Regulation of Hepatic Insulin Signaling and Glucose Homeostasis by Sphingosine Kinase 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Gene Symbol Gene Description ACVR1B Activin a Receptor, Type IB
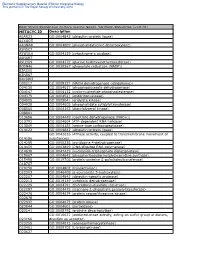
Table S1. Kinase clones included in human kinase cDNA library for yeast two-hybrid screening Gene Symbol Gene Description ACVR1B activin A receptor, type IB ADCK2 aarF domain containing kinase 2 ADCK4 aarF domain containing kinase 4 AGK multiple substrate lipid kinase;MULK AK1 adenylate kinase 1 AK3 adenylate kinase 3 like 1 AK3L1 adenylate kinase 3 ALDH18A1 aldehyde dehydrogenase 18 family, member A1;ALDH18A1 ALK anaplastic lymphoma kinase (Ki-1) ALPK1 alpha-kinase 1 ALPK2 alpha-kinase 2 AMHR2 anti-Mullerian hormone receptor, type II ARAF v-raf murine sarcoma 3611 viral oncogene homolog 1 ARSG arylsulfatase G;ARSG AURKB aurora kinase B AURKC aurora kinase C BCKDK branched chain alpha-ketoacid dehydrogenase kinase BMPR1A bone morphogenetic protein receptor, type IA BMPR2 bone morphogenetic protein receptor, type II (serine/threonine kinase) BRAF v-raf murine sarcoma viral oncogene homolog B1 BRD3 bromodomain containing 3 BRD4 bromodomain containing 4 BTK Bruton agammaglobulinemia tyrosine kinase BUB1 BUB1 budding uninhibited by benzimidazoles 1 homolog (yeast) BUB1B BUB1 budding uninhibited by benzimidazoles 1 homolog beta (yeast) C9orf98 chromosome 9 open reading frame 98;C9orf98 CABC1 chaperone, ABC1 activity of bc1 complex like (S. pombe) CALM1 calmodulin 1 (phosphorylase kinase, delta) CALM2 calmodulin 2 (phosphorylase kinase, delta) CALM3 calmodulin 3 (phosphorylase kinase, delta) CAMK1 calcium/calmodulin-dependent protein kinase I CAMK2A calcium/calmodulin-dependent protein kinase (CaM kinase) II alpha CAMK2B calcium/calmodulin-dependent -

Stimulating the Expression of Sphingosine Kinase 1 (Sphk1) Is Bene�Cial to Reduce Acrylamide-Induced Nerve Cell Damage
Stimulating the Expression of Sphingosine Kinase 1 (SphK1) is Benecial to Reduce Acrylamide-Induced Nerve Cell Damage Yong-Hui Wu ( [email protected] ) Harbin Medical University https://orcid.org/0000-0002-4838-2947 Sheng-Yuan Wang Harbin Medical University Xiao-Li Wang Harbin Medical University Rui Xin Harbin Medical University Ye Xin Harbin Medical University Rui Wang Harbin Medical University Kun Ma Harbin Medical University Cui-Ping Yu Harbin Medical University Dan Zhang Harbin Medical University Xiao-Rong Zhou Harbin Medical University Wei-Wei Ma Harbin Medical University Chao Wang Harbin Medical University Research Keywords: Acrylamide, SphKl, Neurotoxicity, Apoptosis, MAPK pathway Posted Date: September 28th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-80914/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Stimulating the expression of sphingosine kinase 1 (SphK1) is beneficial to reduce acrylamide-induced nerve cell damage Sheng-Yuan Wang1, Xiao-Li Wang1, Rui Xin1, Ye Xin1, Rui Wang1, Kun Ma2, Cui-Ping Yu1, Dan Zhang1, Xiao-Rong Zhou1, Wei-Wei Ma3, Chao Wang4, Yong-Hui Wu1* 1 Department of Occupational Health, Public Health College, Harbin Medical University, Harbin, P. R. 2 Department of Hygienic Toxicology, Public Health College, Harbin Medical University, Harbin, P. R. 3 Harbin Railway Center for Disease Control and Prevention, Harbin, P. R. 4 Health Commission of Heilongjiang Province. * Address correspondence to this author at: The Department of Occupational Health, Public Health College, Harbin Medical University, 157 Baojian Road, Nan gang District, Harbin, People’s Republic of China 150086. Phone: +86-451-8750-2827, Fax: +86-451-8750-2827, E-mail: [email protected]. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Supplementary Materials
