunion. Footwear choices play a role too! Wearing shoes that are too tight or cause the toes to be squeezed together, like many stylish peep-or pointed-toe shoes, aggravates a bunion-prone foot. WHAT CAN I DO ABOUT MY BUNION? If you’ve noticed the beginnings of a bunion, avoid high heels over two inches with tight toe-boxes. You can also use a bunion pad inside of your shoes to provide some protection. WHO CAN HELP WITH MY BUNION? Today’s podiatrist is the bunion expert and can help you Beat Bunion Blues! There are several treatment options available, including the following: – Padding and taping to minimize pain and keep the foot in a normal position, reducing stress and pain. – Anti-inflammatory medications and cortisone injections can be prescribed to ease acute pain and inflammation. – Physical therapy can relieve bunion pain, and ultrasound therapy is a technique for treating bunions and their associated soft tissue involvement. – Orthotics or shoe inserts may be useful in controlling foot function to prevent worsening of a bunion. -

Clinical and Radiographic Features of Spondylitic Hip Disease J
Ann Rheum Dis: first published as 10.1136/ard.38.4.332 on 1 August 1979. Downloaded from Annals of the Rheumatic Diseases, 1979, 38, 332-336 Clinical and radiographic features of spondylitic hip disease J. S. MARKS AND K. HARDINGE From the Rheumatology Unit and the Centre for Hip Surgery, Wrightington Hospital, Wigan, Lancs SUMMARY The clinical and radiographic features of hip disease in 76 patients with definite anky- losing spondylitis have been studied. Symptomatic hip involvement occurred late in the course of the disease, with a mean delay after the onset of 12 years in males and 7 years in females. Patients with disease onset before the age of 20 developed hip symptoms at an earlier stage. Associated diseases included uveitis (13 %), colitis (4 %), and psoriasis (4 %). Bilateral concentric loss of hip joint space with a relatively undeformed femoral head was the commonest radiological change (61 %). Localised loss ofjoint space at the upper pole (16 %) was associated with femoral head destruction and a greater degree of osteophytosis, suggesting coincidental or secondary osteoarthrosis. Bony ankylosis of the hips (10%) was present only in women, and the absence of osteophytes, cysts, and bone lesions of the iliac crests and ischial rami suggests that it is a distinct radiographic manifestation of female ankylosing spondylitis. copyright. Ankylosing spondylitis characteristically affects Clinical details obtained from the medical records the sacroiliac joints and the spine, but peripheral included age at onset of disease, site(s) of initial joint involvement occurs in at least 50% of patients symptoms, age at initial hip symptoms, associated during the course of their disease (Polley and diseases, previous medical and surgical treatment, Slocumb, 1947; Wilkinson and Bywaters, 1958; and details of hip surgery during admission. -

Adult Still's Disease
44 y/o male who reports severe knee pain with daily fevers and rash. High ESR, CRP add negative RF and ANA on labs. Edward Gillis, DO ? Adult Still’s Disease Frontal view of the hands shows severe radiocarpal and intercarpal joint space narrowing without significant bony productive changes. Joint space narrowing also present at the CMC, MCP and PIP joint spaces. Diffuse osteopenia is also evident. Spot views of the hands after Tc99m-MDP injection correlate with radiographs, showing significantly increased radiotracer uptake in the wrists, CMC, PIP, and to a lesser extent, the DIP joints bilaterally. Tc99m-MDP bone scan shows increased uptake in the right greater than left shoulders, as well as bilaterally symmetric increased radiotracer uptake in the elbows, hands, knees, ankles, and first MTP joints. Note the absence of radiotracer uptake in the hips. Patient had bilateral total hip arthroplasties. Not clearly evident are bilateral shoulder hemiarthroplasties. The increased periprosthetic uptake could signify prosthesis loosening. Adult Stills Disease Imaging Features • Radiographs – Distinctive pattern of diffuse radiocarpal, intercarpal, and carpometacarpal joint space narrowing without productive bony changes. Osseous ankylosis in the wrists common late in the disease. – Joint space narrowing is uniform – May see bony erosions. • Tc99m-MDP Bone Scan – Bilaterally symmetric increased uptake in the small and large joints of the axial and appendicular skeleton. Adult Still’s Disease General Features • Rare systemic inflammatory disease of unknown etiology • 75% have onset between 16 and 35 years • No gender, race, or ethnic predominance • Considered adult continuum of JIA • Triad of high spiking daily fevers with a skin rash and polyarthralgia • Prodromal sore throat is common • Negative RF and ANA Adult Still’s Disease General Features • Most commonly involved joint is the knee • Wrist involved in 74% of cases • In the hands, interphalangeal joints are more commonly affected than the MCP joints. -

