Abnormal Liver Functions As a Risk Factor for Acute Mesenteric Ischemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ischaemic Colitis: Practical Challenges and Evidence-Based Recommendations For
Ischaemic Colitis: Practical Challenges and Evidence-Based Recommendations for Management Alexander Hung1*, Tom Calderbank1*, Mark A Samaan1, Andrew A Plumb2, George Webster1 Author affiliations 1Department of Gastroenterology, University College London Hospitals, London, UK 2Department of Radiology, University College London Hospitals, London, UK *Authors contributed equally Correspondence to Mark A Samaan Department of Gastroenterology University College London Hospitals 250 Euston Road London NW1 2PG [email protected] Running title Ischaemic Colitis Management Word count 3212 Key Words Ischaemic colitis, colonic ischaemia ABSTRACT Ischaemic colitis (IC) is a common condition with rising incidence and, in severe cases, a high mortality rate. Its presentation, severity and disease behaviour can vary widely and there exists significant heterogeneity in treatment strategies and resultant outcomes. In this article we explore practical challenges in the management of IC and where available, make evidence-based recommendations for its management based on a comprehensive review of available literature. An optimal approach to initial management requires early recognition of the diagnosis followed by prompt and appropriate investigation. Ideally, this should involve the input of both gastroenterology and surgery. CT with intravenous and oral contrast is the imaging modality of choice. It can support a clinical diagnosis, define the severity and distribution of ischaemia and has prognostic value. In all but fulminant cases, this should be followed (within 48 hours) by lower GI endoscopy to reach the distal-most extent of the disease, providing endoscopic (and histological) confirmation. The mainstay of medical management is conservative/supportive treatment, with bowel rest, fluid resuscitation and antibiotics. Specific laboratory, radiological and endoscopic features are recognised to correlate with more severe disease, higher rates of surgical intervention and ultimately worse outcomes. -

Ischemic Colitis Caused by Polycythemia Vera: a Case Report and Literature Review
EXPERIMENTAL AND THERAPEUTIC MEDICINE 16: 3663-3667, 2018 Ischemic colitis caused by polycythemia vera: A case report and literature review SHASHA ZHANG1, RUIXUE LAI1, XUEQING GAO1, YUFEI ZHAO1, YUE ZHAO2, JIANHUA WU3 and ZHANJUN GUO1 Departments of 1Rheumatology and Immunology, and 2Gastroenterology and Hepatology, 3Animal Center, The Fourth Hospital of Hebei Medical University, Shijiazhuang, Hebei 050011, P.R. China Received January 16, 2018; Accepted August 10, 2018 DOI: 10.3892/etm.2018.6638 Abstract. Polycythemia vera (PV) is a chronic myeloproliferative Ischemic colitis (IC) can be described as an ischemic disease disorder originating from hematopoietic stem cells and of the colon, which results from decreased blood flow due to complicated by thrombosis and bleeding. This report describes a various causes that leads to intestinal wall ischemia, injury or case of ischemic colitis (IC) caused by PV and includes a review necrosis (3). The risk factors for IC mainly include diabetes, of the relevant literature. The patient was a 59-year-old male hypertension, dyslipidemia, peripheral vascular disease, with a history of PV who presented with abdominal pain and aspirin administration, and digoxin or constipation-inducing hematochezia. Colonoscopy and histopathological examination medications (4). The main clinical manifestations include results indicated suspected ischemic bowel disease. Following abdominal pain, diarrhea, and hematochezia (5). A reliable experimental anticoagulant therapy for 7 days, the patient no diagnosis of IC depends on the comprehensive evaluation of longer experienced abdominal pain and hematochezia had clinical symptoms, biochemical tests, radiological examina- resolved. Colonoscopy review showed no obvious anomalies tions, and endoscopic assessments (6). In certain cases, PV 1 month later. -
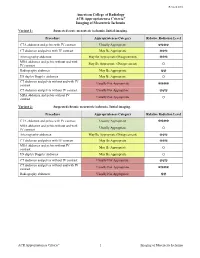
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Mesenteric Ischemia
The new england journal of medicine Review Article Edward W. Campion, M.D., Editor Mesenteric Ischemia Daniel G. Clair, M.D., and Jocelyn M. Beach, M.D. esenteric ischemia is caused by blood flow that is insuffi- From the Cleveland Clinic Lerner College cient to meet the metabolic demands of the visceral organs. The severity of Medicine of Case Western Reserve University (D.G.C.) and the Department of ischemia and the type of organ involved depend on the affected vessel of Vascular Surgery, Heart and Vascular M Institute, Cleveland Clinic (D.G.C., J.M.B.) and the extent of collateral-vessel blood flow. Despite advances in the techniques used to treat problems in the mesenteric — both in Cleveland. Address reprint re- quests to Dr. Clair at the Department of circulation, the most critical factor influencing outcomes in patients with this Vascular Surgery, Cleveland Clinic, 9500 condition continues to be the speed of diagnosis and intervention. Although mes- Euclid Ave., Desk F30, Cleveland, OH enteric ischemia is an uncommon cause of abdominal pain, accounting for less 44195, or at claird@ ccf . org. than 1 of every 1000 hospital admissions, an inaccurate or delayed diagnosis can N Engl J Med 2016;374:959-68. result in catastrophic complications; mortality among patients in whom this con- DOI: 10.1056/NEJMra1503884 Copyright © 2016 Massachusetts Medical Society. dition is acute is 60 to 80%.1-3 This article highlights the pathophysiological features, diagnosis, and treat- ment of ischemic syndromes in the foregut and intestines. The goal of this review is to improve the understanding and management of this life-threatening disorder. -

