Portal Vein Thrombosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Abnormal Liver Chemistries
ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries Paul Y. Kwo, MD, FACG, FAASLD1, Stanley M. Cohen, MD, FACG, FAASLD2, and Joseph K. Lim, MD, FACG, FAASLD3 1Division of Gastroenterology/Hepatology, Department of Medicine, Stanford University School of Medicine, Palo Alto, California, USA; 2Digestive Health Institute, University Hospitals Cleveland Medical Center and Division of Gastroenterology and Liver Disease, Department of Medicine, Case Western Reserve University School of Medicine, Cleveland, Ohio, USA; 3Yale Viral Hepatitis Program, Yale University School of Medicine, New Haven, Connecticut, USA. Am J Gastroenterol 2017; 112:18–35; doi:10.1038/ajg.2016.517; published online 20 December 2016 Abstract Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defined as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defined as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. -

Outcomes and Predictors of In-Hospital Mortality Among Cirrhotic
Turk J Gastroenterol 2014; 25: 707-713 Outcomes and predictors of in-hospital mortality among cirrhotic patients with non-variceal upper gastrointestinal bleeding in upper Egypt LIVER Khairy H Morsy1, Mohamed AA Ghaliony2, Hamdy S Mohammed3 1Department of Tropical Medicine and Gastroenterology, Sohag University Faculty of Medicine, Sohag, Egypt 2Department of Tropical Medicine and Gastroenterology, Assuit University Faculty of Medicine, Assuit, Egypt 3Department of Internal Medicine, Sohag University Faculty of Medicine, Sohag, Egypt ABSTRACT Background/Aims: Variceal bleeding is one of the most frequent causes of morbidity and mortality among cir- rhotic patients. Clinical endoscopic features and outcomes of cirrhotic patients with non-variceal upper gastroin- testinal bleeding (NVUGIB) have been rarely reported. Our aim is to identify treatment outcomes and predictors of in-hospital mortality among cirrhotic patients with non-variceal bleeding in Upper Egypt. Materials and Methods: A prospective study of 93 cirrhotic patients with NVUGIB who were admitted to the Original Article Tropical Medicine and Gastroenterology Department, Assiut University Hospital (Assiut, Egypt) over a one-year period (November 2011 to October 2012). Clinical features, endoscopic findings, clinical outcomes, and in-hospital mortality rates were studied. Patient mortality during hospital stay was reported. Many independent risk factors of mortality were evaluated by means of univariate and multiple logistic regression analyses. Results: Of 93 patients, 65.6% were male with a mean age of 53.3 years. The most frequent cause of bleeding was duodenal ulceration (26.9%). Endoscopic treatment was needed in 45.2% of patients, rebleeding occurred in 4.3%, and the in-hospital mortality was 14%. -