Saethre-Chotzen Syndrome
Saethre-Chotzen syndrome Authors: Professor L. Clauser1 and Doctor M. Galié Creation Date: June 2002 Update: July 2004 Scientific Editor: Professor Raoul CM. Hennekam 1Department of craniomaxillofacial surgery, St. Anna Hospital and University, Corso Giovecca, 203, 44100 Ferrara, Italy. [email protected] Abstract Keywords Disease name and synonyms Excluded diseases Definition Prevalence Management including treatment Etiology Diagnostic methods Genetic counseling Antenatal diagnosis Unresolved questions References Abstract Saethre-Chotzen Syndrome (SCS) is an inherited craniosynostotic condition, with both premature fusion of cranial sutures (craniostenosis) and limb abnormalities. The most common clinical features, present in more than a third of patients, consist of coronal synostosis, brachycephaly, low frontal hairline, facial asymmetry, hypertelorism, broad halluces, and clinodactyly. The estimated birth incidence is 1/25,000 to 1/50,000 but because the phenotype can be very mild, the entity is likely to be underdiagnosed. SCS is inherited as an autosomal dominant trait with a high penetrance and variable expression. The TWIST gene located at chromosome 7p21-p22, is responsible for SCS and encodes a transcription factor regulating head mesenchyme cell development during cranial tube formation. Some patients with an overlapping SCS phenotype have mutations in the FGFR3 (fibroblast growth factor receptor 3) gene; especially the Pro250Arg mutation in FGFR3 (Muenke syndrome) can resemble SCS to a great extent. Significant intrafamilial -

Arthritis in Myasthenia Gravis
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.38.11.1048 on 1 November 1975. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1975, 38, 1048-1055 Arthritis in myasthenia gravis J. A. AARLI1, E.-J. MILDE, AND S. THUNOLD From the Departments of Neurology and Pathology, School of Medicine, University of Bergen, and the Rheumatic Disease Unit, The Deaconesses' Hospital, Bergen, Norway SYNOPSIS Seven patients with myasthenia gravis developed clinical signs of arthropathy. In two patients, the symptoms were due to a deforming rheumatoid arthritis and the myasthenic symptoms appeared as a transitory phase during the course of the disease. Muscle antibodies of IgG class were demonstrated with sera from both patients. Autoreactivity between muscle antibodies and rheuma- toid factor was detected in one patient. Both patients died from sudden cardiac failure. Necropsy was performed in one and revealed a spotty myocardial necrosis. One patient had juvenile rheumatoid arthritis. Two patients had mild articular symptoms with indices of multivisceral disease and sero- logical findings indicating a systemic lupus erythematosus. One patient had classical ankylosing spondylitis, and one, unspecified arthropathy. guest. Protected by copyright. The concept of myasthenia gravis as a pure cate a clinical overlap (Oosterhuis and de Haas, disorder of the neuromuscular transmission has 1968). The aim of the present paper is a re- probably been an obstacle to the full delineation appraisal ofthe relationship between myasthenia of the clinical picture of this disease. Thus, care- gravis and arthritis. Seven patients are described ful clinical examination has revealed a series of and the data compared with relevant literature. -

Angular Limb Deformities in Foals: Treatment and Prognosis*
Article #4 CE Angular Limb Deformities in Foals: Treatment and Prognosis* Nicolai Jansson, DVM, PhD, DECVS Skara Equine Hospital Skara, Sweden Norm G. Ducharme, DVM, MSc, DACVS Cornell University ABSTRACT: This article presents an overview of the clinical management of foals with angular limb deformities. Both conservative and surgical treatment options exist; the choice of which to use should be based on the type, severity, and location of the deformity as well as the age of the foal. Conservative measures include controlled exercise, rigid external limb support, and corrective hoof trimming. Surgical treatment modalities comprise tech- niques for manipulating physeal growth and, after physeal closure, various corrective osteotomy or ostectomy methods. The prognosis is generally good if treatment is initi- ated well in advance of physeal closure. ngular limb deformities and their treat- Conservative Treatment ment in foals and young horses constitute In most foals born with mild to moderate a significant part of the orthopedic prob- angular deformities, spontaneous resolution A 2 lems that veterinarians must manage. This article occurs within the first 2 to 4 weeks of life. In discusses the clinical management and prognosis newborn foals, periarticular laxity is the most of these postural deformities. likely cause, and these foals require no special treatment other than a short period of con- TREATMENT trolled exercise. In our opinion, mildly and The absence of controlled studies has moderately affected foals should not be confined impaired the accumulation of scientific data to a stall because exercise is important for nor- guiding the management of angular limb defor- mal muscular development and resolution of the mities in foals (Table 1). -