Acute Mesenteric Ischemia Revealing Cirrhosis: About a Clinical Case
Gastroenterology & Hepatology: Open Access Case Report Open Access Acute mesenteric ischemia revealing cirrhosis: about a clinical case Abstract Volume 11 Issue 2 - 2020 Acute mesenteric ischemia (AMI) is a rare and serious medical and surgical emergency, the 1 1 2 prognosis of which depends on the early diagnosis and appropriate treatment. It is caused Kpossou AR, Sokpon CNM, Doukpo MM, 3 4 5 1 by acute or chronic interruption of splanchno-mesenteric blood flow. This interruption may Gandji EW, Diallo K, Laleye C, Vignon RK, be due to embolism, thrombosis or intestinal hypoperfusion. We report a case of acute Eyisse-Kpossou YOT,5 Sehonou J1 mesenteric ischemia in a young subject in a National Hospital and University Center of 1Departement of Hepato-gastroenterology, National and Benin. He was a 23-year-old man with no history of admitting a diffuse abdominal pain, University Hospital Hubert Koutoukou Maga (CNHU-HKM), excruciating, sudden onset of torsion and associated vomiting and stopping of materials and Benin 2 gases. Emergency laparotomy revealed acute mesenteric ischemia with ileal necrosis. Ileal Departement of Hepato-gastroenterology, National and resection with endo-ileal endo- ileal anastomosis was performed. Etiological research has University Hospital Hubert Koutoukou Maga (CNHU-HKM), Benin revealed cirrhosis of undetermined cause. The postoperative course was marked by short 3Departement of Visceral Surgery, National and University bowel syndrome and ascitic decompensation of cirrhosis. Under symptomatic treatment, Hospital -

Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S
Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S. Naval Hospital Sigonella, Sigonella, Italy DWAYNE C. CLARK, M.D., Fond du Lac Regional Clinic, Fond du Lac, Wisconsin Acute abdominal pain is a common presenting complaint in older patients. Presentation may differ from that of the younger patient and is often complicated by coexistent disease, delays in presentation, and physical and social barri- ers. The physical examination can be misleadingly benign, even with catastrophic conditions such as abdominal aortic aneurysm rupture and mesenteric ischemia. Changes that occur in the biliary system because of aging make older patients vulnerable to acute cholecystitis, the most common indication for surgery in this population. In older patients with appendicitis, the initial diagnosis is correct only one half of the time, and there are increased rates of perforation and mortality when compared with younger patients. Medication use, gallstones, and alcohol use increase the risk of pancreatitis, and advanced age is an indicator of poor prognosis for this disease. Diverticulitis is a common cause of abdominal pain in the older patient; in appropriately selected patients, it may be treated on an outpatient basis with oral antibiotics. Small and large bowel obstructions, usually caused by adhesive disease or malignancy, are more common in the aged and often require surgery. Morbidity and mortality among older patients presenting with acute abdominal pain are high, and these patients often require hospitalization with prompt surgical consultation. (Am Fam Physician 2006;74:1537-44. Copyright © 2006 American Academy of Family Physicians.) cute abdominal pain (generally sultation.2,11 In retrospective studies, more defined as pain of less than one than one half of older patients presenting week’s duration) is a common to the emergency department with acute presenting complaint among abdominal pain required hospital admission, Aolder patients. -

