Ankylosing Spondylitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical and Radiographic Features of Spondylitic Hip Disease J
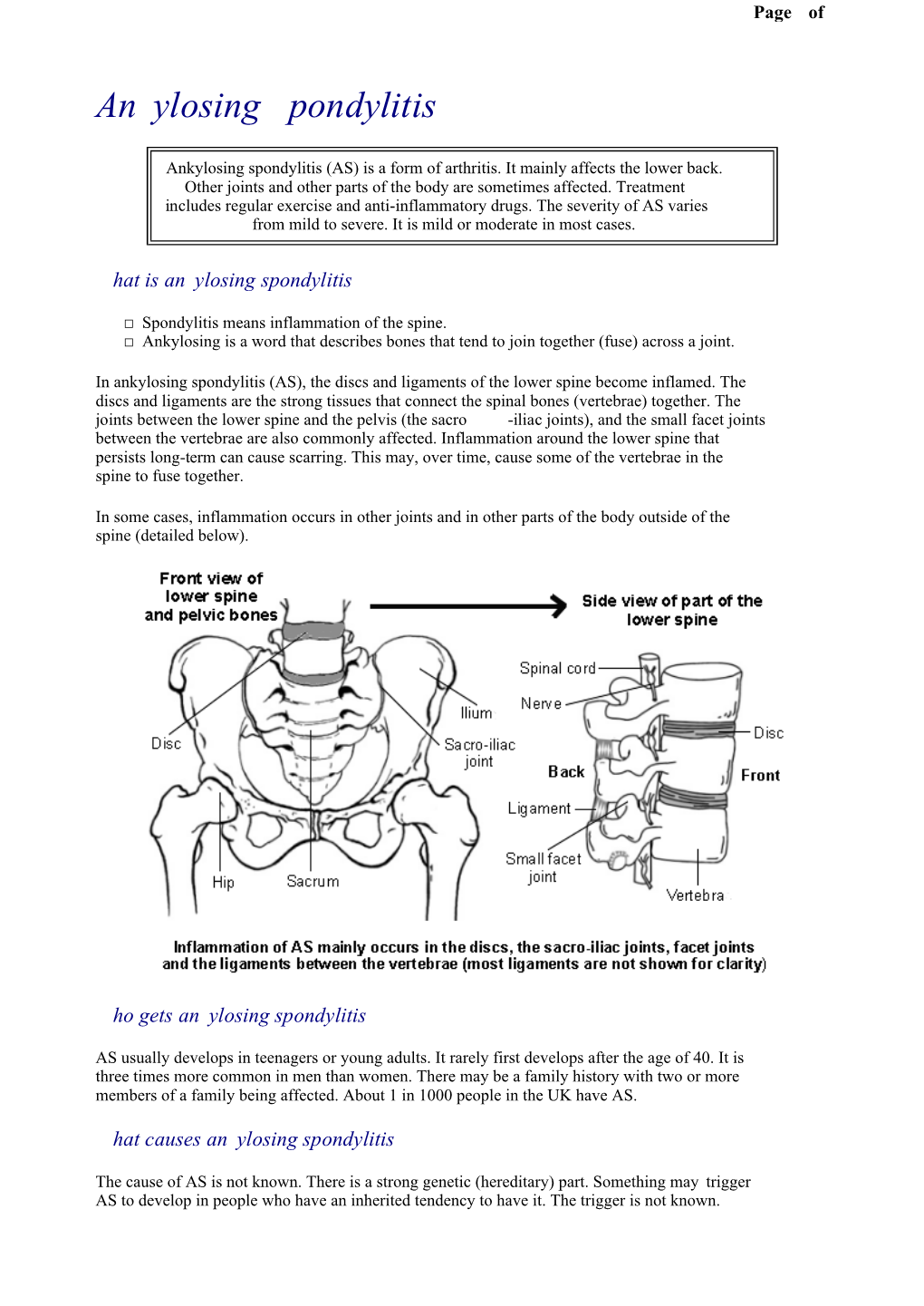
Ann Rheum Dis: first published as 10.1136/ard.38.4.332 on 1 August 1979. Downloaded from Annals of the Rheumatic Diseases, 1979, 38, 332-336 Clinical and radiographic features of spondylitic hip disease J. S. MARKS AND K. HARDINGE From the Rheumatology Unit and the Centre for Hip Surgery, Wrightington Hospital, Wigan, Lancs SUMMARY The clinical and radiographic features of hip disease in 76 patients with definite anky- losing spondylitis have been studied. Symptomatic hip involvement occurred late in the course of the disease, with a mean delay after the onset of 12 years in males and 7 years in females. Patients with disease onset before the age of 20 developed hip symptoms at an earlier stage. Associated diseases included uveitis (13 %), colitis (4 %), and psoriasis (4 %). Bilateral concentric loss of hip joint space with a relatively undeformed femoral head was the commonest radiological change (61 %). Localised loss ofjoint space at the upper pole (16 %) was associated with femoral head destruction and a greater degree of osteophytosis, suggesting coincidental or secondary osteoarthrosis. Bony ankylosis of the hips (10%) was present only in women, and the absence of osteophytes, cysts, and bone lesions of the iliac crests and ischial rami suggests that it is a distinct radiographic manifestation of female ankylosing spondylitis. copyright. Ankylosing spondylitis characteristically affects Clinical details obtained from the medical records the sacroiliac joints and the spine, but peripheral included age at onset of disease, site(s) of initial joint involvement occurs in at least 50% of patients symptoms, age at initial hip symptoms, associated during the course of their disease (Polley and diseases, previous medical and surgical treatment, Slocumb, 1947; Wilkinson and Bywaters, 1958; and details of hip surgery during admission. -

Hallux Valgus
MedicalContinuing Education Building Your FOOTWEAR PRACTICE Objectives 1) To be able to identify and evaluate the hallux abductovalgus deformity and associated pedal conditions 2) To know the current theory of etiology and pathomechanics of hallux valgus. 3) To know the results of recent Hallux Valgus empirical studies of the manage- ment of hallux valgus. Assessment and 4) To be aware of the role of conservative management, faulty footwear in the develop- ment of hallux valgus deformity. and the role of faulty footwear. 5) To know the pedorthic man- agement of hallux valgus and to be cognizant of the 10 rules for proper shoe fit. 6) To be familiar with all aspects of non-surgical management of hallux valgus and associated de- formities. Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Continu- ing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $15 per topic) or 2) per year, for the special introductory rate of $99 (you save $51). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. In the near future, you may be able to submit via the Internet. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned credits. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. -

Adult Still's Disease
