Hystopathological Study of the Intestinal Epithelium Submitted to Different Times of Programmed Ischemia and Twenty Four Hours Reperfusion1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
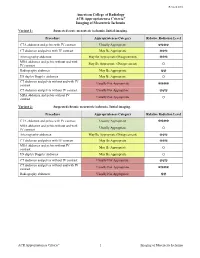
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Mesenteric Ischemia
The new england journal of medicine Review Article Edward W. Campion, M.D., Editor Mesenteric Ischemia Daniel G. Clair, M.D., and Jocelyn M. Beach, M.D. esenteric ischemia is caused by blood flow that is insuffi- From the Cleveland Clinic Lerner College cient to meet the metabolic demands of the visceral organs. The severity of Medicine of Case Western Reserve University (D.G.C.) and the Department of ischemia and the type of organ involved depend on the affected vessel of Vascular Surgery, Heart and Vascular M Institute, Cleveland Clinic (D.G.C., J.M.B.) and the extent of collateral-vessel blood flow. Despite advances in the techniques used to treat problems in the mesenteric — both in Cleveland. Address reprint re- quests to Dr. Clair at the Department of circulation, the most critical factor influencing outcomes in patients with this Vascular Surgery, Cleveland Clinic, 9500 condition continues to be the speed of diagnosis and intervention. Although mes- Euclid Ave., Desk F30, Cleveland, OH enteric ischemia is an uncommon cause of abdominal pain, accounting for less 44195, or at claird@ ccf . org. than 1 of every 1000 hospital admissions, an inaccurate or delayed diagnosis can N Engl J Med 2016;374:959-68. result in catastrophic complications; mortality among patients in whom this con- DOI: 10.1056/NEJMra1503884 Copyright © 2016 Massachusetts Medical Society. dition is acute is 60 to 80%.1-3 This article highlights the pathophysiological features, diagnosis, and treat- ment of ischemic syndromes in the foregut and intestines. The goal of this review is to improve the understanding and management of this life-threatening disorder. -

Acute Mesenteric Ischemia Revealing Cirrhosis: About a Clinical Case
Gastroenterology & Hepatology: Open Access Case Report Open Access Acute mesenteric ischemia revealing cirrhosis: about a clinical case Abstract Volume 11 Issue 2 - 2020 Acute mesenteric ischemia (AMI) is a rare and serious medical and surgical emergency, the 1 1 2 prognosis of which depends on the early diagnosis and appropriate treatment. It is caused Kpossou AR, Sokpon CNM, Doukpo MM, 3 4 5 1 by acute or chronic interruption of splanchno-mesenteric blood flow. This interruption may Gandji EW, Diallo K, Laleye C, Vignon RK, be due to embolism, thrombosis or intestinal hypoperfusion. We report a case of acute Eyisse-Kpossou YOT,5 Sehonou J1 mesenteric ischemia in a young subject in a National Hospital and University Center of 1Departement of Hepato-gastroenterology, National and Benin. He was a 23-year-old man with no history of admitting a diffuse abdominal pain, University Hospital Hubert Koutoukou Maga (CNHU-HKM), excruciating, sudden onset of torsion and associated vomiting and stopping of materials and Benin 2 gases. Emergency laparotomy revealed acute mesenteric ischemia with ileal necrosis. Ileal Departement of Hepato-gastroenterology, National and resection with endo-ileal endo- ileal anastomosis was performed. Etiological research has University Hospital Hubert Koutoukou Maga (CNHU-HKM), Benin revealed cirrhosis of undetermined cause. The postoperative course was marked by short 3Departement of Visceral Surgery, National and University bowel syndrome and ascitic decompensation of cirrhosis. Under symptomatic treatment, Hospital -

Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S
Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S. Naval Hospital Sigonella, Sigonella, Italy DWAYNE C. CLARK, M.D., Fond du Lac Regional Clinic, Fond du Lac, Wisconsin Acute abdominal pain is a common presenting complaint in older patients. Presentation may differ from that of the younger patient and is often complicated by coexistent disease, delays in presentation, and physical and social barri- ers. The physical examination can be misleadingly benign, even with catastrophic conditions such as abdominal aortic aneurysm rupture and mesenteric ischemia. Changes that occur in the biliary system because of aging make older patients vulnerable to acute cholecystitis, the most common indication for surgery in this population. In older patients with appendicitis, the initial diagnosis is correct only one half of the time, and there are increased rates of perforation and mortality when compared with younger patients. Medication use, gallstones, and alcohol use increase the risk of pancreatitis, and advanced age is an indicator of poor prognosis for this disease. Diverticulitis is a common cause of abdominal pain in the older patient; in appropriately selected patients, it may be treated on an outpatient basis with oral antibiotics. Small and large bowel obstructions, usually caused by adhesive disease or malignancy, are more common in the aged and often require surgery. Morbidity and mortality among older patients presenting with acute abdominal pain are high, and these patients often require hospitalization with prompt surgical consultation. (Am Fam Physician 2006;74:1537-44. Copyright © 2006 American Academy of Family Physicians.) cute abdominal pain (generally sultation.2,11 In retrospective studies, more defined as pain of less than one than one half of older patients presenting week’s duration) is a common to the emergency department with acute presenting complaint among abdominal pain required hospital admission, Aolder patients. -

Portal Vein Thrombosis
Portal Vein Thrombosis a a Syed Abdul Basit, MD , Christian D. Stone, MD, MPH , b, Robert Gish, MD * KEYWORDS Thrombosis Cirrhosis Portal vein Anticoagulation Thrombophilia Thromboelastography Malignancy KEY POINTS Portal vein thrombosis (PVT) is most commonly found in cirrhosis and often diagnosed incidentally by imaging studies. There are 3 important complications of PVT: Portal hypertension with gastrointestinal bleeding, small bowel ischemia, and acute ischemic hepatitis. Acute PVT is associated with symptoms of abdominal pain and/or acute ascites, and chronic PVT is characterized by the presence of collateral veins and risk of gastrointestinal bleeding. Treatment to prevent clot extension and possibly help to recanalize the portal vein is generally recommended for PVT in the absence of contraindications for anticoagulation. PVT may obviate liver transplantation owing to a lack of adequate vasculature for organ/ vessel anastomoses. INTRODUCTION Definition Portal vein thrombosis (PVT) is defined as a partial or complete occlusion of the lumen of the portal vein or its tributaries by thrombus formation. Diagnosis of PVT is occurring more frequently, oftentimes found incidentally, owing to the increasing use of abdom- inal imaging (Doppler ultrasonography, most commonly) performed in the course of routine patient evaluations and surveillance for liver cancer. There are 3 important clinical complications of PVT: Small bowel ischemia: PVT may extend hepatofugal, causing thrombosis of the mesenteric venous arch and resultant small intestinal ischemia, which has a mortality rate as high as 50% and may require small bowel or multivisceral trans- plant if the patient survives.1 a Section of Gastroenterology and Hepatology, University of Nevada School of Medicine, 2040 West Charleston Boulevard, Suite 300, Las Vegas, NV 89102, USA; b Division of Gastroenter- ology and Hepatology, Department of Medicine, Stanford University School of Medicine, Alway Building, Room M211, 300 Pasteur Drive, MC: 5187 Stanford, CA 94305-5187, USA * Corresponding author. -

Acute Mesenteric Ischemia: Guidelines of the World Society of Emergency Surgery Miklosh Bala1*, Jeffry Kashuk2, Ernest E
Bala et al. World Journal of Emergency Surgery (2017) 12:38 DOI 10.1186/s13017-017-0150-5 REVIEW Open Access Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery Miklosh Bala1*, Jeffry Kashuk2, Ernest E. Moore3, Yoram Kluger4, Walter Biffl5, Carlos Augusto Gomes6, Offir Ben-Ishay4, Chen Rubinstein7, Zsolt J. Balogh8, Ian Civil9, Federico Coccolini10, Ari Leppaniemi11, Andrew Peitzman12, Luca Ansaloni10, Michael Sugrue13, Massimo Sartelli14, Salomone Di Saverio15, Gustavo P. Fraga16 and Fausto Catena17 Abstract Acute mesenteric ischemia (AMI) is typically defined as a group of diseases characterized by an interruption of the blood supply to varying portions of the small intestine, leading to ischemia and secondary inflammatory changes. If untreated, this process will eventuate in life threatening intestinal necrosis. The incidence is low, estimated at 0.09–0.2% of all acute surgical admissions. Therefore, although the entity is an uncommon cause of abdominal pain, diligence is always required because if untreated, mortality has consistently been reported in the range of 50%. Early diagnosis and timely surgical intervention are the cornerstones of modern treatment and are essential to reduce the high mortality associated with this entity. The advent of endovascular approaches in parallel with modern imaging techniques may provide new options. Thus, we believe that a current position paper from World Society of Emergency Surgery (WSES) is warranted, in order to put forth the most recent and practical recommendations for diagnosis and treatment of AMI. This review will address the concepts of AMI with the aim of focusing on specific areas where early diagnosis and management hold the strongest potential for improving outcomes in this disease process. -