Bunion Surgery - Orthoinfo - AAOS 6/10/12 3:20 PM
Bunion Surgery - OrthoInfo - AAOS 6/10/12 3:20 PM Copyright 2001 American Academy of Orthopaedic Surgeons Bunion Surgery Most bunions can be treated without surgery. But when nonsurgical treatments are not enough, surgery can relieve your pain, correct any related foot deformity, and help you resume your normal activities. An orthopaedic surgeon can help you decide if surgery is the best option for you. Whether you've just begun exploring treatment for bunions or have already decided with your orthopaedic surgeon to have surgery, this booklet will help you understand more about this valuable procedure. What Is A Bunion? A bunion is one problem that can develop due to hallux valgus, a foot deformity. The term "hallux valgus" is Latin and means a turning outward (valgus) of the big toe (hallux). The bone which joins the big toe, the first metatarsal, becomes prominent on the inner border of the foot. This bump is the bunion and is made up of bone and soft tissue. What Causes Bunions? By far the most common cause of bunions is the prolonged wearing of poorly fitting shoes, usually shoes with a narrow, pointed toe box that squeezes the toes into an unnatural position. Bunions also may be caused by arthritis or polio. Heredity often plays a role in bunion formation. But these causes account for only a small percentage of bunions. A study by the American Orthopaedic Foot and Ankle Society found that 88 percent of women in the U.S. wear shoes that are too small and 55 percent have bunions. Not surprisingly, bunions are nine times more common in women than men. -
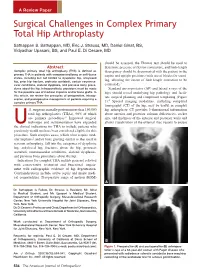
Surgical Challenges in Complex Primary Total Hip Arthroplasty
A Review Paper Surgical Challenges in Complex Primary Total Hip Arthroplasty Sathappan S. Sathappan, MD, Eric J. Strauss, MD, Daniel Ginat, BS, Vidyadhar Upasani, BS, and Paul E. Di Cesare, MD should be assessed, the Thomas test should be used to Abstract determine presence of flexion contracture, and limb-length Complex primary total hip arthroplasty (THA) is defined as discrepancy should be documented with the patient in the primary THA in patients with compromised bony or soft-tissue supine and upright positions (with use of blocks for stand- states, including but not limited to dysplastic hip, ankylosed hip, prior hip fracture, protrusio acetabuli, certain neuromus- ing, allowing the extent of limb-length correction to be 3 cular conditions, skeletal dysplasia, and previous bony proce- estimated). dures about the hip. Intraoperatively, provisions must be made Standard anteroposterior (AP) and lateral x-rays of the for the possible use of modular implants and/or bone grafts. In hips should reveal underlying hip pathology and facili- this article, we review the principles of preoperative, intraop- tate surgical planning and component templating (Figure erative, and postoperative management of patients requiring a 4 complex primary THA. 1). Special imaging modalities, including computed tomography (CT) of the hip, may be useful in complex .S. surgeons annually perform more than 150,000 hip arthroplasty. CT provides 3-dimensional information total hip arthroplasties (THAs), 90% of which about anterior and posterior column deficiencies, socket are primary procedures.1 Improved surgical size, and thickness of the anterior and posterior walls and technique and instrumentation have expanded allows visualization of the external iliac vessels to ensure Uthe clinical indications for THA to include patients who previously would not have been considered eligible for this procedure. -