Abnormal Liver Enzymes
Jose Melendez-Rosado , MD Ali Alsaad , MBChB Fernando F. Stancampiano , MD William C. Palmer , MD 1.5 ANCC Contact Hours Abnormal Liver Enzymes ABSTRACT Abnormal liver enzymes are frequently encountered in primary care offi ces and hospitals and may be caused by a wide variety of conditions, from mild and nonspecifi c to well-defi ned and life-threatening. Terms such as “abnormal liver chemistries” or “abnormal liver enzymes,” also referred to as transaminitis, should be reserved to describe infl am- matory processes characterized by elevated alanine aminotransferase, aspartate aminotransferase, and alkaline phosphatase. Although interchangeably used with abnormal liver enzymes, abnormal liver function tests specifi cally denote a loss of synthetic functions usually evaluated by serum albumin and prothrombin time. We discuss the entities that most commonly cause abnormal liver enzymes, specifi c patterns of enzyme abnormalities, diagnostic modalities, and the clinical scenarios that warrant referral to a hepatologist. he liver is the largest solid organ in the human elevated liver function tests (LFTs), they would more body, as well as one of the most versatile. It accurately describe as liver inflammation tests. LFTs manufactures cholesterol, contributes to hor- should instead refer to serum assessments of hepatic mone production, stores glucose in the form synthetic function, such as albumin and prothrombin Tof glycogen, processes drugs prior to systemic exposure, time. Disease categories, such as viral inflammation and and aids in the digestion of food and production of injury from alcohol use, may be differentiated by fol- proteins. However, the liver is also vulnerable to injury, lowing patterns and trends of enzyme elevations. -
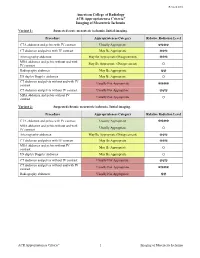
ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia
Revised 2018 American College of Radiology ACR Appropriateness Criteria® Imaging of Mesenteric Ischemia Variant 1: Suspected acute mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ MRA abdomen and pelvis without and with May Be Appropriate (Disagreement) IV contrast O Radiography abdomen May Be Appropriate ☢☢ US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ MRA abdomen and pelvis without IV Usually Not Appropriate contrast O Variant 2: Suspected chronic mesenteric ischemia. Initial imaging. Procedure Appropriateness Category Relative Radiation Level CTA abdomen and pelvis with IV contrast Usually Appropriate ☢☢☢☢ MRA abdomen and pelvis without and with Usually Appropriate IV contrast O Arteriography abdomen May Be Appropriate (Disagreement) ☢☢☢ CT abdomen and pelvis with IV contrast May Be Appropriate ☢☢☢ MRA abdomen and pelvis without IV May Be Appropriate contrast O US duplex Doppler abdomen May Be Appropriate O CT abdomen and pelvis without IV contrast Usually Not Appropriate ☢☢☢ CT abdomen and pelvis without and with IV Usually Not Appropriate contrast ☢☢☢☢ Radiography abdomen Usually Not Appropriate ☢☢ ACR Appropriateness Criteria® 1 Imaging of Mesenteric Ischemia IMAGING OF MESENTERIC ISCHEMIA Expert Panels on Vascular Imaging and Gastrointestinal Imaging: Michael Ginsburg, MDa; Piotr Obara, MDb; Drew L. Lambert, MDc; Michael Hanley, MDd; Michael L. Steigner, MDe; Marc A. Camacho, MD, MSf; Ankur Chandra, MDg; Kevin J. Chang, MDh; Kenneth L. -

Colonic Ischemia 9/21/14, 9:02 PM
Colonic ischemia 9/21/14, 9:02 PM Official reprint from UpToDate® www.uptodate.com ©2014 UpToDate® Colonic ischemia Authors Section Editors Deputy Editor Peter Grubel, MD John F Eidt, MD Kathryn A Collins, MD, PhD, FACS J Thomas Lamont, MD Joseph L Mills, Sr, MD Martin Weiser, MD All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Aug 2014. | This topic last updated: Aug 25, 2014. INTRODUCTION — Intestinal ischemia is caused by a reduction in blood flow, which can be related to acute arterial occlusion (embolic, thrombotic), venous thrombosis, or hypoperfusion of the mesenteric vasculature causing nonocclusive ischemia. Colonic ischemia is the most frequent form of intestinal ischemia, most often affecting the elderly [1]. Approximately 15 percent of patients with colonic ischemia develop gangrene, the consequences of which can be life-threatening, making rapid diagnosis and treatment imperative. The remainder develops nongangrenous ischemia, which is usually transient and resolves without sequelae [2]. However, some of these patients will have a more prolonged course or develop long-term complications, such as stricture or chronic ischemic colitis. The diagnosis and treatment of patients can be challenging since colonic ischemia often occurs in patients who are debilitated and have multiple medical problems. The clinical features, diagnosis, and treatment of ischemia affecting the colon and rectum will be reviewed here. Acute and chronic intestinal ischemia of the small intestine are discussed separately. (See "Acute mesenteric ischemia" and "Chronic mesenteric ischemia".) BLOOD SUPPLY OF THE COLON — The circulation to the large intestine and rectum is derived from the superior mesenteric artery (SMA), inferior mesenteric artery (IMA), and internal iliac arteries (figure 1). -