1 Supplementary Materials: Supplemental Figure 1. Gene expression profiles of kidneys in the Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice. (A) A heat map of microarray data show the genes that significantly changed up to 2 fold compared between Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice (N=4 mice per group; p<0.05). Data show in log2 (sample/wild-type). 2 Supplemental Figure 2. Sting signaling is essential for immuno-phenotypes of the Fcgr2b-/-lupus mice. (A-C) Flow cytometry analysis of splenocytes isolated from wild-type, Fcgr2b-/- and Fcgr2b-/-. Stinggt/gt mice at the age of 6-7 months (N= 13-14 per group). Data shown in the percentage of (A) CD4+ ICOS+ cells, (B) B220+ I-Ab+ cells and (C) CD138+ cells. Data show as mean ± SEM (*p < 0.05, **p<0.01 and ***p<0.001). 3 Supplemental Figure 3. Phenotypes of Sting activated dendritic cells. (A) Representative of western blot analysis from immunoprecipitation with Sting of Fcgr2b-/- mice (N= 4). The band was shown in STING protein of activated BMDC with DMXAA at 0, 3 and 6 hr. and phosphorylation of STING at Ser357. (B) Mass spectra of phosphorylation of STING at Ser357 of activated BMDC from Fcgr2b-/- mice after stimulated with DMXAA for 3 hour and followed by immunoprecipitation with STING. (C) Sting-activated BMDC were co-cultured with LYN inhibitor PP2 and analyzed by flow cytometry, which showed the mean fluorescence intensity (MFI) of IAb expressing DC (N = 3 mice per group). 4 Supplemental Table 1. Lists of up and down of regulated proteins Accession No. -

Activation of Sphingosine Kinase 1 by ERK1/2Mediated Phosphorylation
The EMBO Journal Vol. 22 No. 20 pp. 5491±5500, 2003 Activation of sphingosine kinase 1 by ERK1/2-mediated phosphorylation Stuart M.Pitson1,2, Paul A.B.Moretti1, second messenger and a ligand for cell-surface receptors Julia R.Zebol1, Helen E.Lynn1, Pu Xia1,3, (Hla et al., 2001; Spiegel and Milstien, 2002). MathewA.Vadas 1,3 and The cellular levels of S1P are controlled by its Binks W.Wattenberg1,4 formation from sphingosine through the activity of sphingosine kinase, and by its degradation by S1P lyase 1Hanson Institute, Division of Human Immunology, Institute of (Van Veldhoven et al., 2000) and S1P phosphatases Medical and Veterinary Science, Frome Road, Adelaide, SA 5000 and (Mandala, 2001). In the basal state, this balance between 3Department of Medicine, Adelaide University, Frome Road, Adelaide, Australia S1P generation and degradation results in low cellular levels of S1P (Pyne and Pyne, 2000). However, when cells 4Present address: James Graham Brown Cancer Center, Dehlia Baxter Research Building, 580 S. Preston Avenue, Louisville, KY 40202, are exposed to speci®c growth factors and other agonists USA like tumour necrosis factor-a (TNFa) or phorbol esters the cellular levels of S1P can increase rapidly and transiently 2Corresponding author e-mail: [email protected] (Pitson et al., 2000b). This results in the triggering of various signalling pathways through as yet unidenti®ed Sphingosine kinase 1 is an agonist-activated signalling intracellular S1P targets, as well as through the engage- enzyme that catalyses the formation of sphingosine ment of cell surface S1P receptors following its release 1-phosphate, a lipid second messenger that has been from cells (Hobson et al., 2001). -

Interaction of 6-Phosphofructo-2-Kinase/Fructose-2,6- Bisphosphatase (PFK-2/Fbpase-2) with Glucokinase Activates Glucose Phospho