Ischemic Colitis Overview Ischemic Colitis, Although Rare, Is the Most Frequent Form of Mesenteric Ischemia, Affecting Mostly Th
Ischemic Colitis Overview Ischemic colitis, although rare, is the most frequent form of mesenteric ischemia, affecting mostly the elderly. Ischemia is caused when the blood supply does not reach the tissue deliver- ing the necessary oxygen. Without oxygen, cells begin to die which may cause tissue damage, tissue destruction, colon strictures or in extreme cases gangrene. The mesentery is a vital net- work of blood vessels that supply the colon with the necessary blood, oxygen and nutrients. The mesentery is initially divided into four main channels that feed the different sections of the colon. Eventually the vessels are divided into hundreds of channels supporting the continually working small and large intestine. Ischemia can occur in any of the branches of the mesentery. Despite the presence of so many vessels, the colon blood supply has two weak points. Narrow branches of the network supply the splenic flexure and the rectosigmoid junction. These two watershed areas are most vulnerable to ischemia. The larger the vessel that is blocked, the more tissue damage that will be caused. Causes Blockages or poor blood flow can be caused by a variety of reasons. Often the reason for the event cannot be identified, especially because it most often occurs in debilitated patients with multiple health problems. Spontaneous spasm, and occlusion of the vessel or low blood flow can cause the ischemia. When this happens 75%-85% of patients are effected in the water shed areas described above. Usually the event is limited and the patient recovers on their own. Only a small portion of these patients develop long-term complications, which may include per- sistent colitis or inflammation in a portion of the colon and/or the development of a stricture. -

Intussusception in Children: Not Only Surgical Treatment
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2017;6(1):e060135 doi: 10.7363/060135 Received: 2016 Sept 23; revised: 2016 Dec 08; accepted: 2016 Dec 08; published online: 2017 Feb 25 Original article Intussusception in children: not only surgical treatment Anna Maria Caruso, Alessandro Pane, Andrea Scanu, Alessandro Muscas, Roberto Garau, Franco Caddeo, Luigi Mascia Pediatric Surgery Unit, A.O. Brotzu, Cagliari, Italy Abstract Introduction: Intussusception is the commonest cause of acute in testinal obstruction in children. Failure of timely diagnosis and treatment results in a surgical emergency leading to fatal outcome. The classic triad of symptoms is seen in less than onethird of the children affected. Aim of this study was to evaluate the comprehensive management of intussusception in children, evaluating the outcome of conservative treatment with hydrostatic ultrasound reduction and surgery. Material and methods: A retrospective analysis was conducted including pediatric patients (up to 14 years old) with diagnosis of bowel intussusception. The management and treatment depended on the patients’ situation: for children in good general conditions initial hydrostatic reduction under continuous ultrasonographic monitoring was attempted; if severe dehydration and/or septic shock was observed, the conservative treatment was contraindicated and direct surgical treatment was performed. Result: A total of 44 pediatric patients were included in the study. The most frequent symptoms observed were paroxysmal abdominal pain (100% of cases) and vomiting (72%); only 29% of patients presented with the classic triad of symptoms (abdominal pain, palpable mass and blood stained stools). 28 patients (64%) were managed conservatively with ultrasound hydrostatic reduction. -

ACS/ASE Medical Student Core Curriculum: Vomiting, Diarrhea, And
ACS/ASE Medical Student Core Curriculum Vomiting, Diarrhea, and Constipation VOMITING, DIARRHEA, AND CONSTIPATION VOMITING The occurrence of vomiting may be the result of both gastrointestinal (GI) and non-GI causes. Categorization of the cause of vomiting is often segregated by the presence or absence of abdominal pain. Benign causes of vomiting often do not present with abdominal pain. These benign causes of vomiting are often the results of medications (including chemotherapy), motion sickness, food poisoning, infectious gastroenteritis, hepatitis, upper GI bleeding, postoperative ileus, or acute central nervous system disease. A thorough history of present illness as well as determination of associated symptoms may very well identify the etiology for these benign causes of vomiting. More concerning causes of vomiting are those associated with abdominal pain. These often include potentially serious conditions that may require surgical intervention, including gastrointestinal obstruction, mesenteric ischemia, pancreatitis, biliary colic, and perforated intestine causing peritonitis, as in the case of perforated appendicitis. The presence of bilious emesis is more concerning for a bowel obstructive process, or protracted ileus from complications of one of the above-noted diagnoses, and often warrants more acute evaluation and assessment. Gastric obstruction is a common occurrence in children but a rare and concerning diagnosis in adults. Infants may develop a progressive obstruction of the gastric pylorus in a disease of hypertrophic pyloric stenosis. This process, which has some genetic and environmental contributions to its development, leads to the progressive hypertrophy of the pylorus to the point of near-complete obstruction. Presentation of these children often occurs before the third month of life with symptoms of persistent non-bilious vomiting and often severe dehydration and classic metabolic alkalosis from electrolyte loss. -