Original Article Clinical Features of Ischemic Hepatitis Caused by Shock with Four Different Types: a Retrospective Study of 328 Cases
Int J Clin Exp Med 2015;8(9):16670-16675 www.ijcem.com /ISSN:1940-5901/IJCEM0011996 Original Article Clinical features of ischemic hepatitis caused by shock with four different types: a retrospective study of 328 cases Gang Guo1, Xian-Zheng Wu1, Li-Jie Su1, Chang-Qing Yang2 1Department of Emergency Internal Medicine, Tongji Hospital Affiliated to Tongji University, Shanghai 200065, P.R. China; 2Department of Gastroenterology, Tongji Hospital Affiliated to Tongji University, Shanghai 200065, P.R. China Received June 27, 2015; Accepted August 11, 2015; Epub September 15, 2015; Published September 30, 2015 Abstract: The aim of the study was to investigate the clinical features of ischemic hepatitis due to shock with four dif- ferent types (allergic shock, hypovolemic shock, septic shock, and cardiogenic shock). A total of 328 patients (200 males, 128 females, mean age, 65.84 ± 15.21 years old, range, 15-94 years) diagnosed with shock in Tongji Hos- pital were retrospectively investigated from Jun 2008 to Feb 2010. The parameters of liver function test, including alanine aminotransferanse (ALT), aspartate aminotransferanse (AST), lactate dehydrogenase (LDH), total bilirubin (TB), alkaline phosphatase (ALP) and γ-glutamyltransferase (γ-GT), were recorded and analyzed. Besides, the serum levels of C-reactive protein (CRP) and brain natriuretic peptide (BNP) were also measured and relevant correlation analysis was conducted. Among all the cases, 242 (73.8%) patients developed ischemic hepatitis. The mortality of shock patients combined with ischemic hepatitis was significantly higher than the total mortality (26.0% vs 23.8%, P < 0.05). The incidence of hepatic damage was highest in the septic shock (87.5%), while the lowest in thehypo- volemic shock (49.4%). -

Liver Dysfunction in the Intensive Care Unit ANNALS of GASTROENTEROLOGY 2005, 18(1):35-4535
Liver dysfunction in the intensive care unit ANNALS OF GASTROENTEROLOGY 2005, 18(1):35-4535 Review Liver dysfunction in the intensive care unit Aspasia Soultati, S.P. Dourakis SUMMARY crosis factor-alpha, is pivotal for the development of liver injury at that stage. Liver dysfunction plays a significant role in the Intensive Care Unit (ICU) patients morbidity and mortality. Although determinations of aminotransferases, coagulation Metabolic, hemodynamic and inflammatory factors studies, glucose, lactate and bilirubin can detect hepatic contribute in liver damage. Hemorrhagic shock, septic shock, injury, they only partially reflect the underlying pathophys- multiple organ dysfunction, acute respiratory dysfunction, iological mechanisms. Both the presence and degree of jaun- metabolic disorders, myocardial dysfunction, infection from dice are associated with increased mortality in a number of hepatitis virus, and therapeutic measures such as blood non hepatic ICU diseases. transfusion, parenteral nutrition, immunosuppresion, and Therapeutic approaches to shock liver focus on the drugs are all recognised as potential clinical situations on prevention of precipitating causes. Prompt resuscitation, the grounds of which liver dysfunction develops. definitive treatment of sepsis, meticulous supportive care, The liver suffers the consequences of shock- or sepsis-in- controlling of circulation parameters and metabolism, in ducing circumstances, which alter hepatic circulation pa- addition to the cautious monitoring of therapeutic measures rameters, oxygen supply and inflammatory responses at the such as intravenous nutrition, mechanical ventilation and cellular level. Moreover, the liver is an orchestrator of met- catecholamine administration reduce the incidence and abolic arrangements which promote the clearance and pro- severity of liver dysfunction. Only precocious measures can duction of inflammatory mediators, the scavenging of bac- be taken to prevent hepatitis in ICU. -