Interaction of 6-Phosphofructo-2-Kinase/Fructose-2,6- Bisphosphatase (PFK-2/FBPase-2) With Glucokinase Activates Glucose Phosphorylation and Glucose Metabolism in Insulin-Producing Cells Laura Massa,1 Simone Baltrusch,1 David A. Okar,2,3 Alex J. Lange,2 Sigurd Lenzen,1 and Markus Tiedge1 The bifunctional enzyme 6-phosphofructo-2-kinase/ fructose-2,6-bisphosphatase (PFK-2/FBPase-2) was re- cently identified as a new intracellular binding partner he enzyme glucokinase (GK) plays a pivotal role for glucokinase (GK). Therefore, we studied the impor- in the recognition of glucose in pancreatic tance of this interaction for the activity status of GK -cells and the regulation of glucose metabolism and glucose metabolism in insulin-producing cells by Tin the liver (1–7). In pancreatic -cells, GK acts overexpression of the rat liver and pancreatic islet as a glucose sensor and catalyzes the rate-limiting step for isoforms of PFK-2/FBPase-2. PFK-2/FBPase-2 overex- initiation of glucose-induced insulin secretion (6). GK is pression in RINm5F-GK cells significantly increased the regulated in a complex manner in pancreatic -cells by GK activity by 78% in cells expressing the islet isoform, posttranslational modifications of the enzyme protein that by 130% in cells expressing the liver isoform, and by mainly depend on the intracellular glucose concentration 116% in cells expressing a cAMP-insensitive liver S32A/ (8–13). These posttranslational mechanisms of GK activity H258A double mutant isoform. Only in cells overex- regulation are comprised of conformational changes pressing the wild-type liver PFK-2/FBPase-2 isoform (14,15), sulfhydryl-group conversions (16–18), and inter- was the increase of GK activity abolished by forskolin,  apparently due to the regulatory site for phosphoryla- actions with -cell matrix proteins (13,19), insulin gran- tion by a cAMP-dependent protein kinase. -

4-6 Weeks Old Female C57BL/6 Mice Obtained from Jackson Labs Were Used for Cell Isolation
Methods Mice: 4-6 weeks old female C57BL/6 mice obtained from Jackson labs were used for cell isolation. Female Foxp3-IRES-GFP reporter mice (1), backcrossed to B6/C57 background for 10 generations, were used for the isolation of naïve CD4 and naïve CD8 cells for the RNAseq experiments. The mice were housed in pathogen-free animal facility in the La Jolla Institute for Allergy and Immunology and were used according to protocols approved by the Institutional Animal Care and use Committee. Preparation of cells: Subsets of thymocytes were isolated by cell sorting as previously described (2), after cell surface staining using CD4 (GK1.5), CD8 (53-6.7), CD3ε (145- 2C11), CD24 (M1/69) (all from Biolegend). DP cells: CD4+CD8 int/hi; CD4 SP cells: CD4CD3 hi, CD24 int/lo; CD8 SP cells: CD8 int/hi CD4 CD3 hi, CD24 int/lo (Fig S2). Peripheral subsets were isolated after pooling spleen and lymph nodes. T cells were enriched by negative isolation using Dynabeads (Dynabeads untouched mouse T cells, 11413D, Invitrogen). After surface staining for CD4 (GK1.5), CD8 (53-6.7), CD62L (MEL-14), CD25 (PC61) and CD44 (IM7), naïve CD4+CD62L hiCD25-CD44lo and naïve CD8+CD62L hiCD25-CD44lo were obtained by sorting (BD FACS Aria). Additionally, for the RNAseq experiments, CD4 and CD8 naïve cells were isolated by sorting T cells from the Foxp3- IRES-GFP mice: CD4+CD62LhiCD25–CD44lo GFP(FOXP3)– and CD8+CD62LhiCD25– CD44lo GFP(FOXP3)– (antibodies were from Biolegend). In some cases, naïve CD4 cells were cultured in vitro under Th1 or Th2 polarizing conditions (3, 4). -