Portal Vein Thrombosis
Portal Vein Thrombosis a a Syed Abdul Basit, MD , Christian D. Stone, MD, MPH , b, Robert Gish, MD * KEYWORDS Thrombosis Cirrhosis Portal vein Anticoagulation Thrombophilia Thromboelastography Malignancy KEY POINTS Portal vein thrombosis (PVT) is most commonly found in cirrhosis and often diagnosed incidentally by imaging studies. There are 3 important complications of PVT: Portal hypertension with gastrointestinal bleeding, small bowel ischemia, and acute ischemic hepatitis. Acute PVT is associated with symptoms of abdominal pain and/or acute ascites, and chronic PVT is characterized by the presence of collateral veins and risk of gastrointestinal bleeding. Treatment to prevent clot extension and possibly help to recanalize the portal vein is generally recommended for PVT in the absence of contraindications for anticoagulation. PVT may obviate liver transplantation owing to a lack of adequate vasculature for organ/ vessel anastomoses. INTRODUCTION Definition Portal vein thrombosis (PVT) is defined as a partial or complete occlusion of the lumen of the portal vein or its tributaries by thrombus formation. Diagnosis of PVT is occurring more frequently, oftentimes found incidentally, owing to the increasing use of abdom- inal imaging (Doppler ultrasonography, most commonly) performed in the course of routine patient evaluations and surveillance for liver cancer. There are 3 important clinical complications of PVT: Small bowel ischemia: PVT may extend hepatofugal, causing thrombosis of the mesenteric venous arch and resultant small intestinal ischemia, which has a mortality rate as high as 50% and may require small bowel or multivisceral trans- plant if the patient survives.1 a Section of Gastroenterology and Hepatology, University of Nevada School of Medicine, 2040 West Charleston Boulevard, Suite 300, Las Vegas, NV 89102, USA; b Division of Gastroenter- ology and Hepatology, Department of Medicine, Stanford University School of Medicine, Alway Building, Room M211, 300 Pasteur Drive, MC: 5187 Stanford, CA 94305-5187, USA * Corresponding author. -

Diverticulosis, Diverticulitis, Ischaemic Colitis, Irritable Bowel Syndrome
Diverticulosis, diverticulitis, Ischemic colitis. Irritable bowel syndrome Dr. Fuszek Péter Phd. Semmelweis Egyetem Kútvölgyi Klinikai Tömb 2016-10-12 Case Riport • The 55-year-old female patient (referred by a family doctor) • History: serious illness is not known. Constipation since childhood. • Complaints: left upper quadrant abdominal pain, bloody stool, nausea, dysuria • temperature: 38,3 UH: thickened sigmoid colon • LAB: Dg: Diverticulitis • WBC: 14 Colon cancer • CRP: 15 Haemorrhoids, ? • Urine: normal Colitis Diverticulosis, diverticulitis Diverticula are small, bulging Sometimes, however, pouches that can form in large one or more of the bowel. They are found most often pouches become in the lower part of the large inflamed or infected. intestine (colon). Diverticula are That condition is common, especially after age 40, known as diverticulitis and seldom cause problems. Epidemiology The incidence of diverticular disease has increased over the past century. Autopsy studies from the early part of the 20th century reported colonic diverticula rates of 2% to 10%. This has increased dramatically over the years. More recent data suggest that up to 50% of individuals older than 60 years of age have colonic diverticula, with 10% to 25% developing complications such as diverticulitis. Hospitalizations for diverticular disease have also been on the rise. According to an American study evaluating hospitalization rates between 1998 and 2005, rates of admission for diverticular disease increased by 26% during the eight-year study period. Similar trends have been observed in Canadian and European data over the same time period . Can J Gastroenterol. 2011 Jul; 25(7): 385–389. Patogenesis Diverticula are small mucosal herniations protruding through the intestinal layers and the smooth muscle along the natural openings created by the vasa recta or nutrient vessels in the wall of the colon. -

Ischemic Colitis Complicating Major Vascular Surgery Scott R
Surg Clin N Am 87 (2007) 1099–1114 Ischemic Colitis Complicating Major Vascular Surgery Scott R. Steele, MD, FACS Department of Surgery, Madigan Army Medical Center, Fort Lewis, WA 98431, USA Ischemic colitis is a well-described complication of major vascular surgery, mostly following open abdominal aortic aneurysm (AAA) repair and endovascular aneurysm repair (EVAR), but also with aortoiliac surgery, aortic dissection, and thoracic aneurysm repair [1,2]. Although Boley and colleagues [3] described ischemia of the colon in 1963 as a revers- ible process secondary to vascular occlusion, the term was not coined until 1966, when Marston and colleagues [4] described its three stages of evolu- tion (transient ischemia, late ischemic stricture, and gangrene), along with the natural history of the disease. Furthermore, the development of colonic ischemia as a result of major vascular and aortic surgery has only been well described since the 1970s [5–9]. The original reports were scattered and mostly consisted of autopsy studies, depicting not only the high mortality associated with this condition but also, in retrospect, the relative lack of in- sight as to explanations for its onset and progression. Unfortunately, recent outcomes have not shown much improvement. Luckily, the overall inci- dence remains low, estimated at between 0.6% and 3.1%, with higher rates attributed to ruptured aneurysms, open repair, and emergent surgery [10]. Following the development of ischemic colitis, mortality has been reported to be as high as 67%, highlighting the need for rapidly identifying the com- mencement of symptoms and, perhaps more importantly, those patients at risk, in attempt to prevent its onset [10,11]. -