When to Suspect Ischemic Colitis Recognition of Ischemic Colitis Requires a High Level of Suspicion Because Presenting Symptoms Can Often Be Misleading
When to Suspect Ischemic Colitis Recognition of ischemic colitis requires a high level of suspicion because presenting symptoms can often be misleading. The authors identify causes of this variable and potentially deadly condition and discuss strategies for diagnosis and treatment. By Carlos J. Roldan, MD, FAAEM, FACEP, Sarah Noffsinger, MD, and Scott Wiesenborn, MD schemic colitis, the most common form of in- testinal ischemic pathology, was first reported secondary to inferior mesenteric artery ligation during surgical procedures involving the aorta Ior the colon but is now thought to be a multifactorial event.1 Although its reported predominance is in the elderly, it can affect individuals ranging in age from 29 to 98 years, depending on the predisposing risk factors. Ischemic colitis causes as many as one in 1,000 hospitalizations in the US each year.2,3 The clinical presentation and course of ischemic colitis vary widely, ranging from transient self-limit- ing ischemia with minimal sequelae to acute fulmi- nant ischemia with transmural infarction that may progress to necrosis and death.4 A careful history may detail predisposing factors for ischemic coli- tis, including atherosclerosis, embolic event, aortic Colonoscopy showing ischemic colitis. © 2009 ISM/Phototake aneurysm, recent surgery, and dehydration. A bet- one episode of vomiting. At that point he called for ter understanding of the relevant anatomy and the an ambulance. The EMS team established intrave- precipitating factors may increase the awareness, and nous access and administered oxygen and aspirin en thereby improve the recognition and diagnosis, of route to the hospital. On arrival, the patient’s pain this condition in the emergency department. -

Superior Mesenteric Vein Thrombosis As a Complication of Crohn's Disease
Case Report Open Access J Surg Volume 3 Issue 5 -April 2017 Copyright © All rights are reserved by Oktay Yener DOI: 10.19080/OAJS.2017.03.555624 Superior Mesenteric Vein Thrombosis as a Complication of Crohn’s Disease: An Unusual Case Oktay Yener* Department of General Surgery, Göztepe Training and Research Hospital, Turkey Submission: April 22, 2017; Published: April 28, 2017 *Corresponding author: ; Email: Oktay Yener, Department of General Surgery, Plaj Yolu Yıldız Sok. Kaya Apt. No: 16 D: 10 Caddebostan, İstanbul, Turkey, Tel: Abstract Background: Mesenteric venous thrombosis (MVT) is a rare but potentially catastrophic clinical complication, which may lead to ischemia or infarctionMethods: of the intestine. We report here a case of superior mesenteric vein (SMV) thrombosis in a 21 year old male patient with no history of Crohn’s disease or other risk factors of thrombosis. Patient was admitted to the hospital with the signs and symptoms of small bowel obstruction. He was taken to the operating room after the initial diagnostic tests and underwent partial small bowel resection followed by end to end anastomosis. İntraoperativeResults: diagnosis was acute mesenteric ischemia (AMI). Conclusion:Final pathological evaluation of the resected specimen was confirmed as demonstrating features of Crohn’s disease. Keywords: Crohn’s disease should be considered as one of the underlying causes when AMI is the diagnosis. Abbreviations: Crohn’s disease; Acute mesenteric ischemia, Intestinal obstruction AMI: Acute mesenteric ischemia; CT: Computed tomography; IV: Intravenous; MVT: Mesenteric venous thrombosis; SMV: Superior mesenteric vein Introduction of treatment [6,7]. We report here a case of SMV thrombosis in Acute mesenteric venous ischemia is a serious acute a 21 year old male patient with no history of Crohn’s disease or abdominal condition requiring early diagnosis and intervention other risk factors of thrombosis.