44 y/o male who reports severe knee pain with daily fevers and rash. High ESR, CRP add negative RF and ANA on labs. Edward Gillis, DO ? Adult Still’s Disease Frontal view of the hands shows severe radiocarpal and intercarpal joint space narrowing without significant bony productive changes. Joint space narrowing also present at the CMC, MCP and PIP joint spaces. Diffuse osteopenia is also evident. Spot views of the hands after Tc99m-MDP injection correlate with radiographs, showing significantly increased radiotracer uptake in the wrists, CMC, PIP, and to a lesser extent, the DIP joints bilaterally. Tc99m-MDP bone scan shows increased uptake in the right greater than left shoulders, as well as bilaterally symmetric increased radiotracer uptake in the elbows, hands, knees, ankles, and first MTP joints. Note the absence of radiotracer uptake in the hips. Patient had bilateral total hip arthroplasties. Not clearly evident are bilateral shoulder hemiarthroplasties. The increased periprosthetic uptake could signify prosthesis loosening. Adult Stills Disease Imaging Features • Radiographs – Distinctive pattern of diffuse radiocarpal, intercarpal, and carpometacarpal joint space narrowing without productive bony changes. Osseous ankylosis in the wrists common late in the disease. – Joint space narrowing is uniform – May see bony erosions. • Tc99m-MDP Bone Scan – Bilaterally symmetric increased uptake in the small and large joints of the axial and appendicular skeleton. Adult Still’s Disease General Features • Rare systemic inflammatory disease of unknown etiology • 75% have onset between 16 and 35 years • No gender, race, or ethnic predominance • Considered adult continuum of JIA • Triad of high spiking daily fevers with a skin rash and polyarthralgia • Prodromal sore throat is common • Negative RF and ANA Adult Still’s Disease General Features • Most commonly involved joint is the knee • Wrist involved in 74% of cases • In the hands, interphalangeal joints are more commonly affected than the MCP joints. -

Arthritis in Myasthenia Gravis
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.38.11.1048 on 1 November 1975. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1975, 38, 1048-1055 Arthritis in myasthenia gravis J. A. AARLI1, E.-J. MILDE, AND S. THUNOLD From the Departments of Neurology and Pathology, School of Medicine, University of Bergen, and the Rheumatic Disease Unit, The Deaconesses' Hospital, Bergen, Norway SYNOPSIS Seven patients with myasthenia gravis developed clinical signs of arthropathy. In two patients, the symptoms were due to a deforming rheumatoid arthritis and the myasthenic symptoms appeared as a transitory phase during the course of the disease. Muscle antibodies of IgG class were demonstrated with sera from both patients. Autoreactivity between muscle antibodies and rheuma- toid factor was detected in one patient. Both patients died from sudden cardiac failure. Necropsy was performed in one and revealed a spotty myocardial necrosis. One patient had juvenile rheumatoid arthritis. Two patients had mild articular symptoms with indices of multivisceral disease and sero- logical findings indicating a systemic lupus erythematosus. One patient had classical ankylosing spondylitis, and one, unspecified arthropathy. guest. Protected by copyright. The concept of myasthenia gravis as a pure cate a clinical overlap (Oosterhuis and de Haas, disorder of the neuromuscular transmission has 1968). The aim of the present paper is a re- probably been an obstacle to the full delineation appraisal ofthe relationship between myasthenia of the clinical picture of this disease. Thus, care- gravis and arthritis. Seven patients are described ful clinical examination has revealed a series of and the data compared with relevant literature. -
Surgical Challenges in Complex Primary Total Hip Arthroplasty