Bowel Obstruction As a Result of Ischemic Colitis : Review of Literature with Contribution of One Case Report
Open Access Research Journal Medical and Health Science Journal, MHSJ www.pradec.eu ISSN: 1804-1884 (Print) 1805-5014 (Online) Volume 11, 2012, pp.67-71 BOWEL OBSTRUCTION AS A RESULT OF ISCHEMIC COLITIS : REVIEW OF LITERATURE WITH CONTRIBUTION OF ONE CASE REPORT The ischemic colitis is comparatively rare disease. In most of the B. KOROUKOV 1, cases it has indistinctive clinical picture and its diagno sis requires I. TERZIEV 2, persistence in performing of the diagnostic procedures. In very R. PANDEV 1 rare cases it can manifest with some of its complications, mucous membrane hemorrhage or subileus symptoms. We present a case 1Department of Surgery of a male patient at the age of 64, who was operated on the 2 occasion of intestinal obstruction, which developed as a result of Department of General and Clinical ischemic colitis in the sigmoid colon region, complicated with Pathology University Multi-Profile stenosis. The consequent two-step surgery led to patient’s health Hospital for Active Treatment “Tsaritsa recovery in the three-year period of follow-up. Yoanna - ISUL”, Bulgaria Keywords: Bowel obstruction, ischemic colitis, diagnostics, surgical treatment. UDC: 616.34:617.55 Introduction The ischemic colitis is a disease, which is a result of acute or chronic disturbance in the blood supply of colon with consequent inflammatory changes in its wall. It was described as a term in medicine for the first time in 1960s by Boley (Boley et al., 1963) and Marston (Marston et al., 1966). Several major studies, related to the disease, found the frequency - 5-10/100 000. It is found most frequently in women and in patients above the age of 65 years (Guttormson and Bubrick, 1989; Klempnauer et al. -

Diverticular Disease-Related Colitis
Diverticular Disease-Related Colitis KEY FACTS Colon TERMINOLOGY ○ Abscess, fistula, perforation • Segmental colitis-associated diverticulosis (SCAD) ○ Exception is Crohn disease-like variant of SCAD that may show mural lymphoid aggregates ETIOLOGY/PATHOGENESIS MICROSCOPIC • Unknown, TNF-α may play role • Chronic colitis-like changes mimicking inflammatory bowel CLINICAL ISSUES disease • Presents with hematochezia, abdominal pain, diarrhea • Ulcerative colitis-like variant shows changes confined to • Median age: 64 years mucosa ○ Range: 40-86 years ○ Diverticulitis may or may not be present in these cases • Predominately involves descending and sigmoid colon (with • Crohn disease-like variant shows mural lymphoid rectal sparing) aggregates • Treatment directed toward diverticular disease suppresses • Changes in both variants confined to segment involved symptoms with diverticulosis coli MACROSCOPIC TOP DIFFERENTIAL DIAGNOSES • Mucosal changes are mild and nonspecific • Ulcerative colitis, Crohn disease, infectious colitis, diversion • Mural changes are related more to underlying diverticulosis colitis, NSAID-associated colitis coli rather than SCAD Diverticular Disease-Associated Colitis Diverticular Disease-Associated Colitis (Left) The mucosa surrounding the openings of diverticula ſt into the colonic lumen is erythematous and granular, consistent with diverticular disease-associated colitis (DDAC) . (Right) It is not uncommon to find some inflammation or erosions around the luminal opening of a colonic diverticulum ſt. To be diagnostic of DDAC, inflammation must involve the mucosa in the interdiverticular region . Chronic Active Colitis Basal Lymphoplasmacytosis (Left) A chronic colitis pattern of inflammatory infiltrate is seen in both the ulcerative colitis-like and Crohn disease- like variant of DDAC. The mucosal changes are indistinguishable from true inflammatory bowel disease (IBD). (Right) A band of lymphoplasmacytic infiltrate is present beneath the base of the crypts in the mucosa.