New Nucleotide Sequence Data on the EMBL File Server
.=) 1991 Oxford University Press Nucleic Acids Research, Vol. 19, No. 2 413 New nucleotide sequence data on the EMBL File Server October 30, 1990 to November 13, 1990 New nucleotide sequence data, available from the EMBL File Server, (see Stoehr, P.J. and Omond, R.A. (1989) Nucleic Acids Res., 17 (16), 6763 -6764), are reported below. Availability of all the newest sequence data is the result of collaboration between.the EMBL Data Library and GenBank' , and data are supplied regularly by both groups. Updates to existing data are not reported here. This report has been prepared by the EMBL Data Library. PRIMATES: Human casein kinase II alpha subunit mRNA, complete cds. Human specific HS5 DNA Lozeman F.J., Litchfield D.W., Piening C., Takio K., Walsh Ueda S., Washio K., Kurosaki K.; K.A., Krebs E.G.; Genomics 8:7-12(1990). X17579 Biochemistry 29:8436-8447(1990). M55268 Human mRNA for heat shock protein HSP27 Human mRNA for actin-binding protein (ABP-280) Carper S.W., Rocheleau T.A., Storm F.K.; Gorlin J.B., Yamin R., Egan S., Stewart M., Stossel T.P., Nucleic Acids Res. 18:6457-6457(1990). X54079 Kwiatkowski D.J., Hartwig J.H.; J. Cell Biol. 111:1089-1105(1990). X53416 Human Ig germline H-chain D-region Dxpl and Dxp'1 genes, 3' Human amiloride-binding protein, complete cds. end. Barbry P., Champe M., Chassande O., Munemitsu S., Champigny Huang C., Stollar B.David.; G., Lingueglia E., Maes P., Frelin C., Tartar A., Ullrich A., Unpublished. M37485 Lazdunski M.; Proc. Natl. Acad. -

Lipid Metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives
cancers Review Lipid metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives 1, 1, 1 2 1 Laurence Pellerin y, Lorry Carrié y , Carine Dufau , Laurence Nieto , Bruno Ségui , 1,3 1, , 1, , Thierry Levade , Joëlle Riond * z and Nathalie Andrieu-Abadie * z 1 Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, Université Fédérale de Toulouse Midi-Pyrénées, Université Toulouse III Paul-Sabatier, Inserm 1037, 2 avenue Hubert Curien, tgrCS 53717, 31037 Toulouse CEDEX 1, France; [email protected] (L.P.); [email protected] (L.C.); [email protected] (C.D.); [email protected] (B.S.); [email protected] (T.L.) 2 Institut de Pharmacologie et de Biologie Structurale, CNRS, Université Toulouse III Paul-Sabatier, UMR 5089, 205 Route de Narbonne, 31400 Toulouse, France; [email protected] 3 Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France * Correspondence: [email protected] (J.R.); [email protected] (N.A.-A.); Tel.: +33-582-7416-20 (J.R.) These authors contributed equally to this work. y These authors jointly supervised this work. z Received: 15 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Simple Summary: Melanoma is a devastating skin cancer characterized by an impressive metabolic plasticity. Melanoma cells are able to adapt to the tumor microenvironment by using a variety of fuels that contribute to tumor growth and progression. In this review, the authors summarize the contribution of the lipid metabolic network in melanoma plasticity and aggressiveness, with a particular attention to specific lipid classes such as glycerophospholipids, sphingolipids, sterols and eicosanoids. -
Cdna Sequence and Tissue Expression Analysis of Glucokinase from Liver of Grass Carp (Ctenopharyngodon Idella )