A Review Paper Surgical Challenges in Complex Primary Total Hip Arthroplasty Sathappan S. Sathappan, MD, Eric J. Strauss, MD, Daniel Ginat, BS, Vidyadhar Upasani, BS, and Paul E. Di Cesare, MD should be assessed, the Thomas test should be used to Abstract determine presence of flexion contracture, and limb-length Complex primary total hip arthroplasty (THA) is defined as discrepancy should be documented with the patient in the primary THA in patients with compromised bony or soft-tissue supine and upright positions (with use of blocks for stand- states, including but not limited to dysplastic hip, ankylosed hip, prior hip fracture, protrusio acetabuli, certain neuromus- ing, allowing the extent of limb-length correction to be 3 cular conditions, skeletal dysplasia, and previous bony proce- estimated). dures about the hip. Intraoperatively, provisions must be made Standard anteroposterior (AP) and lateral x-rays of the for the possible use of modular implants and/or bone grafts. In hips should reveal underlying hip pathology and facili- this article, we review the principles of preoperative, intraop- tate surgical planning and component templating (Figure erative, and postoperative management of patients requiring a 4 complex primary THA. 1). Special imaging modalities, including computed tomography (CT) of the hip, may be useful in complex .S. surgeons annually perform more than 150,000 hip arthroplasty. CT provides 3-dimensional information total hip arthroplasties (THAs), 90% of which about anterior and posterior column deficiencies, socket are primary procedures.1 Improved surgical size, and thickness of the anterior and posterior walls and technique and instrumentation have expanded allows visualization of the external iliac vessels to ensure Uthe clinical indications for THA to include patients who previously would not have been considered eligible for this procedure. -

The Role of Arthroscopic Adhesiolysis in the Treatment of the Arthrofibrosis and the Partial Ankylosis of the Knee
Acta Orthop Traumatol Turc 28, 379-383 , 1994 The role of arthroscopic adhesiolysis in the treatment of the arthrofibrosis and the partial ankylosis of the knee Metin Lütfü Saydartl), Ethem Gür1l ), Vecihi Kırdemir1 l ), Ali Saib Engin(1) Dizin parsiyel ankilozu ve artrofibrozisinin tedavisinde artroskopik adezyolizisin rolü Travma, klf/k yada distal femur cerrahi girişim ardından gelişen diz hareketi kısıtlanan 23 hastanın 27 dizi, artroskopik kontrol altında , perkutan adezyon releasei ile tedavi edildi. Diz hareketlerini kısıtlayan neden ile artroskopik adezyolizis arasındaki dönem 4 ile 24 ay (ortalama 7 ay) arasında değişiyordu. Ortalama preope ratif diz hareketi 43°, ortalama postop diz hareketi IIS°'ydi. Ortalama postoperatif hareket kaybı 17"'ydi. Takip sonunda ortalama hareket kazancı SS°'ydi. Anahtar kelimeler: Artroskopi, artrofibrozis, adezyolizis, diz, ankiloz The role of arthroscopic adhesiolysis in the treatment of the arthrofibrosis and the partial ankylosis of theknee The 27 knees of 23 patients with limited range of motion that developed after trauma, fractures or open surgical procedures of the distal femur were treated by the percutaneous release of the adhesions under art hroscopic control. The inteNal between the cause of the limited ROM and the arthroscopic adhesiolysis ran ged from 4 months to 24 months (mean: 7 months). The average preoperative ROM was 43° and the average postoperative ROM was 115°. The average loss from the postoperative ROM was 1r. At the fol/ow-up, the average final gain of ROM was 55°. Keywords: Arthroscopy, arthrofibrosis, adhesiolysis, knee, ankylosis. The pathogenesis of arthrofibrosis is not a single Another subgroup of the post-traumatic arthrofib process but there are multiple factors that play roles rosis is the Infrapatellar Contracture Syndrome in this procedure. -