Mesenteric Ischemia
The new england journal of medicine Review Article Edward W. Campion, M.D., Editor Mesenteric Ischemia Daniel G. Clair, M.D., and Jocelyn M. Beach, M.D. esenteric ischemia is caused by blood flow that is insuffi- From the Cleveland Clinic Lerner College cient to meet the metabolic demands of the visceral organs. The severity of Medicine of Case Western Reserve University (D.G.C.) and the Department of ischemia and the type of organ involved depend on the affected vessel of Vascular Surgery, Heart and Vascular M Institute, Cleveland Clinic (D.G.C., J.M.B.) and the extent of collateral-vessel blood flow. Despite advances in the techniques used to treat problems in the mesenteric — both in Cleveland. Address reprint re- quests to Dr. Clair at the Department of circulation, the most critical factor influencing outcomes in patients with this Vascular Surgery, Cleveland Clinic, 9500 condition continues to be the speed of diagnosis and intervention. Although mes- Euclid Ave., Desk F30, Cleveland, OH enteric ischemia is an uncommon cause of abdominal pain, accounting for less 44195, or at claird@ ccf . org. than 1 of every 1000 hospital admissions, an inaccurate or delayed diagnosis can N Engl J Med 2016;374:959-68. result in catastrophic complications; mortality among patients in whom this con- DOI: 10.1056/NEJMra1503884 Copyright © 2016 Massachusetts Medical Society. dition is acute is 60 to 80%.1-3 This article highlights the pathophysiological features, diagnosis, and treat- ment of ischemic syndromes in the foregut and intestines. The goal of this review is to improve the understanding and management of this life-threatening disorder. -

Acute Mesenteric Ischemia Revealing Cirrhosis: About a Clinical Case
Gastroenterology & Hepatology: Open Access Case Report Open Access Acute mesenteric ischemia revealing cirrhosis: about a clinical case Abstract Volume 11 Issue 2 - 2020 Acute mesenteric ischemia (AMI) is a rare and serious medical and surgical emergency, the 1 1 2 prognosis of which depends on the early diagnosis and appropriate treatment. It is caused Kpossou AR, Sokpon CNM, Doukpo MM, 3 4 5 1 by acute or chronic interruption of splanchno-mesenteric blood flow. This interruption may Gandji EW, Diallo K, Laleye C, Vignon RK, be due to embolism, thrombosis or intestinal hypoperfusion. We report a case of acute Eyisse-Kpossou YOT,5 Sehonou J1 mesenteric ischemia in a young subject in a National Hospital and University Center of 1Departement of Hepato-gastroenterology, National and Benin. He was a 23-year-old man with no history of admitting a diffuse abdominal pain, University Hospital Hubert Koutoukou Maga (CNHU-HKM), excruciating, sudden onset of torsion and associated vomiting and stopping of materials and Benin 2 gases. Emergency laparotomy revealed acute mesenteric ischemia with ileal necrosis. Ileal Departement of Hepato-gastroenterology, National and resection with endo-ileal endo- ileal anastomosis was performed. Etiological research has University Hospital Hubert Koutoukou Maga (CNHU-HKM), Benin revealed cirrhosis of undetermined cause. The postoperative course was marked by short 3Departement of Visceral Surgery, National and University bowel syndrome and ascitic decompensation of cirrhosis. Under symptomatic treatment, Hospital -

Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S
Diagnosis of Acute Abdominal Pain in Older Patients COREY LYON, LCDR, MC, USN, U.S. Naval Hospital Sigonella, Sigonella, Italy DWAYNE C. CLARK, M.D., Fond du Lac Regional Clinic, Fond du Lac, Wisconsin Acute abdominal pain is a common presenting complaint in older patients. Presentation may differ from that of the younger patient and is often complicated by coexistent disease, delays in presentation, and physical and social barri- ers. The physical examination can be misleadingly benign, even with catastrophic conditions such as abdominal aortic aneurysm rupture and mesenteric ischemia. Changes that occur in the biliary system because of aging make older patients vulnerable to acute cholecystitis, the most common indication for surgery in this population. In older patients with appendicitis, the initial diagnosis is correct only one half of the time, and there are increased rates of perforation and mortality when compared with younger patients. Medication use, gallstones, and alcohol use increase the risk of pancreatitis, and advanced age is an indicator of poor prognosis for this disease. Diverticulitis is a common cause of abdominal pain in the older patient; in appropriately selected patients, it may be treated on an outpatient basis with oral antibiotics. Small and large bowel obstructions, usually caused by adhesive disease or malignancy, are more common in the aged and often require surgery. Morbidity and mortality among older patients presenting with acute abdominal pain are high, and these patients often require hospitalization with prompt surgical consultation. (Am Fam Physician 2006;74:1537-44. Copyright © 2006 American Academy of Family Physicians.) cute abdominal pain (generally sultation.2,11 In retrospective studies, more defined as pain of less than one than one half of older patients presenting week’s duration) is a common to the emergency department with acute presenting complaint among abdominal pain required hospital admission, Aolder patients. -