Conformational Limb Abnormalities and Corrective Farriery for Foals
Conformational Limb Abnormalities and Corrective Farriery for Foals For the past couple of years the general public has questioned the horse industry, and one of the questions is “Are we breeding horses more prone to breakdown with injuries”? It seems that we hear more often now that there are more leg and foot problems than ever before. Is it that we are more aware of conformational deficits and limb deviations, or are there some underlying factors that make our horses prone to injury? To improve, or even just maintain the breed, racing should prove soundness as well as speed and stamina. 1 The male side is usually removed from the bloodline if unable to produce good results at the racetrack. However, the female may have such poor conformation that she never even gets into training, but yet she enters the broodmare band. The generational effect of this must surely lead to an increase in the number of conformational deficits in our foals and yearlings.1 Something that we hear quite often is “Whoever saw the perfect horse”? and “There are plenty of horses with poor conformation that win races”. That doesn’t mean we should not continue to attempt to produce horses with good conformation. There is an acceptable range of deviation from the ideal, and therefore these deformities have to be accepted if it does not jeopardize the overall athletic soundness of the horse. Although mild conformational deficits may not significantly impact soundness, more significant limb deformities cause abnormal limb loading, lameness, gait abnormalities, and interference issues. 2 Developmental deformities of the limb include angular, flexural, and rotational limb deformities. -

Observed Changes in Radiographic Measurements of The
The Journal of Foot & Ankle Surgery xxx (2014) 1–4 Contents lists available at ScienceDirect The Journal of Foot & Ankle Surgery journal homepage: www.jfas.org Original Research Observed Changes in Radiographic Measurements of the First Ray after Frontal and Transverse Plane Rotation of the Hallux: Does the Hallux Drive the Metatarsal in a Bunion Deformity? Paul Dayton, DPM, MS, FACFAS 1, Mindi Feilmeier, DPM, FACFAS 2, Merrell Kauwe, BS 3, Colby Holmes, BS 3, Austin McArdle, BS 3, Nathan Coleman, DPM 4 1 Foot and Ankle Division, UnityPoint Clinic, and Adjunct Professor, Des Moines University College of Podiatric Medicine and Surgery, Fort Dodge, IA 2 Assistant Professor, Des Moines University College of Podiatric Medicine and Surgery, Fort Dodge, IA 3 Podiatric Medical Student, Des Moines University College of Podiatric Medicine and Surgery, Des Moines, IA 4 Second Year Resident, Podiatric Medicine and Surgery Residency, Foot and Ankle Division, UnityPoint Health, Fort Dodge, IA article info abstract Level of Clinical Evidence: 5 It is well known that the pathologic positions of the hallux and the first metatarsal in a bunion deformity are multiplanar. It is not universally understood whether the pathologic changes in the hallux or first metatarsal Keywords: etiology drive the deformity. We have observed that frontal plane rotation of the hallux can result in concurrent po- fi fresh frozen cadaver sitional changes proximally in the rst metatarsal in hallux abducto valgus. In the present study, we observed hallux abducto valgus the changes in common radiographic measurements used to evaluate a bunion deformity in 5 fresh frozen metatarsus primus adducto valgus cadaveric limbs. -

Arthrogryposis Multiplex Congenita Part 1: Clinical and Electromyographic Aspects
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.35.4.425 on 1 August 1972. Downloaded from Journal ofNeurology, Neurosurgery, anid Psychiatry, 1972, 35, 425-434 Arthrogryposis multiplex congenita Part 1: Clinical and electromyographic aspects E. P. BHARUCHA, S. S. PANDYA, AND DARAB K. DASTUR From the Children's Orthopaedic Hospital, and the Neuropathology Unit, J.J. Group of Hospitals, Bombay-8, India SUMMARY Sixteen cases with arthrogryposis multiplex congenita were examined clinically and electromyographically; three of them were re-examined later. Joint deformities were present in all extremities in 13 of the cases; in eight there was some degree of mental retardation. In two cases, there was clinical and electromyographic evidence of a myopathic disorder. In the majority, the appearances of the shoulder-neck region suggested a developmental defect. At the same time, selective weakness of muscles innervated by C5-C6 segments suggested a neuropathic disturbance. EMG revealed, in eight of 13 cases, clear evidence of denervation of muscles, but without any regenerative activity. The non-progressive nature of this disorder and capacity for improvement in muscle bulk and power suggest that denervation alone cannot explain the process. Re-examination of three patients after two to three years revealed persistence of the major deformities and muscle Protected by copyright. weakness noted earlier, with no appreciable deterioration. Otto (1841) appears to have been the first to ventricles, have been described (Adams, Denny- recognize this condition. Decades later, Magnus Brown, and Pearson, 1953; Fowler, 1959), in (1903) described it as multiple congenital con- addition to the spinal cord changes.