African Journal of Biotechnology Vol. 11(3), pp. 534-542, 10 January, 2012 Available online at http://www.academicjournals.org/AJB DOI: 10.5897/AJB11.3174 ISSN 1684–5315 © 2012 Academic Journals Full Length Research Paper cDNA sequence and tissue expression analysis of glucokinase from liver of grass carp (Ctenopharyngodon idella ) CHENG Han-liang*, JI Nan-jing, PENG Yong-xing, SHEN Xin, XU Jian-he, DONG Zhi-guo and WU Chen-chen Jiangsu Key Laboratory of Marine Biotechnology, Huaihai Institute of Technology, Lianyungang 222005, People’s Republic of China. Accepted 19 December, 2011 A full-length cDNA coding glucokinase (GK) was cloned from the liver of grass carp ( Ctenopharyngodon idella ) by reverse transcriptase-polymerase chain reaction (RT-PCR) and rapid amplification of cDNA ends methods. The cDNA obtained was 2066 bp exclusive of poly (A) residues with a 1431 bp open reading frame encoding 476 amino acids. The GK protein has a calculated molecular weight of 53.7 kDa and isoelectric point of 5.11. Some conserved functional sites were found including one conserved hexokinase signature sequence Leu 156 -Phe 181 ; two N-linked glycosylation sites Asn 176 and Asn 214 ; one cell attachment sequence Arg 202 -Asp 204 ; one glycosaminoglycan attachment site Ser455 -Gly 458 . The amino acid sequence has a high similarity to GK of other species, the percent identity compared with topmouth culter, common carp, human and rat are 98.1, 96.8, 80.3 and 79.8%, respectively. Tissue distribution of GK mRNA in brain, mesenteric adipose tissue, spleen, white muscle and liver of grass carp was analyzed by SYBR real-time fluorescence quantitative RT-PCR method using β-actin as an internal control for cDNA normalization. -

Balance Between Senescence and Apoptosis Is Regulated by Telomere Damage–Induced Association Between P16 and Caspase-3
JBC Papers in Press. Published on May 10, 2018 as Manuscript RA118.003506 The latest version is at http://www.jbc.org/cgi/doi/10.1074/jbc.RA118.003506 Balance between senescence and apoptosis is regulated by telomere damage–induced association between p16 and caspase-3 Shanmugam Panneer Selvam1,2, Braden M. Roth1,2, Rose Nganga1,2, Jisun Kim1,2, Marion A. Cooley3,#, Kristi Helke4, Charles D. Smith5, and Besim Ogretmen1,2* 1Department of Biochemistry and Molecular Biology, 2Hollings Cancer Center, 3Department of Regenerative Medicine, 4Department of Comparative Medicine, Medical University of South Carolina, 86 Jonathan Lucas Street, Charleston, SC 29425; 5Department of Pharmacology, Pennsylvania State University, 500 University Drive, Hershey, PA 17033. #Current Address: Department of Oral Biology, Augusta University, Augusta, GA 30912. *Address correspondence to: [email protected] Running title: p16-caspase-3 complex and senescence Key words: apoptosis; senescence; sphingolipid; sphingosine 1-phosphate; telomere damage Downloaded from Abstract damage–induced apoptosis, indicating that an Telomerase activation protects cells from telomere association between p16 and caspase-3 damage by delaying senescence and inducing cell proteinsforces senescence induction by inhibiting immortalization, whereas telomerase inhibition caspase- 3 activation and apoptosis. These results http://www.jbc.org/ mediates rapid senescence or apoptosis. However, suggest that p16 plays a direct role in telomere the cellular mechanisms that determine telomere damage–dependent senescence by limiting damage–dependent senescence versus apoptosis apoptosis via binding to caspase-3, revealing a induction are largely unknown. Here, we direct link between telomere damage–dependent demonstrate that telomerase instability mediated senescence and apoptosis with regards to aging by guest on May 31, 2018 by silencing of sphingosine kinase 2 (SPHK2) and and cancer.