A New Paradigm in Gallstones Diseases and Marked Elevation of Transaminases
A New Paradigm in Gallstones Diseases and Marked Elevation of Transaminases. , 2017; 16 (2): 285-290 285 ORIGINAL ARTICLE March-April, Vol. 16 No. 2, 2017: 285-290 The Official Journal of the Mexican Association of Hepatology, the Latin-American Association for Study of the Liver and the Canadian Association for the Study of the Liver A New Paradigm in Gallstones Diseases and Marked Elevation of Transaminases: An Observational Study Sara Campos,* Nuno Silva,** Armando Carvalho** * Gastroenterology department, Centro Hospitalar e Universitário de Coimbra (CHUC). ** Internal Medicine department, Centro Hospitalar e Universitário de Coimbra (CHUC). ABSTRACT Background. In clinical practice, it is assumed that a severe rise in transaminases is caused by ischemic, viral or toxic hepatitis. Nevertheless, cases of biliary obstruction have increasingly been associated with significant hypertransaminemia. With this study, we sought to determine the true etiology of marked rise in transaminases levels, in the context of an emergency department. Mate- rial and methods. We retrospectively identified all patients admitted to the emergency unit at Centro Hospitalar e Universitário de Coimbra between 1st January 2010 and 31st December 2010, displaying an increase of at least one of the transaminases by more than 15 times. All patient records were analyzed in order to determine the cause of hypertransaminemia. Results. We analyzed 273 patients – 146 males, mean age 65.1 ± 19.4 years. The most frequently etiology found for marked hypertransaminemia was pancreaticobiliary acute disease (n = 142;39.4%), mostly lithiasic (n = 113;79.6%), followed by malignancy (n = 74;20.6%), ischemic hepatitis (n = 61;17.0%), acute primary hepatocellular disease (n = 50;13.9%) and muscle damage (n = 23;6.4%). -

ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries
18 PRACTICE GUIDELINES CME ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries P a u l Y. K w o , M D , F A C G , F A A S L D 1 , Stanley M. Cohen , MD, FACG, FAASLD2 and Joseph K. Lim , MD, FACG, FAASLD3 Clinicians are required to assess abnormal liver chemistries on a daily basis. The most common liver chemistries ordered are serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase and bilirubin. These tests should be termed liver chemistries or liver tests. Hepatocellular injury is defi ned as disproportionate elevation of AST and ALT levels compared with alkaline phosphatase levels. Cholestatic injury is defi ned as disproportionate elevation of alkaline phosphatase level as compared with AST and ALT levels. The majority of bilirubin circulates as unconjugated bilirubin and an elevated conjugated bilirubin implies hepatocellular disease or cholestasis. Multiple studies have demonstrated that the presence of an elevated ALT has been associated with increased liver-related mortality. A true healthy normal ALT level ranges from 29 to 33 IU/l for males, 19 to 25 IU/l for females and levels above this should be assessed. The degree of elevation of ALT and or AST in the clinical setting helps guide the evaluation. The evaluation of hepatocellular injury includes testing for viral hepatitis A, B, and C, assessment for nonalcoholic fatty liver disease and alcoholic liver disease, screening for hereditary hemochromatosis, autoimmune hepatitis, Wilson’s disease, and alpha-1 antitrypsin defi ciency. In addition, a history of prescribed and over-the-counter medicines should be sought. For the evaluation of an alkaline phosphatase elevation determined to be of hepatic origin, testing for primary biliary cholangitis and primary sclerosing cholangitis should be undertaken.