Arthritis: a Radiologic Overview
Henry Ford Hosp Med Journal Vol 27, No 1, 1979 Arthritis: A Radiologic Overview Gordon H. Beute, MD* Fhediagnosisof arthritis is estabi ished bythe correlationof faces, alterations in the joint capsule or pericapsular clinical, laboratory and radiographic data. Some fundamen ligaments, and imbalance of action of opposing muscles tal aspects of radiographic evaluation will be reviewed. and tendons. The changes are often bilateral and symmetri cal. Secondary degenerative joint disease is uncommon Baseline radiographic study ofa patient with polyarthralgia except in the knees and hips, and when present it usually is should include films of involved joints and the contralateral not prominent. When the spine is involved, the cervical joints if they are presently asymptomatic. Generally, a region is most commonly affected. A typical finding is screening study for a peripheral arthritis should include a atlanto-axial subluxation. single view of the hands and wrists, not only because these sites are frequently affected during the course of the disease, Juvenile rheumatoid arthritis usually involves the knees, but because differential radiographic features are more ankles and wrists. Less often affected are the hands, elbows, apparent here than in other joints. The clinical presentation hips, feet, shoulders and cervical spine. Monoarticular may appropriately limit evaluation to a single joint, to the disease is more common in children than in adults. Ra appendicular skeleton or the axial skeleton. Serial studies diographic manifestations are similar to those in the adult are useful in assessing progression of the disease and but differ in several respects. Periosteal new bone is fre occasionally are helpful in differential diagnosis. -

Role of Talectomy in Severe Resistant Clubfoot in Children Mohammad a Hegazy1, Hossam M Khairy2, Sherif M El-Aidy3
RESEARCH ARTICLE Role of Talectomy in Severe Resistant Clubfoot in Children Mohammad A Hegazy1, Hossam M Khairy2, Sherif M El-Aidy3 ABSTRACT Despite of the global attention paid to talectomy in management of severe, rigid, and resistant deformities of clubfoot, no evaluation of this procedure has been done before in our institution. The aim of work was to evaluate the outcome of surgical removal of talus in these patients. Seventeen severe, rigid, and resistant clubfeet in 10 patients undergoing talectomy were evaluated pre- and postoperative at the Department of Orthopedic Surgery, Zagazig University hospitals, Al-Sharkia, Egypt. The collected data were statistically analyzed. Out of the 10 investigated cases, there were seven males and three females. Seven (70%) cases were bilaterally affected; only three (30%) were one-sided affected. They were one left-sided in two cases and the other was right-sided. Their age ranged 1–5 years with a mean of 30.2 ± 13.3 months. There were good results in 11 (65%) cases out of the 17 operated. Fair results were found in 6 (35%) cases. Three from the 6 feet with fair results following talectomy showed residual cavus; and the others were noticed with residual hindfoot varus with slight inversion and adduction of the forefoot. All cases were with stable and plantigrade foot. In general, patients of both good and fair results were being able to wear shoes and to walk independently with pain free movements. Talectomy could be considered as a single salvage procedure for cases of clubfoot suffering from rigid, resistant and severe deformities. -

Current Treatment Options for Refractory Osteoarthritis of Low-Motion Joints in Horses Santiago D
Current treatment options for refractory osteoarthritis of low-motion joints in horses Santiago D. Gutierrez-Nibeyro, DVM, MS, DACVS, DACVSMR Clinical Associate Professor of Equine Surgery Department of Veterinary Clinical Medicine, College of Veterinary Medicine University of Illinois Summary: Osteoarthritis of the distal intertarsal and tarsometatarsal joints is a common cause of lameness in all types of performance horses, but is particularly prevalent among Western performance horses. Osteoarthritis of the proximal interphalangeal joint, although less common among performance horses, is also a frequent cause of lameness in several breeds. This is an overview of the current treatment options available to potentially manage osteoarthritis of these low-motion joints in horses intended for athletic use. Treatment options for refractory osteoarthritis of the distal intertarsal and tarsometatarsal joints Medical management remains the best therapeutic option for osteoarthritis (OA) of the distal hock joints. The use of corrective shoeing, intra-articular hyaluronan and corticosteroids, and systemic non-steroidal anti-inflammatory medication allows most horses to continue in training and performance. Because of the reported detrimental effects on the articular cartilage, many veterinarians use methylprednisolone in the distal hock joints to accelerate or promote joint ankylosis. However, some horses do not respond well to anti-inflammatory injections or have only a short duration of response. Extracorporeal shock wave therapy (ESWT) is the generation of a pressure wave outside of the body, which is then directed at a specific area of the body for treatment. It has been hypothesized that symptomatic relief in patients treated with ESWT is the result of an analgesic effect. In humans, pain relief has been reported to occur within 3 weeks after therapy and may last indefinitely. -

Narrative Review of Ring Fixator Management of Recurrent Club Foot Deformity
1104 Review Article on Clubfoot Page 1 of 12 Narrative review of ring fixator management of recurrent club foot deformity Zachery Meyer1, Jacob R. Zide2, Alexander Cherkashin1^, Mikhail Samchukov1^, Daniel D. Bohl3, Anthony I. Riccio1^ 1Department of Orthopaedic Surgery, Texas Scottish Rite Hospital, Dallas, TX, USA; 2Department of Orthopaedic Surgery, Baylor University Medical Center, Dallas, TX, USA; 3Baylor University Medical Center, Department of Orthopaedic Surgery, Dallas, TX, USA Contributions: (I) Conception and design: AI Riccio, M Samchukov, A Cherkashin; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: None; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Anthony I. Riccio, MD. Texas Scottish Rite Hospital for Children, 2222 Welborn Street, Dallas, TX 75219, USA. Email: [email protected]. Abstract: Despite the widespread use of the Ponseti method for treatment of clubfeet, there continue to be a significant number of patients who present with a severe, stiff clubfoot as a result of extensive intra- articular soft tissue release or lack of access to care. In such patients, circular external fixators can be utilized for deformity correction with distraction across soft tissues, joints, and osteotomies. Ilizarov or hexapod circular fixators may be utilized according to surgeon preference. Indications for soft tissue release and osteotomies to aid in correction of clubfoot deformity with Ilizarov and hexapod fixators are not standardized and are guided by patient age, joint congruity, soft tissue suppleness, and osseous deformity. Correction time varies according to clubfoot deformity severity. -

Balneo Research Journal DOI: Vol.11, No.1, February 2020 P: 574–579
BALNEO RESEARCH JOURNAL Vol 11 No. 1, February 2020 Climatology Balneology Medical Hydrology Physical and Rehabilitation Medicine Website http://bioclima.ro/Journal.htm E-mail: [email protected] ISSN: 2069-7597 / eISSN: 2069-7619 Balneo Research Journal is part of the international data bases ﴾BDI﴿ as follow: EBSCOhost. CrossRef, DOAJ, Electronic ﴿Journals Library ﴾GIGA﴿, USA National Library of Medicine - NLM, Emerging Sources Citation Index ﴾Thomson Reuters ﴿Publisher: Romanian Association of Balneology ﴾Bucharest Asociatia Romana de Balneologie / Romanian Association of Balneology Editura Balneara Balneo Reserch Journal Table of Contents: Vol 11 No. 1, February 2020 (307) Effectiveness of pulmonary rehabilitation in improving quality of life in patients with different COPD stages - MARC Monica, PESCARU Camelia, ILIE Adrian Cosmin, CRIȘAN Alexandru, HOGEA STANCA Patricia, TRĂILĂ Daniel Balneo Research Journal. 2020;11(1):3–8 Full Text DOI 10.12680/balneo.2020.307 (308) A review of antimicrobial photodynamic therapy (aPDT) in periodontitis - CONDOR Daniela, CULCITCHI Cristian, BARU Oana, CZINNA Julia, BUDURU Smaranda Balneo Research Journal. 2020;11(1):9–13 Full Text DOI 10.12680/balneo.2020.308 (309) Effect of Low Level Laser Therapy (LLLT) on muscle pain in temporomandibular disorders – an update of literature - KUI Andreea, TISLER Corina, CIUMASU Alexandru, ALMASAN Oana, CONDOR Daniela, BUDURU Smaranda Balneo Research Journal. 2020;11(1):14–19 Full Text DOI 10.12680/balneo.2020.309 (310) The control of cardiovascular risk factors – an essential component of the rehabilitation of patients with ischemic heart disease. What are the current targets? - POP Dana, DĂDÂRLAT-POP Alexandra, CISMARU Gabriel, ZDRENGHEA Dumitru Balneo Research Journal. 2020;11(1):20–23 Full Text DOI 10.12680/balneo.2020.310 (311) Clinical-evolutive particularities and therapeutic-rehabilitative approach in the rare case of acute disseminated encephalomyelitis following an episode of viral meningitis of unknown etiology - ILUȚ Silvina, VACARAS Vitalie, RADU M. -
21-0960M-9 SUPERSEDES VA FORM 21-0960M-9, MAY 2013, Page 1 JUN 2017 WHICH WILL NOT BE USED
OMB Approved No. 2900-0813 Respondent Burden: 30 minutes Expiration Date: 06-30-2020 KNEE AND LOWER LEG CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - The veteran or service member is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. MEDICAL RECORD REVIEW WAS THE VETERAN'S VA CLAIMS FILE REVIEWED? YES NO IF YES, LIST ANY RECORDS THAT WERE REVIEWED BUT WERE NOT INCLUDED IN THE VETERAN'S VA CLAIMS FILE: IF NO, CHECK ALL RECORDS REVIEWED: Military service treatment records Department of Defense Form 214 Separation Documents Military service personnel records Veterans Health Administration medical records (VA treatment records) Military enlistment examination Civilian medical records Military separation examination Interviews with collateral witnesses (family and others who have known the veteran before and after military service) Military post-deployment questionnaire Other: No records were reviewed SECTION I - DIAGNOSIS NOTE: These are condition(s) for which an evaluation has been requested on an exam request form (Internal VA) or for which the Veteran has requested medical evidence be provided for submission to VA.